Does Medicare cover enteral nutrition therapy (tube feeding)?
Your costs in Original Medicare. You pay 20% of the. Medicare-Approved Amount. . Medicare will only cover your enteral infusion pump if your doctor or supplier is enrolled in Medicare. If a supplier doesn't accept. assignment. , Medicare doesn't limit how much the supplier can charge you. You may also have to pay the entire bill (your share and ...
How much does Medicare pay for enteral nutrition formulas?
Medicare covers enteral nutrition therapy, commonly called tube feeding, for beneficiaries who cannot swallow due to a permanent medical problem or an impairment of long and indefinite duration. Medicare Part B coverage of enteral nutrition therapy is provided under the prosthetic device benefit for beneficiaries residing at home, or in a
Does Medicare cover a feeding pump?
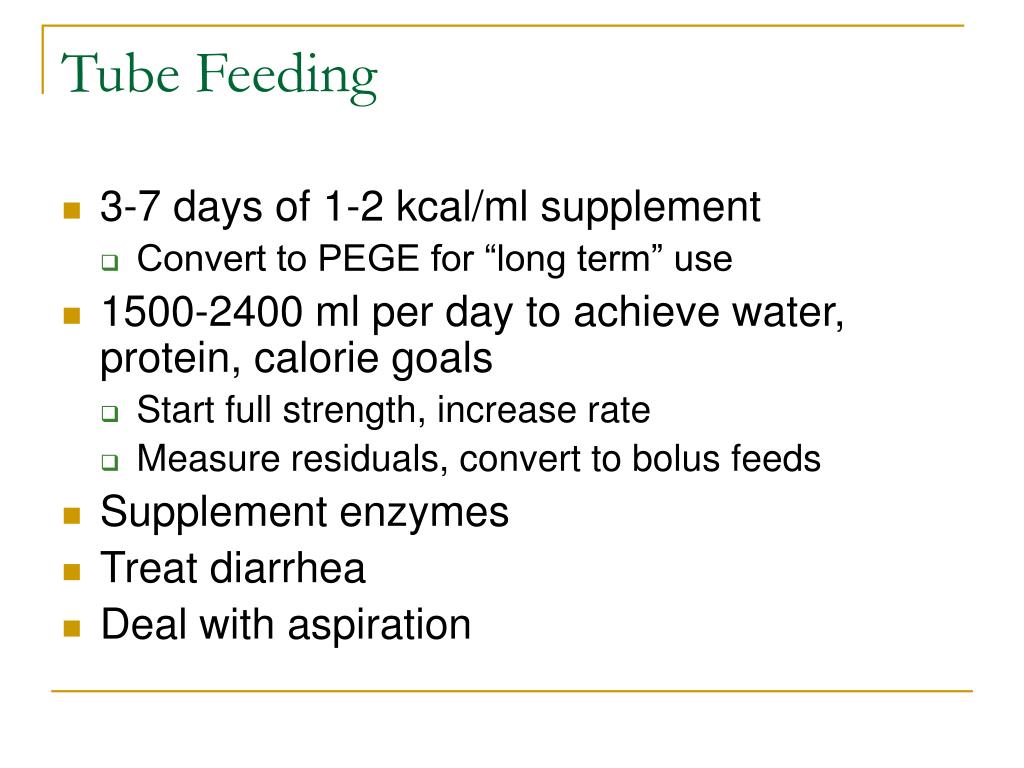
Medicare Part B Guidelines For additional information on Nestlé Health Science products, please contact your representative or call: 1-800-422-asK2 (2752) All be met to qualify for standard tube feeding reimbursement:* • Diagnosis reflecting a functional impairment •Tube feeding is required to “provide sufficient nutrients to maintain weight
How does Medicare classify eneral nutrition products?
Apr 06, 2022 · Medicare Part B covers enteral nutrition when it is administered to patients via a feeding tube in the home. Medicare Part A covers enteral nutrition therapy administered in an inpatient hospital or skilled nursing facility.. To qualify for Medicare coverage, your need for enteral nutrition must result from a permanent injury or disability.Your medical record should …

Does Medicare cover oral enteral nutrition?
Medicare pays for no more than one month's supply of enteral nutrients at any one time. If the claim involves a pump, it must be supported by sufficient medical documentation to establish that the pump is medically necessary, i.e., gravity feeding is not satisfactory due to aspiration, diarrhea, dumping syndrome.
Does Medicare pay for feeding tube food?
Both Medicare and other-payers routinely cover enteral nutrition therapy when the patient requires tube feeding, when enteral nutrition is the patient's exclusive source of nutrition, and if the patient has an anatomical or physiological malfunction of the gastrointestinal tract.
Is TPN covered by Medicare?
Medicare coverage: Medicare covers TPN both at home and in the hospital. When TPN is administered in the hospital, payment for it is included in the diagnosis-related group (DRG) payment.
Does Medicare pay for nutritional supplements?
Generally, Medicare doesn't cover nutritional supplements or vitamins except in some cases. For example, if you are diagnosed with a certain condition that requires vitamins and supplements as part of your treatment. In that case, your Medicare Part B may cover the cost of the vitamins and supplements you need.
Is B4152 covered by Medicare?
Nutritional supplementation is not covered under Medicare Part B. Enteral formulas consisting of semi-synthetic intact protein/protein isolates (B4150 or B4152) are appropriate for the majority of beneficiaries requiring enteral nutrition.Sep 8, 2021
Is a feeding tube considered skilled nursing?
Skilled nursing facilities, or nursing homes, are licensed to provide nursing care to its patients, which include caring for patients with feeding tubes.
How do I bill Medicare for enteral nutrition?
CODING GUIDELINES Enteral feeding supply allowances (B4034, B4035, and B4036) include all supplies, other than the feeding tube and nutrients, required for the administration of enteral nutrients to the beneficiary for one day. Only one unit of service may be billed for any one day.Oct 8, 2020
How much does parenteral nutrition cost?
Results: The annual cost per patient for parenteral solutions was $55,193 +/- 30,596 (mean +/- SD) based on Medicare charges and for enteral tube feedings was $9605 +/- 9327.
Who qualifies for TPN?
TPN can be administered in the hospital or at home and is most often used for patients with Crohn's disease, cancer, short bowel syndrome or ischemic bowel disease. However, critically ill patients who cannot receive nutrition orally for more than four days are also candidates for TPN.Mar 17, 2021
Does Medicare cover Areds 2?
Does Medicare cover Preservision Areds 2 and how much does it cost? Medicare Part D and Medicare Advantage do not cover Preservision Areds 2.
How much does Medicare reimburse for medical nutrition therapy?
Medicare covers 3 hours of MNT the initial year of referral and up to 2 hours of MNT for subsequent years. Hours are based on calendar year and cannot be carried over from year to year. Additional coverage is available in the same calendar year with a second referral when more MNT is medically necessary.
Does Medicare cover MNT for prediabetes?
Research shows MNT is effective in reducing complications associated with certain chronic diseases like type 2 diabetes. The new legislation provides Medicare Part B coverage for MNT for: prediabetes.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
What percentage of Medicare payment does a supplier pay for assignment?
If your supplier accepts Assignment you pay 20% of the Medicare-approved amount, and the Part B Deductible applies. Medicare pays for different kinds of DME in different ways. Depending on the type of equipment:
What are the requirements for DME?
DME meets these criteria: 1 Durable (can withstand repeated use) 2 Used for a medical reason 3 Not usually useful to someone who isn't sick or injured 4 Used in your home 5 Generally has an expected lifetime of at least 3 years
What happens if you live in an area that's been declared a disaster or emergency?
If you live in an area that's been declared a disaster or emergency, the usual rules for your medical care may change for a short time. Learn more about how to replace lost or damaged equipment in a disaster or emergency .
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. you pay 20% of the. Medicare-Approved Amount.
Does Medicare cover DME equipment?
You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare.
What are the rules for Medicare?
The rules for Medicare are different than for Medicaid. The patient must have both Medicare Part A and Part B to be eligible. The patient must be tube-fed and have a diagnosis of significant impairment of the GI, or Gastro-Intestinal, tract.
What is the phone number for Finnegan Health?
Finnegan Health Services is here to answer any and all questions about Enteral and Oral Nutrition supplies. Please call us today at 501-663-6600 or email [email protected] and one of our Customer Service Representatives will be happy to help.
Does Medicaid cover tube feeding?
For an adult, Medicaid does not cover oral nutrition but instead, only covers tube feeding supplies. Tube-fed patients on Medicaid require a PA, or Prior Authorization, before being approved. Finnegan Health Services will handle all of this paperwork for you.
Does Medicaid require EPSDT?
The prescribing PCP will determine the amount of nutrition needed. If the child is drinking the formula by mouth and not by tube, Medicaid requires EPSDT, or Well-Child, visits almost annually. These visits are a general check-up by a pediatrician.
GENERAL DOCUMENTATION REQUIREMENTS
In order to justify payment for DMEPOS items, suppliers must meet the following requirements:
NUTRIENTS
Food thickeners (B4100), baby food, and other regular grocery products that can be blenderized and used with the enteral system will be denied as noncovered.
SUPPLIES
The unit of service (UOS) for the supply allowance (B4034, B4035, or B4036) is one (1) UOS per day.
DME INFORMATION FORM (DIF)
A DME Information Form (DIF) which has been completed, signed, and dated by the supplier, must be kept on file by the supplier and made available upon request.
CODING GUIDELINES
Enteral feeding supply allowances (B4034, B4035, and B4036) include all supplies, other than the feeding tube and nutrients, required for the administration of enteral nutrients to the beneficiary for one day. Only one unit of service may be billed for any one day.
