- Your doctor has ordered the scan as a medically necessary test.
- It's been 23 months since your last bone density scan or you have a condition that needs more frequent testing.
- The facility where the scan is done accepts Medicare.
How often will Medicare pay for DEXA scan?
Medicare will pay for a bone density test (DXA) as part of preventive screening every two years for women 65 or older and men 70 or older. Many insurance providers will cover the test under certain circumstances.
Does Medicare cover a DEXA scan?
Medicare Part B usually covers the costs associated with a DEXA scan. Part B is the branch of Medicare that provides coverage benefits for medically-necessary outpatient procedures to help treat an ongoing illness.
How much does it cost for a DEXA scan?
Use our DEXA Scan locator to find DEXA Scan costs in your area. It is almost always a cash pay test, not covered by insurance. The cash price for a DEXA Scan for bone density averages around $200.
How often should I have a DEXA scan?
How often should a DEXA scan be done? Medicare allows a DEXA scan to be done once every two years, and this is the current recommended timeframe. There are exceptions to this rule if you have certain diseases. Your healthcare provider will consider several factors, such as your age, level of fracture risk, previous DEXA scan and current ...

Is bone density Scan covered by Medicare?
Bone mass measurements covers this test once every 24 months (or more often if medically necessary) if you meet one of more of these conditions: You're a woman whose doctor determines you're estrogen-deficient and at risk for osteoporosis, based on your medical history and other findings.
What diagnosis code will Medicare cover for a DEXA scan?
Medicare beneficiaries who meet the above criteria may have a Diagnostic DXA once every 24 months (more often if medically necessary)....Updated DXA Policy for Medicare Patients.Z78.0Asymptomatic menopausal stateZ87.310Personal history of (healed) osteoporosis fracture4 more rows•Mar 6, 2017
What ICD-10 code covers DEXA scan for Medicare 2021?
ICD-10 CM code Z79. 83 should be reported for DXA testing while taking medicines for osteoporosis/osteopenia. ICD-10 CM code Z09 should be reported for an individual who has COMPLETED drug therapy for osteoporosis and is being monitored for response to therapy.
How do you qualify for a DEXA scan?
The National Osteoporosis Foundation recommends people at average risk get a DEXA scan starting at 65 (women) and 70 (men). Family history: If one or more family members have had osteoporosis or more than one fracture, you could be at a higher risk for bone loss.
How often should you have a bone density scan if you have osteopenia?
If you're diagnosed with osteopenia, you will need regular bone density tests to monitor bone health, usually every two to three years. Not everyone with osteopenia develops osteoporosis. Changes to your lifestyle can keep bone loss to a minimum.
What is CPT code for DEXA scan?
Group 1CodeDescription77080DUAL-ENERGY X-RAY ABSORPTIOMETRY (DXA), BONE DENSITY STUDY, 1 OR MORE SITES; AXIAL SKELETON (EG, HIPS, PELVIS, SPINE)77085DUAL-ENERGY X-RAY ABSORPTIOMETRY (DXA), BONE DENSITY STUDY, 1 OR MORE SITES; AXIAL SKELETON (EG, HIPS, PELVIS, SPINE), INCLUDING VERTEBRAL FRACTURE ASSESSMENT1 more row
At what age should you stop getting bone density tests?
The main reason to have the test is to find and treat serious bone loss. But most men, and women under age 65, probably don't need the test. Here's why: Most people do not have serious bone loss.
What ICD 10 code covers bone scan?
Encounter for screening for osteoporosis Z13. 820 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z13. 820 became effective on October 1, 2021.
What is the ICD 10 code for screening for osteoporosis?
Z13. 820 Encounter for screening for osteoporosis - ICD-10-CM Diagnosis Codes.
What is normal bone density for a 70 year old woman?
It is recommended that women < 70 years old are treated if the bone mineral density T-score is below -2.5. For women > or = 70 years of age, a lower cut-off point has been chosen, i.e. a Z-score below -1.
What is the difference between a DEXA scan and a bone density test?
A bone density test, also referred to as a DEXA scan, is a noninvasive test that measures calcium and other minerals in your bones. It measures the strength and thickness, or mass, of your bones. As we age, bones naturally become thinner. Osteopenia occurs when bones are thinner than normal.
What is a normal T-score for a 70 year old woman?
70-74 years of age the average T-score is -1.69 SD and the decrease in Z-score to those who are osteoporotic is 1.31 (Table 38).
What are the risk factors for DXA?
With any one of these factors, your insurance company should cover a DXA. 1) Early menopause (before age 40) 2) Adults with a prior low-impact fracture. 3) Adults with a disease or condition ...
Does Medicare cover bone density?
Medicare coverage. Medicare will pay for a bone density test (DXA) as part of preventive screening every two years for women 65 or older and men 70 or older. Many insurance providers will cover the test under certain circumstances.
Medicare Coverage Of Osteoporosis Medications
Many medications available today can slow the rate of bone loss and, in some cases, even rebuild bone strength.
Who Should Undergo A Bone Density Test
Postmenopausal women, men ages 70 and older, or those who recently suffered from a broken bone are advised to take a bone density test. Women are at high risk for osteoporosis. Bone loss is women is fastest during the first few years after menopause and continues into old age.
Osteoporosis And Its Complications
Osteoporosis is a medical condition characterized by architectural weakening in the bones and decreased bone mass. These changes make the bones more fragile and increase the risk of fractures, especially at the spine, hip, and wrist.
Risk Factors For Osteoporosis
When you think of osteoporosis, you likely think of women. It is true that postmenopausal women are at highest risk for the condition. Once their bodies no longer produce premenopausal levels of estrogen, the protective benefits of the hormone on their bones go away.
Does Medicare Cover Bone Density Testing
Fortunately, Medicare feels that bone health is essential and can help you get excellent bone care, whether it be testing or treatment. There are about 10 million people in the United States alone with Osteoporosis and almost 34 million more with low bone mass.
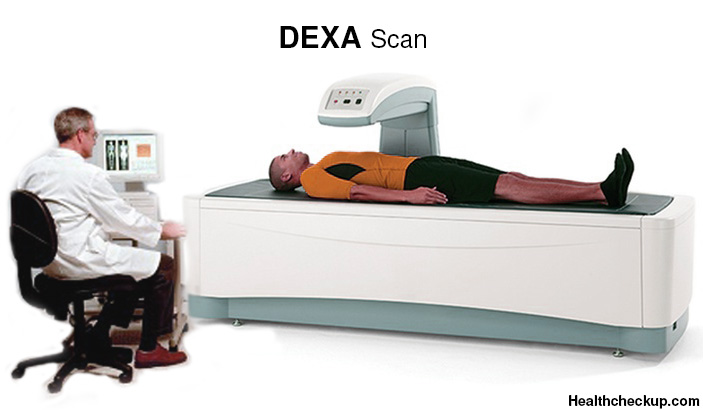
How Is Bone Density Testing Done
Bone density testing is typically done in a clinical setting such as a hospital or an outpatient facility. After putting on a loose gown, youll be asked to lie on a padded platform. A suspended mechanical arm then passes over parts of your body, taking images of your skeleton.
How To Get Help Covering The Cost Of Bone Density Testing Under Medicare
Supplemental plans fill in the gaps by covering the 20% you would otherwise pay under Part B. By relieving you of this cost, you can worry less about bills and more about recovery. The best part about a supplement is that when Medicare approves a service, the supplement must authorize the service as well.
What to expect from bone density test?
What to Expect. Bone density tests are painless and don’t require much preparation. Aside from avoiding calcium supplements 24 hours in advance, you should wear loose, comfortable clothing. Several bone density tests use ultrasound, urine tests, and X-rays or some form of radiation, such as: DXA (Dual-energy X-ray Absorptiometry)
Can you get a hyperparathyroid test with Medicare?
The test may be ordered more often if your physician deems it medically necessary. If you have Original Medicare, you will pay nothing for this test as long as your doctor accepts assignment.
How often does Medicare cover bone density?
Because certain conditions put you at a higher risk for bone problems and related injuries, Medicare covers bone density testing once every 24 months. You may qualify for more frequent testing if you have any of the following conditions, which could lead to decreased bone density: rheumatoid arthritis. chronic kidney disease.
How long has it been since your last bone density scan?
It’s been 23 months since your last bone density scan or you have a condition that needs more frequent testing. The facility where the scan is done accepts Medicare. To check whether a medical facility participates in Medicare, click here.
Do you have to have a bone density test if you have Medicare?
If you need to have a bone density test more often, your doctor will have to provide proof of a reason for more frequent testing. You may be asked to have your test done within a certain network if you have a Medicare Advantage plan. If you go outside your network, you may have to pay a share of the testing cost.
Does Medicare Advantage match Part A?
Medicare Advantage (Part C) must match the coverage of original Medicare (Part A and Part B). However, each plan may have its own requirements on where you can be tested and how much your share of the cost will be.
Can a radiology doctor perform a bone density scan?
Most outpatient facilities with radiology services can perform a bone density scan. This may be: The basic conditions for coverage are: Your doctor has ordered the scan as a medically necessary test. It’s been 23 months since your last bone density scan or you have a condition that needs more frequent testing.
What happens if the payer does not pay for the screening?
If the payer does not pay for the screening then the patient should know this prior to the test. Findings during a screening are incidental to the expectation that the patient would be as healthy as they appear. Incidental findings are always secondary dx codes.
Can you add 733.90 to a primary diagnosis?
You may add 733.90 as a secondary diagnosis, but you cannot make it your primary diagnosis. "A screening code may be a first listed code if the reason for the visit is specifically the screening exam. It may also be used as an additional code if the screening is done during an office visit for other health problems.
Can you code a diagnosis as the first listed?
You absolutely may not code the diagnosis as the first listed you must code screening first listed if the reason for the test was screening. The pate was asymptomatic if this was a screening and you cannot change the parameters of the reason for the test and "make the patient symptomatic" the findings were not expected and not wat was being investigated so the findings are incidental. I am sorry that the patient wil have to pay but they should have known that when they agreed to the screening.
Can you code a Dexa scan for osteopenia?
Click to expand... Yes. You can code it with osteopenia.
Does Medicare pay for osteopenia?
Medicare will pay the osteopenia code, but if they didn't know she had osteopenia prior to the exam being done , and if the patient did not have any of the other qualifying circumstances, then putting 733.90 as the primary diagnosis is fraud. A screening exam must have the screening diagnosis as the primary diagnosis regardless of findings.