How to enroll in a Medicare Advantage plan
- Click the Find Plans button on this page and follow the prompts to display a list of plans in your area. ...
- Arrange a time to talk with us, and we can help you enroll. Use the links below to set up a phone call.
- Call the insurance company that’s offering the plan you want.
- Call Medicare at the number below.
Full Answer
Who qualifies for a Medicare Advantage plan?
Once you understand the plan's rules and costs, here's how to join: Use Medicare's Plan Finder. Visit the plan's website to see if you can join online. Fill out a paper enrollment form. Contact the plan to get an enrollment form, fill it out, and return it to the plan. Call the plan you want to ...
How do I choose the best Medicare Advantage plan?
Apr 09, 2021 · How to enroll in a Medicare Advantage plan Click the Find Plans button on this page and follow the prompts to display a list of plans in your area. From there, you... Arrange a time to talk with us, and we can help you enroll. Use the links below to set up a phone call. Call the insurance company ...
Can anyone join a Medicare Advantage plan?
Review the enrollment period dates below and choose one the following options to get your enrollment started: 1. Online – Enrolling in a Medicare Advantage plan online is easy. Follow the prompts to enter your information and start the enrollment process now. 2. By Phone – Enrolling by phone is easy. Give us a call to get started.
How to sign up for a Medicare Advantage plan?
Mar 14, 2022 · 1. You must have Medicare Parts A and B in order to join a Medicare Advantage Plan. 2. You can enroll in a Medicare Advantage Plan (MAP) during your initial enrollment period, during open fall enrollment, or during a Special Enrollment Period, depending on your circumstances. Once you have a MAP, you can enroll in a different plan during the general …

How do I purchase a Medicare Advantage plan?
The best place to start shopping for Medicare Advantage plans (or a Part D or Medigap policy) is on the Medicare.gov comparison tool.
Are you automatically enrolled in Medicare Advantage?
A company given approval must automatically enroll all Medicare-eligible beneficiaries. But because federal law prohibits marketplace insurers from dropping a member who qualifies for Medicare, both marketplace and Medicare Advantage coverage continue until the person cancels the marketplace plan, Thorn explained.Jul 27, 2016
Can I switch from a Medicare supplement to an Advantage plan?
If you currently have Medicare, you can switch to Medicare Advantage (Part C) from Original Medicare (Parts A & B), or vice versa, during the Medicare Annual Enrollment Period. If you want to make a switch though, it may also require some additional decisions.
What are the disadvantages of a Medicare Advantage plan?
Cons of Medicare AdvantageRestrictive plans can limit covered services and medical providers.May have higher copays, deductibles and other out-of-pocket costs.Beneficiaries required to pay the Part B deductible.Costs of health care are not always apparent up front.Type of plan availability varies by region.More items...•Dec 9, 2021
Can you switch Medicare plans anytime?
If you're covered by both Medicare and Medicaid, you can switch plans at any time during the year. This applies to Medicare Advantage as well as Medicare Part D.
Which statement is true about a member of a Medicare Advantage plan who wants to enroll?
Which statement is true about members of a Medicare Advantage (MA) Plan who want to enroll in a Medicare Supplement Insurance Plan? The consumer must be in a valid MA election or disenrollment period.
Which is better a Medigap policy or Medicare Advantage plan?
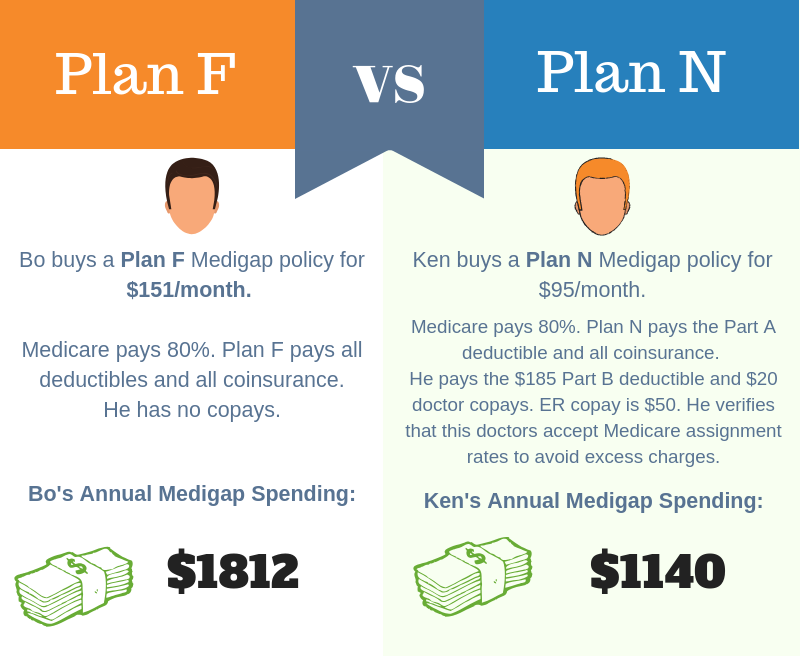
Generally, if you are in good health with few medical expenses, Medicare Advantage is a money-saving choice. But if you have serious medical conditions with expensive treatment and care costs, Medigap is generally better.
What is the difference between an Advantage plan and a supplemental plan?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.Oct 1, 2021
Why is Medicare Advantage being pushed so hard?
Advantage plans are heavily advertised because of how they are funded. These plans' premiums are low or nonexistent because Medicare pays the carrier whenever someone enrolls. It benefits insurance companies to encourage enrollment in Advantage plans because of the money they receive from Medicare.Feb 24, 2021
Is Medicare Advantage more expensive than Medicare?
Clearly, the average total premium for Medicare Advantage (including prescription coverage and Part B) is less than the average total premium for Original Medicare plus Medigap plus Part D, although this has to be considered in conjunction with the fact that an enrollee with Original Medicare + Medigap will generally ...Nov 13, 2021
Who is the largest Medicare Advantage provider?
UnitedHealthcareUnitedHealthcare is the largest provider of Medicare Advantage plans and offers plans in nearly three-quarters of U.S. counties.Dec 21, 2021
Which company has the best Medicare Advantage plan?
List of Medicare Advantage plansCategoryCompanyRatingBest overallKaiser Permanente5.0Most popularAARP/UnitedHealthcare4.2Largest networkBlue Cross Blue Shield4.1Hassle-free prescriptionsHumana4.01 more row•Feb 16, 2022
How long does it take to enroll in Medicare Advantage?
How to enroll in a Medicare Advantage plan: understand when you can sign up. Medicare Advantage plans have certain enrollment periods. When you’re first eligible for Original Medicare, Part A and Part B, you get an enrollment period called the Initial Enrollment Period (IEP). That period spans seven months. It starts three months ...
What is Medicare Advantage?
Medicare Advantage (Medicare Part C) is an optional way to receive your Original Medicare (Part A and Part B) benefits. Under Part C, these benefits are delivered to you through a private insurance company that contracts with Medicare. Many Medicare Advantage plans also include prescription drug coverage. Some people may find Medicare Advantage ...
When is the enrollment period for Medicare Part B?
Another enrollment period that comes up every year is the Fall Open Enrollment, also called the Annual Election Period. It goes from October 15 to December 7 every year. You can enroll in a Medicare Advantage plan, ...
Can I get Medicare Advantage in one plan?
Some people may find Medicare Advantage plans a convenient way to get all their Medicare coverage in one plan. Some plans may even include additional coverage, like routine dental care. When you’re enrolled in a Medicare Advantage plan, you’re still in the Medicare program.
Can I enroll in Medicare Advantage if I am 65?
Remember, you must be enrolled in Medicare Part A and Part B to be eligible for Medicare Advantage, and you have to live in the plan’s service area. If you are under 65 and have end-stage renal disease (ESRD, which is permanent kidney failure), you can generally enroll in a Medicare Advantage plan.
Annual Enrollment Period (October 15 – December 7)
The government has set a designated timeframe each year, known as Annual Enrollment Period (AEP), when individuals enrolled in a Medicare plan may change health plans or make changes to their plan types. During AEP, you may choose to keep your current coverage, or do one of the following:
Special Enrollment Periods (Timing varies based on circumstances)
In most cases, you must stay enrolled for the calendar year during which your coverage begins. However, in certain situations, you may be able to join, switch, or drop a Medicare Advantage Plan at other times. These are called Special Enrollment Periods. Some of these situations are:
Initial Coverage Enrollment Period (Applies when you are turning 65)
The Initial Coverage Enrollment Period (ICEP) is the seven-month period during which people who are newly eligible for Medicare can enroll in a Medicare Advantage plan. The ICEP begins three months before you turn 65 and ends three months after you turn 65. It also applies for individuals who may not be 65, but reach their 25th month of disability.
Medicare Advantage Open Enrollment Period (January 1 – March 31)
During this period, you can complete a one-time change to your existing Medicare Advantage plan. You can switch to another Medicare Advantage plan, this includes adding or dropping drug coverage, or disenroll from your current plan and switch to Original Medicare.
How long do you have to be on Medicare Advantage?
After that point, you have 7 full months to enroll in a Medicare Advantage Plan. Your coverage will begin on your 25th month of receiving disability benefits. If you have Amyotrophic Lateral Sclerosis (ALS), you are eligible for Medicare the first month you receive your disability benefits.
How do I sign up for Medicare Part A?
If you need to sign up for Medicare Part A and Part B, you can do so in one of four ways: Apply online on the Social Security website. Visit your local Social Security office. Call Social Security at 1-800-772-1213 (TTY: 1-800-325-0778) If you worked for a railroad, call the Railroad Retirement Board at 1-877-772-5772.
How long do you have to be on Medicare before you can get a disability?
If you become eligible for Medicare before 65 due to a qualifying disability, you may be able to enroll in a Medicare Advantage plan after you have been getting Social Security or Railroad Retirement Board benefits for 21 full months. After that point, you have 7 full months to enroll in a Medicare Advantage Plan.
How many types of Medicare Advantage Plans are there?
The availability of Medicare Advantage plans in your area will vary and is subject to how many insurance companies offer plans where you live. There are five primary types of Medicare Advantage plans that are the most prevalent, and the availability of each type of plan will also vary based on your location.
What are the factors that affect Medicare Advantage?
Several factors can affect your Medicare Advantage plan costs, such as: Whether your plan offers $0 monthly premiums. The drug deductible included in your plan, if your plan offers prescription drug coverage. Any network restrictions your plan may include regarding approved providers who are in your plan network.
What are the benefits of Medicare Advantage?
Some of the potential benefits offered by a Medicare Advantage plan can include coverage for: Dental care. Vision care.
When does Medicare AEP happen?
Medicare AEP occurs every year from October 15 to December 7. During this time, those who are already enrolled in Original Medicare can enroll in a Medicare Advantage plan. During AEP, you may also switch Medicare Advantage plans or drop your plan entirely to return to Original Medicare. YouTube. MedicareAdvantage.com.
How to switch to Medicare Advantage?
To switch to a new Medicare Advantage Plan, simply join the plan you choose during one of the enrollment periods. You'll be disenrolled automatically from your old plan when your new plan's coverage begins. To switch to Original Medicare, contact your current plan, or call us at 1-800-MEDICARE. Unless you have other drug coverage, you should ...
What happens if you lose Medicare coverage?
In other cases, you may still be able to use your employer or union coverage along with the Medicare Advantage plan you join.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
What is an HMO plan?
Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis). A network is a group of doctors, hospitals, and medical facilities that contract with a plan to provide services. Most HMOs also require you to get a referral from your primary care doctor for specialist care, so that your care is coordinated.
What is a special needs plan?
Special Needs Plan (SNP) provides benefits and services to people with specific diseases, certain health care needs, or limited incomes. SNPs tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve.
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
Can a provider bill you for PFFS?
The provider shouldn’t provide services to you except in emergencies, and you’ll need to find another provider that will accept the PFFS plan .However, if the provider chooses to treat you, then they can only bill you for plan-allowed cost sharing. They must bill the plan for your covered services. You’re only required to pay the copayment or coinsurance the plan allows for the types of services you get at the time of the service. You may have to pay an additional amount (up to 15% more) if the plan allows providers to “balance bill” (when a provider bills you for the difference between the provider’s charge and the allowed amount).