What to do if you receive a Medicare denial letter?
Dec 01, 2021 · MA Denial Notice. Medicare health plans are required to issue the Notice of Denial of Medical Coverage (or Payment), also known as the Integrated Denial Notice (IDN), upon denial, in whole or in part, of an enrollee's request for coverage and upon discontinuation or reduction of a previously authorized course of treatment. The IDN consolidates Medicare Advantage …
What is a denial of medical coverage?
Aug 20, 2020 · If an individual does not understand why they have received the Medicare denial letter, they should contact Medicare at 800-633-4227, or their Medicare Advantage or PDP plan provider to find out...
What happens when Medicare denies coverage?
Dec 10, 2021 · If an enrollee files an appeal, then the plan must deliver a detailed notice stating why services should end. The two notices used for this purpose are: An Important Message From Medicare About Your Rights (IM) Form CMS-R-193, and the. Detailed Notice of Discharge (DND) Form CMS-10066. These forms and their instructions can be accessed on the ...
What is a Medicare Part B denial notice?
After you receive your Medicare denial letter and decide to appeal it, your appeal will usually go through five steps. These include: Level 1: redetermination (appeal) from your plan. Level 2 ...
How do I get a Medicare denial letter?
When Medicare refuses to pay for a prescribed drug, an individual can request a coverage determination or an exception by completing a “Model Coverage Determination Request” form or writing a letter of explanation.Aug 20, 2020
How do I get my Medicare Summary Notice Online?
Log into (or create) your Medicare account. Select "Get your Medicare Summary Notices (MSNs) electronically" under the "My messages" section at the top of your account homepage. You'll come to the "My communication preferences" page where you can select "Yes" under "Change eMSN preference," then "Submit."
Does Medicare send an EOB?
Your Medicare drug plan will mail you an EOB each month you fill a prescription. This notice gives you a summary of your prescription drug claims and costs. Learn more about the EOB. Use Medicare's Blue Button by logging into your secure Medicare account to download and save your Part D claims information.
Who pays if Medicare denies a claim?
If Medicare refuses to pay for a service under Original fee-for-service Part A or Part B, the beneficiary should receive a denial notice. The medical provider is responsible for submitting a claim to Medicare for the medical service or procedure.
How do I download Medicare benefit statement?
With any claims that are submitted through the Medicare, DVA, PCI and PCS channels, you are able to click into the claim and print the Medicare Statement. Select the check box of the claim. Click More and select Print Medicare Statement. You will be taken to a new tab with the Medicare Statement in PDF format.Feb 23, 2022
How often do I get a Medicare Summary Notice?
every 3 monthsWhen should I get it? You'll get your MSN every 3 months if you get any services or medical supplies during that 3-month period. If you don't get any services or medical supplies during that 3-month period you won't get an MSN for that particular 3-month period.
How do I get an explanation of benefits?
After you visit your provider, you may receive an Explanations of Benefits (EOB) from your insurer. This is an overview of the total charges for your visit and how much you and your health plan will have to pay. An EOB is NOT A BILL and helps to make sure that only you and your family are using your coverage.
Can I see my Medicare EOB online?
EOBs are usually mailed once per month. Some plans give you the option of accessing your EOB online. Your EOB is a summary of the services and items you have received and how much you may owe for them.
Can providers check Medicare claims online?
Providers can submit claim status inquiries via the Medicare Administrative Contractors' provider Internet-based portals. Some providers can enter claim status queries via direct data entry screens.Dec 1, 2021
Why was my Medicare claim rejected?
We may reject claims for Medicare benefits such as: an incorrect MBS item being used. the patient having received the maximum allowable number of benefits for an MBS item. issues with patient or health professional eligibility.Dec 10, 2021
How successful are Medicare appeals?
People have a strong chance of winning their Medicare appeal. According to Center, 80 percent of Medicare Part A appeals and 92 percent of Part B appeals turn out in favor of the person appealing.Jun 20, 2013
What is the number one reason Medicare claims are rejected?
Claim rejections (which don't usually involve denial of payment) are often due to simple clerical errors, such as a patient's name being misspelled, or digits in an ID number being transposed.Feb 5, 2020
How to appeal Medicare?
Typically, an individual must provide the following information: 1 name, address, and Medicare number 2 details of the items or services, including dates and reason for the appeal 3 a statement from the service provider 4 any other helpful information
Why is Medicare denied?
Medicare’s reasons for denial can include: Medicare does not deem the service medically necessary. A person has a Medicare Advantage plan, and they used a healthcare provider outside of the plan network. The Medicare Part D prescription drug plan’s formulary does not include the medication. The beneficiary has reached the maximum number ...
What happens if Medicare does not pay for a service?
Summary. If Medicare does not agree to pay for a service or item that a person has received, they will issue a Medicare denial letter. There are many different reasons for coverage to be denied. Medicare provides coverage for many medical services to those aged 65 and over. Younger adults may also be eligible for Medicare if they have specific ...
How long does it take to appeal a Medicare denial?
If an individual has original Medicare, they have 120 days to appeal the decision starting from when they receive the initial Medicare denial letter. If Part D denies coverage, an individual has 60 days to file an appeal. For those with a Medicare Advantage plan, their insurance provider allows 60 days to appeal.
What is a non-coverage notice?
Notice of Medicare Non-Coverage (NOMNC) A Notice of Medicare Non-Coverage (NOMNC) informs an individual that Medicare is not continuing to cover care from a comprehensive outpatient rehabilitation facility (CORF), a home health agency (HHA), or skilled nursing facility (SNF). Medicare must notify someone at least two calendar days before ...
How long does it take for Medicare to redetermine a claim?
Medicare should issue a Medicare Redetermination Notice, which details their decision within 60 calendar days after receiving the appeal.
What is SNF-ABN?
A Skilled Nursing Facility Advanced Beneficiary Notice (SNF-ABN) lets a beneficiary know in advance that Medicare will not pay for a specific service or item at a skilled nursing facility (SNF). In this case, Medicare may decide that the service is not medically necessary.
What is a generic notice?
The Generic Notice (form CMS-10123) The Generic Notice (form CMS-10123), officially called the Notice of Medicare Provider Non-Coverage, is given to all Medicare beneficiaries when the provider makes the determination that the services no longer meet Medicare Coverage Criteria .
What is SNF ABN?
The traditional denial letter, or S NF Advance Beneficiary Notice (SNF ABN), is given in addition to the Generic Notice to any beneficiaries who remain in the facility in the facility receiving non covered care at the conclusion of a Medicare Part A covered stay.
What are the different types of notices?
The following model notices are available in both Microsoft Word and PDF formats in the "Downloads" section below: 1 Notice of Right to an Expedited Grievance 2 Waiver of Liability Statement 3 Notice of Appeal Status 4 Notice of Dismissal of Appeal
What is a MOON in Medicare?
Medicare Outpatient Observation Notice (MOON) Hospitals and CAHs are required to provide a MOON to Medicare beneficiaries (including Medicare Advantage health plan enrollees) informing them that they are outpatients receiving observation services and are not inpatients of a hospital or critical access hospital (CAH).
How long does a hospital have to issue a notice to enrollees?
As under original Medicare, a hospital must issue to plan enrollees, within two days of admission, a notice describing their rights in an inpatient hospital setting, including the right to an expedited Quality Improvement Organization (QIO) review at their discharge. (In most cases, a hospital also issues a follow-up copy of this notice a day or two before discharge.) If an enrollee files an appeal, then the plan must deliver a detailed notice stating why services should end. The two notices used for this purpose are:
When does a plan issue a written notice?
A plan must issue a written notice to an enrollee, an enrollee's representative, or an enrollee's physician when it denies a request for payment or services. The notice used for this purpose is the:
What is a CMS model notice?
CMS model notices contain all of the elements CMS requires for proper notification to enrollees or non-contract providers, if applicable. Plans may modify the model notices and submit them to the appropriate CMS regional office for review and approval. Plans may use these notices at their discretion.
What is a denial letter for Medicare?
Medicare denial letters notify you of services that won’t be covered for a variety of reasons. There are several different types of letters, depending on the reason for denial. Denial letters should include information about how to appeal the decision. You will receive a Medicare denial letter when Medicare denies coverage for a service or item ...
When do you get a notice of non-coverage from Medicare?
You’ll receive a Notice of Medicare Non-Coverage if Medicare stops covering care that you get from an outpatient rehabilitation facility, home health agency, or skilled nursing facility. Sometimes, Medicare may notify a medical provider who then contacts you. You must be notified at least 2 calendar days before services end.
Does Medicare cover skilled nursing?
This letter will notify you about an upcoming service or item at a skilled nursing facility that Medicare will not cover. In this case, Medicare has deemed the service not medically reasonable and necessary. The service might also be deemed custodial (not medical related), which is not covered.
What are some examples of Medicare denied services?
This notice is given when Medicare has denied services under Part B. Examples of possible denied services and items include some types of therapy, medical supplies, and laboratory tests that are not deemed medically necessary.
What is an integrated denial notice?
Notice of Denial of Medical Coverage (Integrated Denial Notice) This notice is for Medicare Advantage and Medicaid beneficiaries, which is why it’s called an Integrated Denial Notice. It may deny coverage in whole or in part or notify you that Medicare is discontinuing or reducing a previously authorized treatment course. Tip.
What happens if Medicare denies coverage?
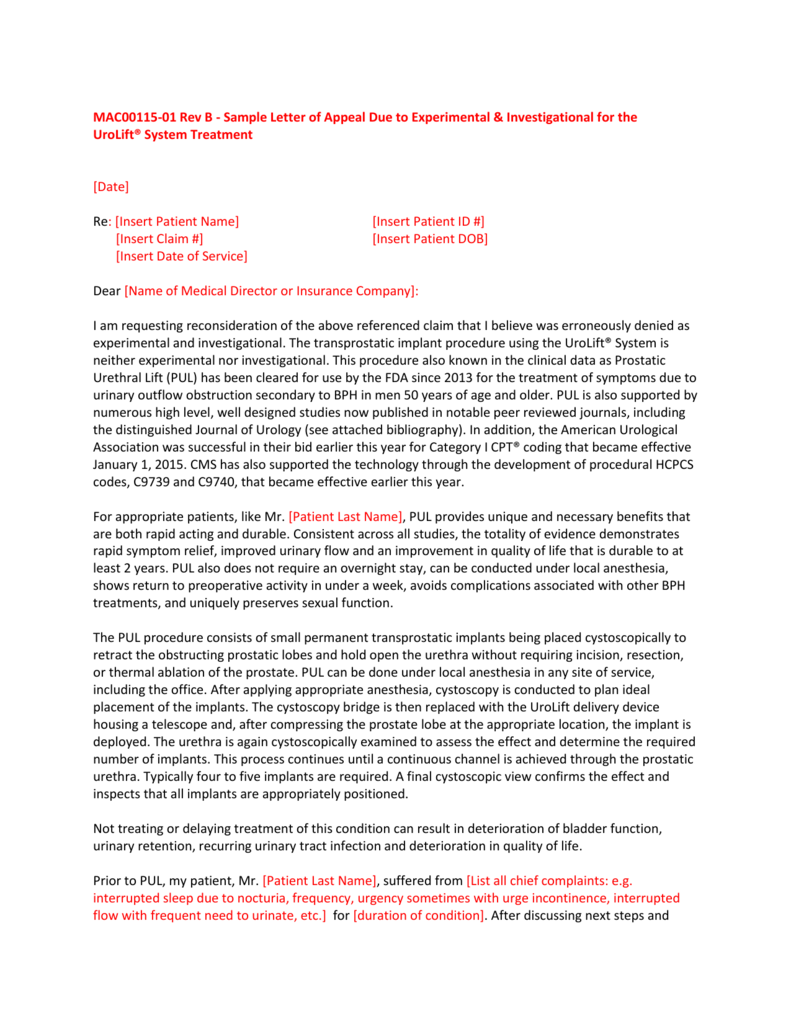
If you feel that Medicare made an error in denying coverage, you have the right to appeal the decision. Examples of when you might wish to appeal include a denied claim for a service, prescription drug, test, or procedure that you believe was medically necessary.
What is a denial letter?
A denial letter will usually include information on how to appeal a decision. Appealing the decision as quickly as possible and with as many supporting details as possible can help overturn the decision.
What is an appeal in Medicare?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: • A request for a health care service, supply, item, or drug you think Medicare should cover. • A request for payment of a health care service, supply, item, ...
How long does it take to get a decision from Medicare?
Any other information that may help your case. You’ll generally get a decision from the Medicare Administrative Contractor within 60 days after they get your request. If Medicare will cover the item (s) or service (s), it will be listed on your next MSN. Learn more about appeals in Original Medicare.
How long does it take to appeal a Medicare denial?
You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. If you miss the deadline, you must provide ...
What to do if you decide to appeal a health insurance plan?
If you decide to appeal, ask your doctor, health care provider, or supplier for any information that may help your case. See your plan materials, or contact your plan for details about your appeal rights.
How many levels of appeals are there?
The appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you'll get instructions in the decision letter on how to move to the next level of appeal.