- Sign in to Availity Essentials ( registration required , PDF (opens in new window) )
- Use the Claim Status tool to locate the claim you want to appeal or dispute, then click the “Dispute Claim” button on the claim details screen. ...
- You can submit the appeal or dispute to Humana immediately or wait until later and submit it from your Appeals worklist.
- To access your Appeals worklist at any time, go to “Claims & Payments,” then click “Appeals.”
Full Answer
Does Humana accept electronic corrected claims?
Humana – CareSource rejects both EDI and paper form corrected claims that are received without the original claim number. Similarly, you may ask, how do you bill a corrected claim?
How to refund Humana overpayments?
Overpayment Refund/Notification Form. Please complete this form and include it with your refund so that we can properly apply the check and record the receipt. If a check is included with this correspondence, please make it payable to UnitedHealthcare and submit it with any supporting documentation. REFUNDINFORMATION
How do I submit a corrected claim?
A corrected claim should be submitted as an electronic replacement claim or on a paper claim form along with a Corrected Claim Review Form (available on the provider tab of the plan’s website). The corrected claim should include all line items previously processed correctly. Reimbursement for line items no longer included on the corrected ...
How do I file an appeal with Humana?
To File a Medical Necessity Appeal:
- Send a letter to your contractor's address.
- Include a copy of the EOB or other decision.
- Include any supporting documents.
- If you don't have all the supporting documents, send the appeal with what you have.
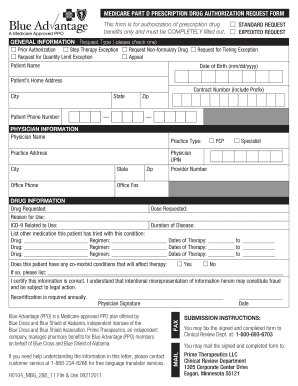
How do I submit a corrected claim to Humana Medicare?
You can submit the request online via Availity Essentials or mail it to: Humana Inc....Medicare Advantage plans: appeals for nonparticipating providersA copy of the original claim.The remittance notification showing the denial.Any clinical records and other documentation that support your case for reimbursement.
How long do you have to submit a corrected claim to Humana Medicare?
claims have to be submitted within 12 months of when you received care.
Does Humana follow Medicare billing guidelines?
Humana is excited to announce that we recognize the new coding and guidelines for our Medicare Advantage, commercial and select Medicaid plans. When the AMA and CMS differ in their coding and guidelines, Humana plans follow the CMS guidance.
How can I contact Humana?
(844) 330-7799Humana / Customer service
What are claim edits?
Claims editing is a step in the claims payment cycle that involves verifying that physician-submitted bills are coded correctly. While claims-transaction systems have some native editing and duplicate checking abilities, these systems are designed to adjudicate claims.
Does Humana accept modifier 59?
1, 2020. Humana's policy is consistent with the CMS changes. The Humana decision significantly reduces the instances in which a PT will need to append the 59, X, XE, XP, XS, or XU modifiers and will eliminate situations in which certain code pairs were prohibited.
What is a modifier 97?
Modifier 97- Rehabilitative Services: When a service or procedure that may be either habilitative or rehabilitative in nature is provided for rehabilitative purposes, the physician or other qualified healthcare professional may add modifier 97- to the service or procedure code to indicate that the service or procedure ...
What is modifier 25 in CPT coding?
Modifier 25 is used to facilitate billing of E/M services on the day of a procedure for which separate payment may be made. It is used to report a significant, separately identifiable E/M service by the same physician on the day of a procedure.
How do I bill my Humana insurance?
Other ways to pay your plan premium Be sure to write your billing ID, found on the coupon or billing-related letter from Humana, on your payment. Call our Customer Care department at the number listed on the back of your Humana member ID card to make a payment or sign up for auto pay.
Can you email Humana?
Please promptly update your service address and other contact information (address, phone/fax numbers, etc.) when changes occur. To do so, you may send an email to [email protected] with your updated contact information.
How do I call Medicare?
(800) 633-4227Centers for Medicare & Medicaid Services / Customer service
Can you have Medicare and Humana at the same time?
People eligible for Medicare can get coverage through the federal government or through a private health insurance company like Humana. Like Medicaid, every Medicare plan is required by law to give the same basic benefits.
Information for participating providers
Participating providers may find the reconsideration processes in the provider manuals for physicians, hospitals and healthcare providers.
Information for nonparticipating providers
In order to request an appeal of a denied claim, you need to submit your request in writing within 60 calendar days from the date of the denial. This request should include:
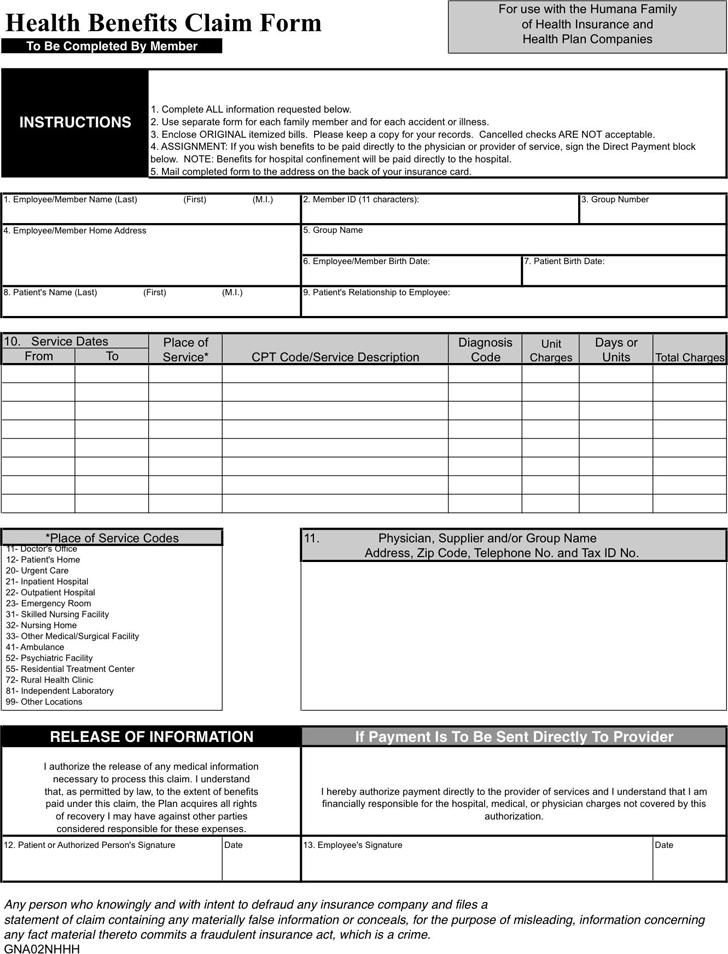
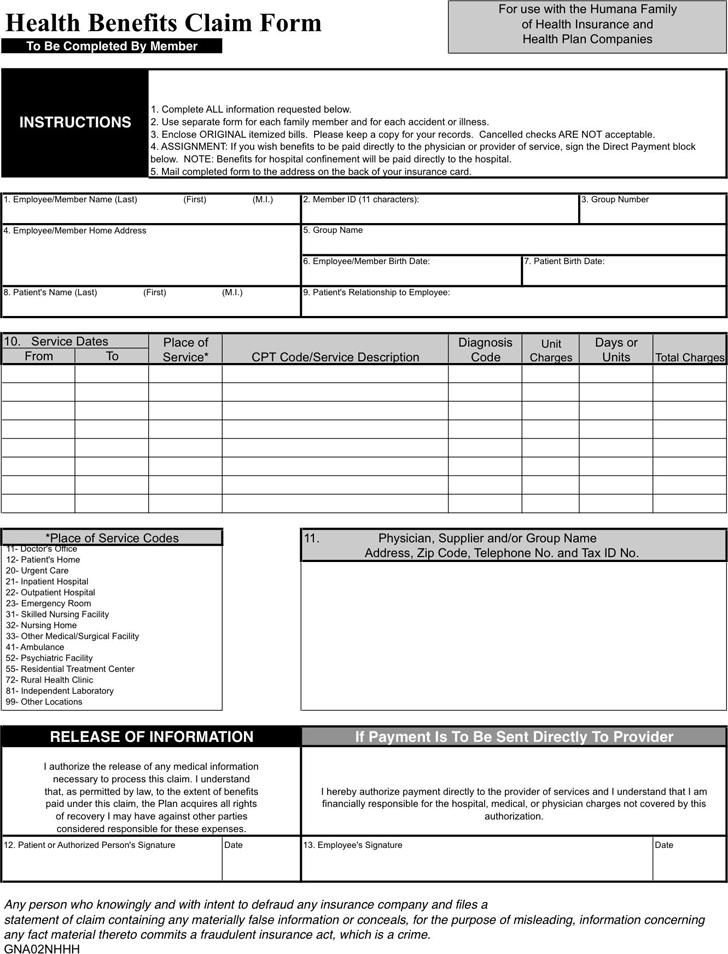
How to file a medical claim?
Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1 The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2 The itemized bill from your doctor, supplier, or other health care provider 3 A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare 4 Any supporting documents related to your claim
What to call if you don't file a Medicare claim?
If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227) . TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and your doctor or supplier still hasn't filed the claim, you should file the claim.
How long does it take for Medicare to pay?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
What happens after you pay a deductible?
After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). , the law requires doctors and suppliers to file Medicare. claim. A request for payment that you submit to Medicare or other health insurance when you get items and services that you think are covered.
When do you have to file Medicare claim for 2020?
For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020. Check the "Medicare Summary Notice" (MSN) you get in the mail every 3 months, or log into your secure Medicare account to make sure claims are being filed in a timely way.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. , these plans don’t have to file claims because Medicare pays these private insurance companies a set amount each month.
Do you have to file a claim with Medicare Advantage?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. , these plans don’t have to file claims because Medicare pays these private insurance companies a set amount each month.
How to contact Humana insurance?
Apply for coverage by phone: Call 1-877-748-7896 if you’d like to learn more about Humana health care plans or apply for coverage.
What is Humana Health Savings Account?
Health Savings Account Plans: The Humana Health Savings Account Plan works like a traditional health care plan, but the policy holder reserves the right to place money in a Health Savings Account to pay for deductibles, co-pays and other medical expenses.
Does Humana pay monthly?
If your plan supplements Medicare or you’ve purchased an individual plan from Humana One, you will need to make regular premium payments. Billing statements are typically sent monthly.
Does Humana cover prescriptions?
Prescription coverage is included in all co-pay plans. 100% After Deductible Plans: After you meet your deductible, Humana pays 100% of your healthcare costs (subject to the terms and conditions of the health care plan.)
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
Claims processing edits
We regularly update our claim payment system to better align with American Medical Association Current Procedural Terminology (CPT ® ), Healthcare Common Procedure Coding System (HCPCS) and International Classification of Diseases (ICD) code sets.
Find it fast
You can enter a keyword or keywords in the search box below to search for notifications about a topic. The more specific you are, the more pertinent your results will be.
Notifications for the Puerto Rico market
For notifications that impact the Puerto Rico market, select display edits for the Puerto Rico market only. These notifications are displayed in Spanish.
Reminders and special announcements
Please review the “General reminders and special announcements” page for important information that applies to all code editing and claim submissions.
When can I appeal an unfavorable Part C coverage determination?
If you have received an unfavorable Part C determination, you can ask for a reconsideration (appeal) by following the instructions given in the determination or as outlined below. Reconsiderations can be requested on any adverse determination.
Can I file an expedited appeal on an adverse initial determination?
An expedited appeal can be requested if you believe that waiting for a decision under the standard time frame could seriously jeopardize the life or health of the member, or the ability to regain maximum function. Refer to the Expedited appeal section.
Who can submit the Part C reconsideration (appeal) request?
You (member), a person you appoint, or your physician. Refer to the How to appoint a representative section for additional information.
When Do I Need to File A Claim?
- You should only need to file a claim in very rare cases
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicar… - If your claims aren't being filed in a timely way:
1. Contact your doctor or supplier, and ask them to file a claim. 2. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and yo…
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them anytime. You need to fill out an "Author…