How do you file a Medicare reimbursement claim?
- Once you see the outstanding claims, first call the service provider to ask them to file the claim. If they cannot or...
- Go to Medicare.gov and download the Patient Request of Medical Payment form CMS-1490-S.
- Fill out the form by carefully following the instructions provided. Explain in detail why you are filing a claim...
Full Answer
How to get reimbursement from Medicare?
Feb 08, 2022 · How Do I File a Medicare Reimbursement Claim? To file your claim, you’ll need to fill out a Patient’s Request for Medical Payment form. You then send both this form and the bill from your provider to your state’s Medicare contractor. What the Medicare Provider Bill Must Include the date you received service the place you received service
How do I file a Medicare claim for medical treatment?
To file for a Medicare reimbursement, you must complete the following steps. Complete Medicare Form 1490 Itemize the bill from the provider Send both documents to the Medicare contractor near you The first and most important step in filing for Medicare reimbursement is to complete the Medicare Form 1490.
How do I get reimbursement for my claim?
Call 1–800 MEDICARE (1–800–633–4227; TTY users should call 1–877–486–2048). Medicare representatives are available 24 hours a day, seven days a week. If all attempts to have the doctor file the claim fail, then click here to file the Medicare claim yourself.
How do I send a claim form to a Medicare contractor?
Jul 27, 2021 · To get reimbursement, you must send in a completed claim form and an itemized bill that supports your claim. It includes detailed instructions for submitting your request. You can fill it out on your computer and print it out. You can print it and fill it out by hand.
How do I submit a bill to Medicare for reimbursement?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
Can you submit your own claims to Medicare?
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself.
Does Medicare offer reimbursement?
The Centers for Medicare & Medicaid Services (CMS) sets reimbursement rates for Medicare providers and generally pays them according to approved guidelines such as the CMS Physician Fee Schedule. There may be occasions when you need to pay for medical services at the time of service and file for reimbursement.
How do I get reimbursed for Medicare Part B?
Submit Medicare Part B premium proof of payment and a completed reimbursement form for each eligible dependent to HealthEquity in one of the following ways: Scan and upload them to healthequity.com. Fax them to 1-801-999-7829. (Be sure to include a cover sheet.)
What form is used to send claims to Medicare?
CMS-1500 claim formThe CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
Can I make a Medicare claim online?
Claim Medicare benefits online If you can't claim at the doctor's office, you can submit a Medicare claim online using either: your Medicare online account through myGov.Dec 10, 2021
How long does it take to get Medicare refund?
Once you've completed the claim process, you should receive your Medicare refund within seven days.
How much is Medicare reimbursement?
According to the Centers for Medicare & Medicaid Services (CMS), Medicare's reimbursement rate on average is roughly 80 percent of the total bill. Not all types of health care providers are reimbursed at the same rate.
What is a Medicare premium refund?
A. Refunding excess Medicare premiums. The law requires the Centers for Medicare & Medicaid Services (CMS) to dispose of excess Medicare premiums paid by, or on behalf of, a deceased beneficiary. The excess premiums may be for supplementary medical insurance (SMI) or hospital insurance (HI).May 1, 2006
How do you qualify to get 144 back from Medicare?
How do I qualify for the giveback?Be a Medicare beneficiary enrolled in Part A and Part B,Be responsible for paying the Part B premium, and.Live in a service area of a plan that has chosen to participate in this program.Nov 24, 2020
What is Medicare reimbursement?
Medicare reimbursement is the process by which a doctor or health facility receives funds for providing medical services to a Medicare beneficiary. However, Medicare enrollees may also need to file claims for reimbursement if they receive care from a provider that does not accept assignment.
What happens if a doctor doesn't accept assignment?
If you visited a doctor or provider that does not accept assignment, then you would need to file a claim for Medicare reimbursement yourself. In this scenario, the provider would still provide you the health service but is allowed to charge more. Furthermore, in most cases, you would be billed up front for the service.
How long do you have to file a Medicare claim?
All Medicare claims should be filed within 12 months of when the medical service (s) were provided. The claim must be filed within this timeframe so that Medicare can pay its share. For example, if your doctor provided service on August 1, 2018, you and your doctor have until August 1, 2019 to file the claim. Even if you have paid the doctor your portion of the costs directly, you’ll want to confirm that the doctor has submitted the claim within the allotted timeframe. Deductibles are credited only when the claimed are filed and processed.
When is the deadline to file Medicare?
The deadline for filing your Medicare claims is 12 months after the date of the provided service (s). For instance, if you received health care services on July 1, 2020, your Doctor must file the claim by July 1, 2021. Obviously, it’s better sooner than later.
Does Medicare pay for Part C?
There are no Medicare claims for Medicare Part C (Medicare Advantage) and Part D (prescription drug coverage). This is because Medicare pays your health insurance plan for Part C and Part D every month. What you will be liable for is the cost sharing (coinsurance, co-payments, and/or deductible) established by the Medicare Part C or Part D plan.
How long does it take for Medicare to process a claim?
Medicare claims to providers take about 30 days to process. The provider usually gets direct payment from Medicare. What is the Medicare Reimbursement fee schedule? The fee schedule is a list of how Medicare is going to pay doctors. The list goes over Medicare’s fee maximums for doctors, ambulance, and more.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare.
Does Medicare cover nursing home care?
Your doctors will usually bill Medicare, which covers most Part A services at 100% after you’ve met your deductible.
Does Medicare reimburse doctors?
Medicare Reimbursement for Physicians. Doctor visits fall under Part B. You may have to seek reimbursement if your doctor does not bill Medicare. When making doctors’ appointments, always ask if the doctor accepts Medicare assignment; this helps you avoid having to seek reimbursement.
Do you have to ask for reimbursement from Medicare?
If you are in a Medicare Advantage plan, you will never have to ask for reimbursement from Medicare. Medicare pays Advantage companies to handle the claims. In some cases, you may need to ask the company to reimburse you. If you see a doctor in your plan’s network, your doctor will handle the claims process.
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
What does it mean when a doctor accepts Medicare?
When your doctor accepts Medicare assignment, it also means she or he agrees not to bill you for more than the Medicare deductible and/or coinsurance. Private insurance companies contracted with Medicare may bill Medicare differently.
Can you appeal a Medicare Advantage plan?
If you have prescription drug coverage–whether it’s through a stand-alone Medicare Part D Prescription Drug Plan, or through a Medicare Advantage Prescription Drug plan–and your plan doesn’t cover a drug prescribed for you , you can file an appeal to get your plan to cover the prescription drug or to get it at a lower cost.
What does it mean when a provider refuses to file a claim for Medicare covered services?
The provider or supplier refused to file a claim for Medicare Covered Services The provider or supplier is unable to file a claim for the Medicare Covered Services The provider or supplier is not enrolled with Medicare
How long does it take for Medicare to process an itemized bill?
itemized bill and any supporting documents. Make a copy of your claim submission for your records and allow at least 60 days for Medicare to receive and process your request.
Can DMEPOS be submitted to Medicare?
In most situations, your supplier of DMEPOS will submit your claim to Medicare , if they do not, you can submit a claim for an item or services furnished by this supplier.
What is the authority to collect Medicare information?
We are authorized by the Centers for Medicare & Medicaid Services to ask you for information needed in the administration of the Medicare program. Authority to collect information is in section 205(a), 1872 and 1875 of the Social Security Act, as amended.
How long does Medicare pay for a ship?
Medicare may pay for medically necessary services furnished on a ship in a U.S. port or within 6 hours of when the ship arrived at or departed from a U.S. port only if all of the following requirements are met:

When Do I Need to File A Claim?
- You should only need to file a claim in very rare cases
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicar…
What Do I Submit with The Claim?
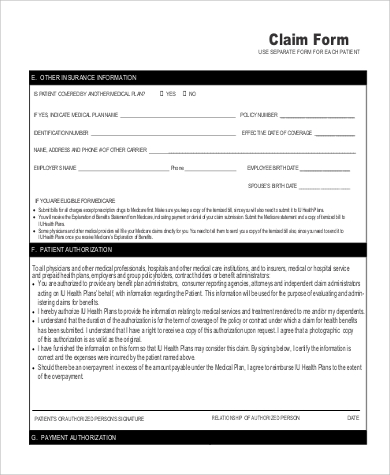
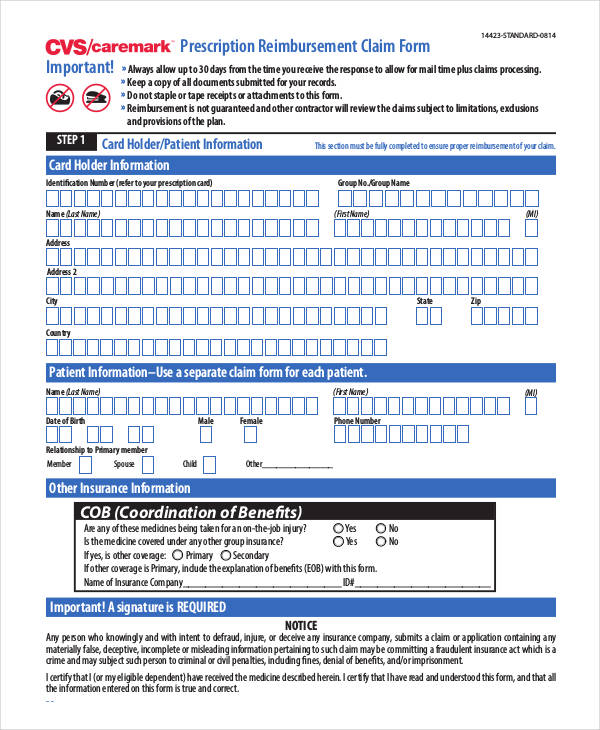
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them anytime. You need to fill out an "Author…