If you apply for a Medicare Supplement
Medigap
Medigap refers to various private health insurance plans sold to supplement Medicare in the United States. Medigap insurance provides coverage for many of the co-pays and some of the co-insurance related to Medicare-covered hospital, skilled nursing facility, home health care, ambulance, durable medical equipment, and doctor charges. Medigap's name is derived from the notion that it exists to …
Full Answer
What to do during Medicare open enrollment?
• Screening for income guidelines, being mindful of programs that might help you pay for your Medicare, and helping with fraud and general complaints. • Talking to Medicare on your behalf. • Providing enrollment help when you first come onto Medicare and annually during open enrollment. • Making referrals to other agencies and programs.
What to look for with Medicare open enrollment?
Top 5 things you need to know about Medicare Enrollment
- People are eligible for Medicare for different reasons. Some are eligible when they turn 65. ...
- Some people get Medicare Part A (Hospital Insurance) and Part B (Medical Insurance) automatically and some people need to sign up for them. ...
- Enrolling in Medicare can only happen at certain times. ...
How we can help with Medicare open enrollment?
- Select a different Medicare Part C plan
- Opt-out of Medicare Part C coverage altogether
- Enroll in a different Medicare Part C Prescription Drug Plan
What do you need to know about Medicare open enrollment?
- Medicare Supplement Insurance, also known as Medigap
- Medicare Part C, also known as Medicare Advantage
- Medicare Part D, also known as Prescription Drug Plans (PDPs)
Can a Medicare Supplement plan be purchased at any time of the year?
Generally, there is no type of Medicare plan that you can get “any time.” All Medicare coverage, including Medicare Supplement (Medigap) plans, is subject to enrollment periods. Other types of Medicare plans, like Medicare Advantage and Medicare Part D prescription drug plans, have open enrollment periods every year.
How long do I have to pick a Medicare Supplement?
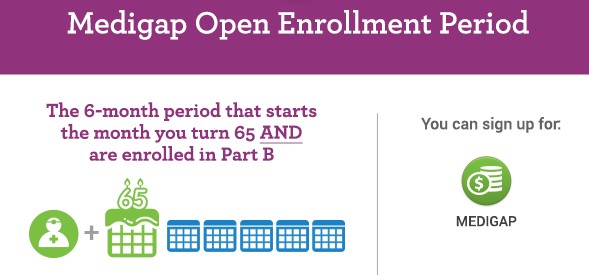
The best time to buy a Medigap policy is the 6-month period that starts the first day of the month you're 65 or older and enrolled in Part B. For example, if you turn 65 and are enrolled in Part B in June, the best time for you to buy a Medigap policy is from June to November.
Can I be denied a Medicare Supplement plan?
For the most part, Medicare Supplement policies are guaranteed renewal. This means as long as you pay the monthly premium, you cannot be denied coverage once you enroll in a plan, regardless of any health conditions that may arise.
How do I make changes to Medicare during open enrollment?
To switch to a new Medicare Advantage Plan, simply join the plan you choose during one of the enrollment periods. You'll be disenrolled automatically from your old plan when your new plan's coverage begins. To switch to Original Medicare, contact your current plan, or call us at 1-800-MEDICARE.
Can I switch from Medicare Advantage to Medicare Supplement?
Once you've left your Medicare Advantage plan and enrolled in Original Medicare, you are generally eligible to apply for a Medicare Supplement insurance plan. Note, however, that in most cases, when you switch from Medicare Advantage to Original Medicare, you lose your “guaranteed-issue” rights for Medigap.
Do Medicare Supplement plans cover pre-existing conditions?
Summary: A Medicare Supplement insurance plan may not deny coverage because of a pre-existing condition. However, a Medicare Supplement plan may deny you coverage for being under 65. A health problem you had diagnosed or treated before enrolling in a Medicare Supplement plan is a pre-existing condition.
Is Medigap plan G guaranteed issue?
Medigap Plan G is only available as a guaranteed issue plan to people who became eligible for Medicare on or after January 1st, 2020. You may still apply for Medigap Plan G through the usual methods (link to article) if you entered Medicare before 2020, but your acceptance may not be guaranteed.
Can I switch Medicare Supplement plans anytime?
As a Medicare beneficiary, you can change supplements at any time. As a result, there's no guarantee an application will be accepted if switched outside the designated Open Enrollment Period. An application may be “medically underwritten”.
Do Medigap plans have out-of-pocket limits?
Do Medigap Plans have an Out-of-Pocket Maximum? Medigap plans don't have a maximum out-of-pocket because they don't need one. The coverage is so good you'll never spend $5,000 a year on medical bills.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
Can I change my health insurance plan after enrollment?
Changing health insurance after open enrollment: Can I switch anytime? In most cases, you can only sign up for or update your health insurance during the annual Open Enrollment Period. However, if you experience certain qualifying life events, you may also become eligible for a Special Enrollment Period.
What is the difference between Medicare Advantage and Medigap?
Medigap is supplemental and helps to fill gaps by paying out-of-pocket costs associated with Original Medicare while Medicare Advantage plans stand in place of Original Medicare and generally provide additional coverage.
What is Medicare Supplement Open Enrollment Period?
What is Medicare Supplement Open Enrollment? Medicare Supplement Open Enrollment Period is a once in a lifetime window that allows you to enroll in any Medigap plan without answering health questions.
How long does Medicare open enrollment last?
Applying outside your open enrollment window can result in higher premiums, as well as restrict your coverage options. This window only lasts for six months for each new beneficiary, unless you delay enrollment into Part B due to having other creditable coverage.
What happens if you miss your Medigap open enrollment period?
When you miss your Medigap Open Enrollment Period and are denied coverage, there are alternative options. If you have a serious health condition that causes a Medigap carrier not to accept you, you should be able to enroll in a Medicare Advantage plan.
Why do people delay enrolling in Medicare Supplement?
For some; they choose to delay enrolling in Part B due to still working and having creditable coverage with their employer. When they do retire and enroll in Part B, they will initiate their Medicare Supplement Open Enrollment Period.
Does timing affect Medigap coverage?
Timing can affect how much you pay for coverage; how easy coverage is to obtain, and it can significantly determine the options available to you. The Megiap OEP is the only time you’ll ever get that allows you to enroll in any Medigap letter plan. You’ll be able to avoid having to answer any health questions.
Which states have open enrollment?
Some states have unique open enrollment rules, like Connecticut and California. In California, they have a birthday rule that allows you to enroll days surrounding your birthday without answering health questions. In Connecticut, they have a year-round open enrollment window for all beneficiaries.
Can you get insurance if you enroll in one time?
If they enroll as soon as their first eligible, during the one-time individual open enrollment window, these health problems will not prevent them from getting coverage.
How to know if you have a Medicare Supplement?
To determine whether or not you have a Medicare Supplement plan, check out your insurance card. You’ll likely see the word “Supplement,” also with a “Plan A”, “Plan G”, or another combination of “Plan” and a letter. Wisconsin, Minnesota, and Massachusetts have their own standardization method.
When does Medicare Part B open enrollment start?
Example B: You’re already 65, you sign-up for Medicare Part B and it begins June 1. This means that your Medigap Open Enrollment Period is from June 1 to November 30. If you get Medicare Part B before you turn 65, then your Open Enrollment Period starts the first day of the month you turn 65.
What happens if you miss your chance to enroll in Medicare at age 65?
If you miss your chance to enroll at age 65, then you don’t have to worry about open enrollment just yet. For example – if you’re 66 years old but have never enrolled in Medicare Part B because you are currently covered by an employer health plan – then your Medigap Open Enrollment Period has not yet occurred.
How long does the Medigap open enrollment period last?
covered under Medicare Part B. Your Medigap Open Enrollment Period then lasts for a total of six months.
What happens if you miss the open enrollment deadline?
If you miss your 6-month open enrollment deadline, many insurers will still offer you coverage. However, insurers will be free to deny your application or charge higher monthly payments. In all cases, Medicare Supplement plans are renewable for life once you’ve enrolled in the plan.
What happens if you miss your Medigap enrollment?
If you miss your Medigap Open Enrollment Period, you may be subject to medical underwriting. This means that your application could be denied by the insurance company offering the plan. Your application could also be accepted at a higher price than you were hoping to spend.
How long does Medicare cover a condition?
While your Medicare Supplement plan can’t pick and choose which health issues to cover, your plan can delay coverage for conditions that were diagnosed or treated during the six months before you enroll and for up to six months after you enroll.
What is the open enrollment period for Medicare?
Medicare Supplement Insurance (Medigap) has a six-month open enrollment period (OEP). Your open enrollment period begins when you are both: 1 65 years old and 2 Enrolled in Medicare Part B
When does Medigap OEP start?
If you get Medicare Part B before you turn 65 , your Medigap OEP starts the first day of the month you turn 65. If you delay enrolling in Medicare Part B until after you turn 65, your Medigap OEP automatically starts the month you enroll in Medicare Part B.
What are the benefits of Medigap OEP?
Benefits of buying Medigap during open enrollment. Purchasing a Medicare Supplement Insurance policy during the Medigap OEP provides several consumer protections. During the OEP, you have the following protections: Medigap insurance companies cannot deny you coverage. Insurers cannot increase premium costs because of your health when you purchase ...
How long do you have to wait to switch Medigap?
You are allowed to switch your Medigap insurance policy within your 6-month OEP. You do not have to wait for coverage to begin (although there may be a waiting period for coverage of a pre-existing condition).
Can you use medical underwriting for Medigap?
After your OEP has passed, Medigap insurance companies are usually allowed to use medical underwriting, which helps the insurer determine whether or not to accept your application and the policy’s premium. Medical underwriting is not allowed during your open enrollment period.
What is a select Medicare policy?
Medicare Select. A type of Medigap policy that may require you to use hospitals and, in some cases, doctors within its network to be eligible for full benefits. . If you buy a Medicare SELECT policy, you have rights to change your mind within 12 months and switch to a standard Medigap policy.
When to buy Medigap policy?
Buy a policy when you're first eligible. The best time to buy a Medigap policy is during your 6-month Medigap Open Enrollment Period. You generally will get better prices and more choices among policies. During that time you can buy any Medigap policy sold in your state, even if you have health problems. This period automatically starts the first ...
How long does it take for a pre-existing condition to be covered by Medicare?
Coverage for the pre-existing condition can be excluded if the condition was treated or diagnosed within 6 months before the coverage starts under the Medigap policy. After this 6-month period, the Medigap policy will cover the condition that was excluded. When you get Medicare-covered services, Original Medicare.
Can Medigap refuse to cover out-of-pocket costs?
A health problem you had before the date that new health coverage starts. . In some cases, the Medigap insurance company can refuse to cover your. out-of-pocket costs. Health or prescription drug costs that you must pay on your own because they aren’t covered by Medicare or other insurance.
Can you shorten the waiting period for a pre-existing condition?
It's possible to avoid or shorten waiting periods for a. pre-existing condition. A health problem you had before the date that new health coverage starts. if you buy a Medigap policy during your Medigap open enrollment period to replace ".
Can you get Medicare if you are 65?
Some states provide these rights to all people with Medicare under 65. Other states provide these rights only to people eligible for Medicare because of disability or only to people with ESRD. Check with your State Insurance Department about what rights you might have under state law.
Can you charge more for a Medigap policy?
Charge you more for a Medigap policy. In some cases, an insurance company must sell you a Medigap policy, even if you have health problems. You're guaranteed the right to buy a Medigap policy: When you're in your Medigap open enrollment period. If you have a guaranteed issue right.
What Is a Medicare Supplement Plan?
Medicare consists of Part A which covers hospital, skilled nursing and hospice costs, and Part B which covers medically necessary services and supplies. Part A and Part B are often referred to as Original Medicare.
Who Is Eligible To Enroll in a Medicare Supplement Plan?
To be eligible for Medigap, you must first be eligible for Original Medicare and enrolled in Part A (hospital insurance) and Part B (medical insurance).
When Is Open Enrollment for Medicare Supplement Plans?
The six-month window (which is your initial Medigap Open Enrollment Period) is the best time to buy a Medigap policy. It begins on the first day of the month in which you’re both 65 or older and enrolled in Medicare Part B. Some states have additional Open Enrollment Periods, including ones for people under 65.
What Are Guaranteed Issue Rights?
Guaranteed Issue rights refer to, “your rights to buy certain Medigap policies in certain situations outside of your Medigap Open Enrollment Period,” according to the Centers for Medicare and Medicaid Services.
Can You Enroll in Medicare Supplement Plans at Other Times?
Medicare’s open enrollment period, which is Oct. 15 through Dec.7 annually, allows you to make changes to your health and drug coverage. But 57% of Medicare enrollees don’t take advantage of the potential money-saving option to compare their Medicare coverage choices, according to data from the Kaiser Family Foundation [5].
Sources
Empowering Beneficiaries and Modernizing Medicare Enrollment. Better Medicare Alliance. Accessed 09/22/2021.