To use this SEP you should call the Social Security Administration at 1-800-772-1213 and request two forms: the Part B enrollment request form (CMS
Centers for Medicare and Medicaid Services
The Centers for Medicare & Medicaid Services, previously known as the Health Care Financing Administration, is a federal agency within the United States Department of Health and Human Services that administers the Medicare program and works in partnership with state government…
Full Answer
What is a Medicare special enrollment period (Sep)?
· To qualify for a Medicare Special Enrollment Period, you must: Have volunteered for at least 12 months outside of the United States; Have volunteered for a tax-exempt program; Have had other health coverage for the duration that you served overseas; Medicare Special Enrollment Period for disabled TRICARE beneficiaries
When should I sign up for Medicare?
· You can sign up for Original Medicare one of four ways: Apply online on the Social Security website. Visit your local Social Security office. Call Social Security at 1-800-772-1213 (TTY: 1-800-325-0778) If you worked for a railroad, call the Railroad Retirement Board at 1-877-772-5772. Complete an ...
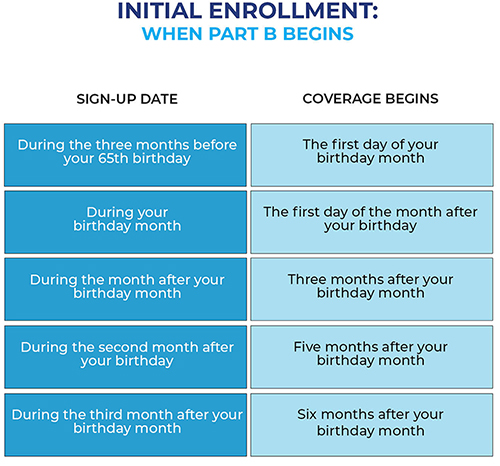
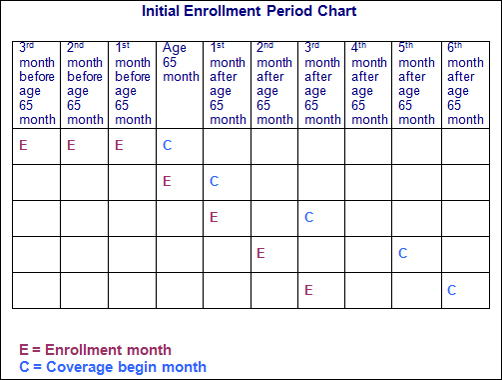
What is the initial enrollment period for Medicare?
· Special Enrollment Period (SEP) If you are age 65 or older, you or your spouse are still working and you are covered under a group health plan based on that current employment, …
What is needed to apply for Medicare?
· Enrolling in a Medicare plan during your Special Enrollment Period is easy and can be done by phone or online. To find out if you qualify, give us a call, and will help you through …
What is Medicare Sep?
You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs).
What is Medicare 8 month SEP?
What is the Medicare Part B special enrollment period (SEP)? The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse's current job. You usually have 8 months from when employment ends to enroll in Part B.
What qualifies as a life changing event for Medicare?
A change in your situation — like getting married, having a baby, or losing health coverage — that can make you eligible for a Special Enrollment Period, allowing you to enroll in health insurance outside the yearly Open Enrollment Period.
How long does it take for Medicare Part B to be approved?
You can also call the Social Security Administration at 1-800-772-1213 or go to your local Social Security office. It takes about 45 to 90 days to receive your acceptance letter after submitting your Medicare application.
What is the maximum income to qualify for Medicare?
To qualify, your monthly income cannot be higher than $1,010 for an individual or $1,355 for a married couple. Your resource limits are $7,280 for one person and $10,930 for a married couple. A Qualifying Individual (QI) policy helps pay your Medicare Part B premium.
What does Sep mean in Social Security?
Special Enrollment PeriodYou may qualify for a "Special Enrollment Period" (SEP) that will let you sign up for Part B: During any month you remain covered under the group health plan and your, or your spouse's, current employment continues; or.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
Does Social Security count towards Irmaa?
Some examples of what counts as income towards IRMAA are: Wages, Social Security benefits, Pension/Rental income, Interest, Dividends, distributions from any tax-deferred investment like a Traditional 401(k) or IRA and, again, Capital Gains.
Can you lose Medicare benefits?
Yes, if you qualify for Medicare by disability or health problem, you could lose your Medicare eligibility. If you qualify for Medicare by age, you cannot lose your Medicare eligibility.
Can you add Medicare Part B at any time?
You can sign up for Medicare Part B at any time that you have coverage through current or active employment. Or you can sign up for Medicare during the eight-month Special Enrollment Period that starts when your employer or union group coverage ends or you stop working (whichever happens first).
Are you automatically enrolled in Medicare Part B?
Medicare will enroll you in Part B automatically. Your Medicare card will be mailed to you about 3 months before your 65th birthday. If you're not getting disability benefits and Medicare when you turn 65, you'll need to call or visit your local Social Security office, or call Social Security at 1-800-772-1213.
Do you have to enroll in Medicare Part B every year?
For Original Medicare (Parts A and B), there are no renewal requirements once enrolled. Medigap plans ― also known as Medicare Supplement plans ― auto renew annually unless you make a change.
Why Would I Need A Medicare Special Enrollment period?
Medicare has limited enrollment periods for Part A and Part B. Many people are automatically enrolled when they turn 65 or qualify through disabili...
When Might I Qualify For A Medicare Special Enrollment period?
Certain situations may qualify you to enroll in Part A and/or Part B using a Medicare Special Enrollment Period. Some qualifying situations may inc...
Medicare Special Enrollment Period For The Working Aged
If you (or your spouse) are still working when you turn 65 and have group coverage through an employer or union, you can generally delay Part A and...
Medicare Special Enrollment Period For International Volunteers
Individuals volunteering in a foreign country may be able to enroll in Part A and/or Part B with a Medicare Special Enrollment Period when they ret...
Medicare Special Enrollment Period For Disabled Tricare Beneficiaries
TRICARE is health insurance for retired and active-duty service members and their families. If you’re a retired service member, you must enroll in...
Medicare Special Enrollment Period If You Were Living Overseas
There are other situations where you may be able to enroll in Medicare outside of normal enrollment periods without a Special Enrollment Period. Th...
What is a SEP in Medicare?
A Medicare Special Enrollment Period (SEP) can let you sign up for Original Medicare Part A and/or Part B outside of regular enrollment periods. If you’re not eligible for an SEP, you’ll have usually to wait until the next General Enrollment Period to sign up for Part A and/or Part B. You might also have to pay a late enrollment penalty ...
When does Medicare enroll in Part A?
Medicare has limited enrollment periods for Part A and Part B. Many people are automatically enrolled when they turn 65 or qualify through disability. Read about automatic enrollment and Medicare’s usual enrollment periods.
How long do you have to enroll in a new insurance plan?
You have eight months to enroll, beginning the month that employment or employment-based coverage ends – whichever happens first. You may not have to pay a late enrollment penalty for not enrolling when you were first eligible.
How to contact Medicare for Part B?
For more information on Part B enrollment for U.S. citizens living abroad, contact Medicare at 1-800-MEDICARE (1-800-633-4227) . If you’re a TTY user, call 1-877-486-2048. Customer service representatives can be reached 24 hours a day, seven days a week.
How many times can you use Medicare Special Enrollment?
The month that the person is notified of Part A enrollment. This Medicare Special Enrollment Period can only be used one time during the TRICARE beneficiary’s lifetime.
Does Cobra count as Medicare?
Keep in mind that COBRA and retiree health insurance don’t count as coverage based on current employment and won’t qualify you for a Medicare Special Enrollment Period when it ends. You also won’t get a Medicare Special Enrollment Period if your group coverage or employment ends during your Medicare Initial Enrollment Period.
How long do you have to enroll in Medicare if you are still working?
When that employment – or your health coverage – ends, you can typically enroll in Part A and Part B with a Medicare Special Enrollment Period. You have eight months to enroll, beginning the month that employment or employment-based coverage ends – whichever happens first. You may not have to pay a late enrollment penalty for not enrolling when you were first eligible.
What is the number to call for Medicare enrollment?
If you have a particular situation that prevented you from enrolling in any type of Medicare coverage for which you were eligible, you are encouraged to call 1-800-MEDICARE and request a Special Enrollment Period.
When is the open enrollment period for Medicare?
Learn more and use this guide to help you sign up for Medicare. Open Enrollment: The fall Medicare Open Enrollment Period has officially begun and lasts from October 15 to December 7, 2020. You may be able to enroll in ...
What to do if you don't fit into Medicare?
If your circumstances do not fit into any of the Special Enrollment Periods described above, you may ask the Centers for Medicare and Medicaid Services (CMS) for your own Special Enrollment Period based on your situation.
How many stars do you need to be to enroll in Medicare Advantage?
If you are enrolled in a Medicare Advantage plan that has received a Plan Performance Rating of three stars or less for three consecutive years, 1 you may enroll in a higher rated plan throughout the year.
How long does it take to switch to another Medicare Advantage plan?
If you permanently move out of your Medicare Advantage plan’s coverage area or move to an area with more available plans, you may switch to another Medicare Advantage plan beginning the month before your move and lasting for two months.
How often can you change your Medicare Advantage plan?
If you move into, out of, or currently reside in a facility of special care such as a skilled nursing home or long-term care hospital, you may enroll in, disenroll from, or change a Medicare Advantage plan one time per month.
How long do you have to disenroll from Medicare?
If you wish to disenroll from employer or union-sponsored coverage (including a group-sponsored Medicare Advantage plan) in order to enroll in Medicare Advantage, or you wish to disenroll from Medicare Advantage in order to join an employer or union-sponsored plan, you may do so for up to two months following the end of your previous coverage.
What is a SEP in health insurance?
You may qualify for a "Special Enrollment Period" (SEP) that will let you sign up for Part B: During any month you remain covered under the group health plan and your, or your spouse's, current employment continues; or.
How old do you have to be to get Medicare?
If you are age 65 or older, you or your spouse are still working and you are covered under a group health plan based on that current employment, you may not need to apply for Medicare medical insurance (Part B) at age 65. You may qualify for a "Special Enrollment Period" (SEP) that will let you sign up for Part B: 1 During any month you remain covered under the group health plan and your, or your spouse's, current employment continues; or 2 In the eight-month period that begins with the month after your group health plan coverage or the current employment it is based on ends, whichever comes first.#N#Exception: If your group health plan coverage or the employment it is based on ends during your initial enrollment period for Medicare Part B, you do not qualify for a SEP. Your initial enrollment period starts three months before the month you attain age 65 and ends three months after the month you turn 65. 3 If your group health plan coverage is based on severance or retirement pay and the job your coverage is based on ended in the last eight months.
Can you get a SEP if you have cobra?
If your group health plan coverage is based on severance or retirement pay and the job your coverage is based on ended in the last eight months. Note : COBRA and retiree health plans aren't considered coverage based on current employment. If you have that type of coverage, you will not be eligible for a SEP when it ends.
Can you get a SEP if you have a group health plan?
Exception: If your group health plan coverage or the employment it is based on ends during your initial enrollment period for Medicare Part B, you do not qualify for a SEP.
Do people on Social Security have a special enrollment period?
People who receive Social Security disability benefits and are covered under a group health plan from either their own or a family member's current employment also have a special enrollment period and premium rights similar to those for workers age 65 or older.
How Long Do Special Enrollment Periods Last?
The Special Enrollment Period for qualifying life events lasts for two months. But the Special Enrollment Period for working past 65 is 8 months.
Is there a SEP for Medicare Part D Plans?
During your 12 months trial right of a Medicare Advantage plan, if you choose to leave Part C, you’ll have the opportunity to enroll in a Part D plan.
Will I Qualify for a Special Election Period When Moving?
When you move to a new county or a new state, it’s possible your current plan won’t be available to you. Eligibility varies depending on your situation.
What if I Move and I have Medigap Insurance?
When you move to another state with Medigap you won’t have to change your coverage if the plan is available in your new place of residence. You’ll still want to notify Medicare and your supplement company that you moved so they can update their information.
What Happens with Part C or Part D if I move?
With Part C or Part D, if you move to a new state or region that is outside your plans service area you will be able to change your plan. You can decide if you want a switch back to Original Medicare or enroll in a similar plan.
Is there a SEP for Incarceration?
You have two months from the time you’re released from jail to use your Medicare SEP to enroll in a plan.
Will I Qualify for a Special Enrollment Period When Losing Coverage?
Losing coverage will qualify you for a Special Enrollment Period. Whether you lose employer health coverage, credible prescription drug coverage, or your plan leaves your network a SEP will be available to you.
What is Medicare SEP?
A Medicare SEP is a period of time to enroll or change a Medicare Advantage plan outside of the Initial Coverage Election Period (ICEP) or Medicare’s Annual Election Period (AEP). There are various types of SEPs that would allow you to enroll in a Medicare Advantage plan outside of these periods. 1
Who has the legal authority to establish SEPs?
CMS has the legal authority to establish SEPs when a person or group of people meet certain exceptional conditions. Some of these conditions include: 3
Why are people not eligible for SNP?
Individuals enrolled in a Special Needs Plan (SNP) who are no longer eligible for the SNP because they no longer meet the specific special needs status
Do you have to have a new Medicare plan to move?
You’ll have new Medicare health or Part D plans available due to a permanent move
Who can qualify for SEP?
A consumer may qualify for an SEP if he or she (or anyone in his or her household)
What are the qualifying events for SEP?
Consumers may qualify for an SEP to enroll in or change plans if they experience a qualifying event in one (1) of the following six (6) categories: 1. Loss of qualifying health coverage 2. Change in household size 3. Change in primary place of living 4.
What are some examples of qualifying health coverage?
Some examples of qualifying health coverage include: • Coverage through a job, or through another person’s job. – This also applies when consumers become newly eligible for help paying for coverage because their employer stops offering coverage or the coverage isn’t considered qualifying coverage. 8. 1.
Can you change your SEP plan?
Consumers who experience a qualifying event can enroll in or change plans through an SEP.
Does the SBM use HealthCare.gov?
This document generally is not intended for use in the State- based Marketplaces (SBMs) that do not use HealthCare.gov, but the material applies to you if are in a state with an SBM that is using HealthCare.gov for eligibility and enrollment. Please review the guidance on our Agents and Brokers Resources webpage (
Can a consumer qualify for SEP?
consumer may qualify for an SEP if he or she (or anyone in his or her household) has a change in his or her primary place of living and gains access to new QHPs as a result. This includes:
What is SEP in retirement?
Simplified Employee Pension (SEP) plans can provide a significant source of income at retirement by allowing employers to set aside money in retirement accounts for themselves and their employees. A SEP does not have the start-up and operating costs of a conventional retirement plan and allows for a contribution of up to 25 percent ...
What is a SEP plan?
Simplified Employee Pension Plan (SEP) A SEP plan allows employers to contribute to traditional IRAs (SEP-IRAs) set up for employees. A business of any size, even self-employed, can establish a SEP. Choose a SEP Plan.
How old do you have to be to qualify for SEP?
The eligibility requirements under the SEP are: an employee must perform service in at least three of the immediately preceding five years, reach age 21 and earn the minimum amount of compensation during the current year.
What is an eligible employee?
An eligible employee is an individual (including a self-employed individual) who meets all the following requirements:
How long can you set up a SEP?
You can set up a SEP for a year as late as the due date (including extensions) of your business income tax return for the year you want to establish the plan.
How often do you receive a statement from a SEP?
You and your employees will receive a statement from the financial institutions investing your SEP contributions both at the time you make the first SEP contributions and at least once a year after that. Each institution must provide a plain-language explanation of any fees and commissions it imposes on SEP assets withdrawn before the expiration of a specified period of time.
Who sets up SEP IRA?
A SEP-IRA must be set up by or for each eligible employee. They may be set up with banks, insurance companies or other qualified financial institutions. All SEP contributions must go to traditional IRAs. Employees are responsible for making investment decisions about their SEP-IRA accounts.
