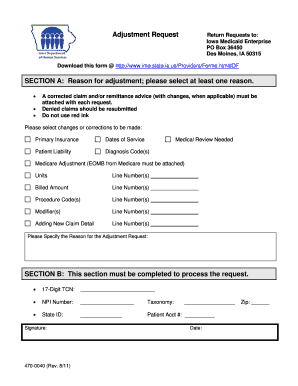
corrected claim - replacement of prior claim - UB 04
- Submit a copy of the remittance advice with the correction clearly noted.
- If necessary, attach requested documentation (e.g., nurses notes, pathology report), along with the copy of the remittance advice. ...
- Boldly and clearly mark the claim as “Corrected Claim” and attach the completed Provider Claim Inquiry Form (available at www.bcbsfl.com). ...
Full Answer
What to do if Medicare denies your medical claim?
to submit paper request or phone calls Quickest route to correct claim(s) that contained errors and faster way of receiving reimbursements 14 Part B TRU Changes Adding or changing order/referring/supervising physician Add/change rendering provider Assignment of claims (contractor errors only) CLIA certification denials
What if Medicare denies my claim?
Apr 13, 2021 · Attach a cover letter Circle or highlight any part of the claim form (for providers who are eligible to submit a paper claim form) Make any extraneous statements such as “corrected,” “second request,” etc. on the claim or documentation (this includes EDI submissions; do not add extraneous statements in the narrative)
How do I submit a corrected claim?
Once you have reviewed the narrative, press F3 one time to return to the claim. Make the correction and press F9. If the system automatically takes you back to the Claim Summary Inquiry screen (Map 1741), the claim has been corrected. You will also notice that the two- line summary for that claim no longer appears on your list of claims to correct.
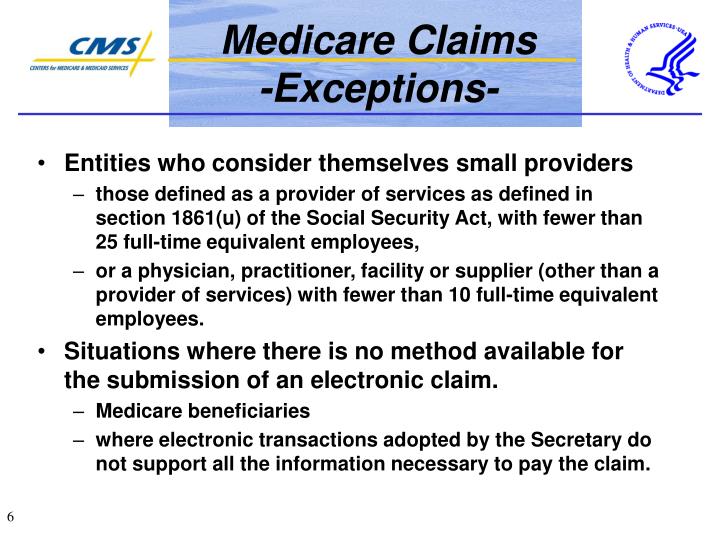
How to file your claims with Medicare?
Medicare Claims Processing Manual Chapter 34 - Reopening and Revision of Claim Determinations and Decisions (Rev. 4219, 01-25-19) Table of Contents. Transmittals for Chapter 34. 10 - Reopenings and Revisions of Claim Determinations and Decisions - General . 10.1 - Authority to Conduct a Reopening . 10.2 - Refusal to Reopen is Not an Initial ...
How do I submit a corrected claim to Medicare?
To submit a corrected claim to Medicare make the correction and resubmit as a regular claim (Claim Type is Default) and Medicare will process it.Hover over Billing and choose Live Claims Feed.Enter the patient's name or chart ID in the Patient field and click Update Filter.More items...•Jan 5, 2022
What is the resubmission code for a corrected claim for Medicare?
7Complete box 22 (Resubmission Code) to include a 7 (the "Replace" billing code) to notify us of a corrected or replacement claim, or insert an 8 (the “Void” billing code) to let us know you are voiding a previously submitted claim.Apr 8, 2015
How do I correct a Medicare billing error?
If the issue is with the hospital or a medical provider, call them and ask to speak with the person who handles insurance. They can help assist you in correcting the billing issue. Those with Original Medicare (parts A and B) can call 1-800-MEDICARE with any billing issues.Jan 6, 2022
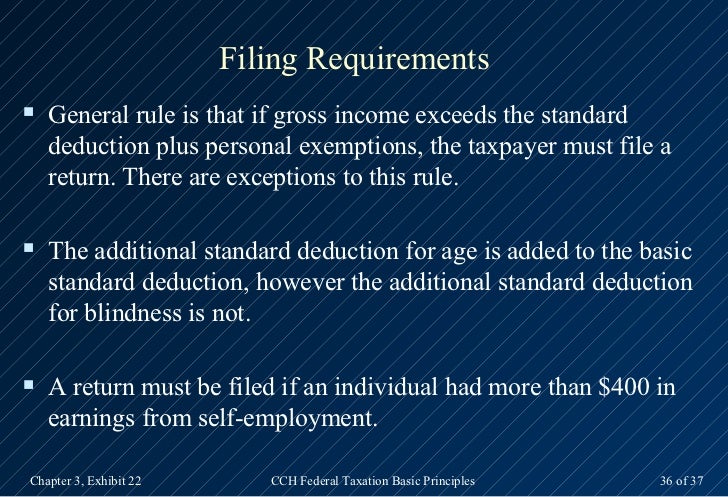
How long do you have to bill a corrected claim to Medicare?
In general, Medicare claims must be filed to the Medicare claims processing contractor no later than 12 months, or 1 calendar year, from the date the services were furnished. This includes resubmitting corrected claims that were unprocessable.Apr 13, 2021
What is the process for claim resubmission?
When you resubmit a claim, you are creating a new claim and sending it to the payer. The payer receives the claim and treats it as a new claim. To resubmit a claim, it needs to be placed back into the Bill Insurance area.Jun 20, 2018
When should I submit a corrected claim?
A corrected claim should only be submitted for a claim that has already paid, was applied to the patient's deductible/copayment or was denied by the Plan, or for which you need to correct information on the original submission.
What is the difference between a corrected claim and a replacement claim?
A corrected or replacement claim is a replacement of a previously submitted claim (e.g., changes or corrections to charges, clinical or procedure codes, dates of service, member information, etc.). The new claim will be considered as a replacement of a previously processed claim.
How do I correct a claim on Novitasphere?
Step 1: Access the Claim Correction feature on the left sidebar. Step 2: Access the claim by entering the required fields (marked by a red *) in the Claim Correction screen, and click the Search button. Step 3: Clic k the Reopen Claim for Correction button to perform a Claim Correction. See limitations to the right.
What are the five steps in the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
What is timely filing for Unitedhealthcare corrected claims?
You should submit a request for payment of Benefits within 90 days after the date of service. If you don't provide this information to us within one year of the date of service, Benefits for that health service will be denied or reduced, as determined by us.
Does Palmetto GBA accept corrected claims?
In the case where a minor error or omission is involved, you may request that Palmetto GBA reopen the claim so the error or omission can be corrected rather than going through the written appeals process. A reopening may be submitted in written form or, in some cases, over the telephone.Sep 11, 2020
What is ADR process?
The ADR process is used to notify you that a claim has been selected for medical review and is a request for you to send any medical documentation that supports the service (s) rendered and billed.
What is the redetermination process?
The redetermination process is the first level of appeal and applies to a claim or line item that receives a full or partial denial (identified as a claim in location DB9997 or a claim/line level reason code that begins with the number five or seven).
What is a redetermination in Medicare?
A redetermination is a written request, for a first level appeal, to the Medicare administrative contractor to review claim data when you are dissatisfied with the original claim determination. The redetermination is an independent process to re-evaluate the claim.
What is general inquiry?
A general inquiry is a written correspondence initiated by you that includes questions related to Medicare billing, processing or payments. There may be times that a redetermination cannot be accepted and the request will be forwarded to the general inquires department for a response to you.
Thursday, May 5, 2011
A corrected claim is a claim that has already been processed, whether paid or denied, and is resubmitted with additional charges, different procedure or diagnosis codes or any information that would change the way the claim originally processed.
corrected claim - replacement of prior claim - UB 04
A corrected claim is a claim that has already been processed, whether paid or denied, and is resubmitted with additional charges, different procedure or diagnosis codes or any information that would change the way the claim originally processed.
What is a corrected claim?
A request made from a contracting provider to change a claim, (e.g., changing information on the service line, modifier addition, diagnosis correction, etc.) that has previously processed is considered a corrected claim. The submission of a corrected claim must be received by BCBSKS within the 15-month timely filing deadline. Claims denied requesting additional information (e.g. by letter or adjustment reason code) should never be marked "corrected claim" when resubmitted. Instead, providers should submit a new claim with the requested information.
What is the purpose of a retrospective review?
The purpose of a retrospective review is to allow the provider to contact customer service to determine whether the original adjudication was correct. A.
What to do if insurance company requests refund?
If the insurance company requests a refund because of the claim correction, you can post a different accounting adjustment, such as “Insurance Take-Back” and relink the payment to that adjustment.
Do you need to unlink an adjustment?
If payments and/or adjustments have already been posted against the charges, you may need to unlink the payments and post an accounting adjustment. The insurance payer will likely ask for the money refunded back as a “take back” on future ERAs. That means that a future check, for an unrelated encounter, may be reduced for the amount of a payment sent to you in error.
Do you have to change the responsible party on a medical claim?
You may need to change the responsible party (an insurance policy, Medicaid, or personal) for some or all of the charges on a claim. You may also need to change the copay amount connected with the office visit charge.
What to do if a visit has wrong charges?
You may need to first handle any payments or adjustments attached to the charge as described above. Then you can delete the incorrect charges and post the correct charges. (As noted above, if the claim has already been sent, you’ll need to include the Payer Claim Control Number for resubmission.)
What happens after you change a visit charge?
After you make changes to a visit’s charges, such as adding a missing diagnosis code, deleting an incorrect procedure code, or changing the responsible party, you must re-batch the claim so it can be submitted . You should also record what happened in the account record.