- You present your Medicare ID card to your health care provider
- Your provider sends your claim to Medicare
- Medicare pays first and sends payment directly to the provider
- Medicare sends you a statement saying what you owe
- You pay the balance to the provider directly
How do doctors get paid by Medicare?
The specific amount you’ll owe may depend on several things, like:
- Other insurance you may have
- How much your doctor charges
- Whether your doctor accepts assignment
- The type of facility
- Where you get your test, item, or service
What does Medicare pay as the secondary payer?
The Medicare secondary payment is $100. When Medicare is the secondary payer, the combined payment made by the primary payer and Medicare on behalf of the beneficiary is $3,000. The beneficiary has no liability for Medicare-covered services since the primary payment satisfied the $520 deductible.
What kind of home care does Medicare pay for?
What types of in-home health care does Medicare cover? If your situation meets Medicare criteria, Medicare may cover in-home health care such as: Skilled nursing care (part-time or intermittent) Part-time home health aides (intermittent) Medical social services; Physical or occupational therapy; Speech language pathology; Medicare benefits might also cover:
Where can I find a doctor that accepts Medicare and Medicaid?
How to find a doctor who accepts Medicare There are a few simple ways to find a doctor who accepts your Medicare plan: Visit physician compare. The Centers for Medicare & Medicaid Services (CMS) has a tool that allows you to look up doctors near you and compare them side-by-side.
How do providers get reimbursed by Medicare?
Traditional Medicare reimbursements When an individual has traditional Medicare, they will generally never see a bill from a healthcare provider. Instead, the law states that providers must send the claim directly to Medicare. Medicare then reimburses the medical costs directly to the service provider.
Does Medicare pay doctors directly?
Rules for private contracts Medicare won't pay any amount for the services you get from this doctor or provider, even if it's a Medicare-covered service. You'll have to pay the full amount of whatever this provider charges you for the services you get.
How Does Medicare pay providers in Part B?
If the provider accepts assignment (agrees to accept Medicare's approved amount as full reimbursement), Medicare pays the Part B claim directly to him/her for 80% of the approved amount. You are responsible for the remaining 20% (this is your coinsurance ).
How is Medicare paid?
How is Medicare financed? Funding for Medicare, which totaled $888 billion in 2021, comes primarily from general revenues, payroll tax revenues, and premiums paid by beneficiaries (Figure 1). Other sources include taxes on Social Security benefits, payments from states, and interest.
Why do doctors charge more than Medicare pays?
Why is this? A: It sounds as though your doctor has stopped participating with Medicare. This means that, while she still accepts patients with Medicare coverage, she no longer is accepting “assignment,” that is, the Medicare-approved amount.
What Does Medicare pay for doctors visits?
If you see a GP Medicare will pay 100% of the cost if the GP bulk bills. If they don't bulk bill, Medicare will pay 100% of the public rate and you will have to pay any extra if the doctor charges more.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
How do providers submit claims to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
What percent of the allowable fee does Medicare pay the healthcare provider?
80 percentUnder Part B, after the annual deductible has been met, Medicare pays 80 percent of the allowed amount for covered services and supplies; the remaining 20 percent is the coinsurance payable by the enrollee.
Where does my Medicare money go?
What does it pay for?Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.benefits. The health care items or services covered under a health insurance plan. ... skilled nursing facility (snf) care. ... home health care. ... hospice.
How is Medicare funded and administered?
Medicare is federally administered and covers older or disabled Americans, while Medicaid operates at the state level and covers low-income families and some single adults. Funding for Medicare is done through payroll taxes and premiums paid by recipients. Medicaid is funded by the federal government and each state.
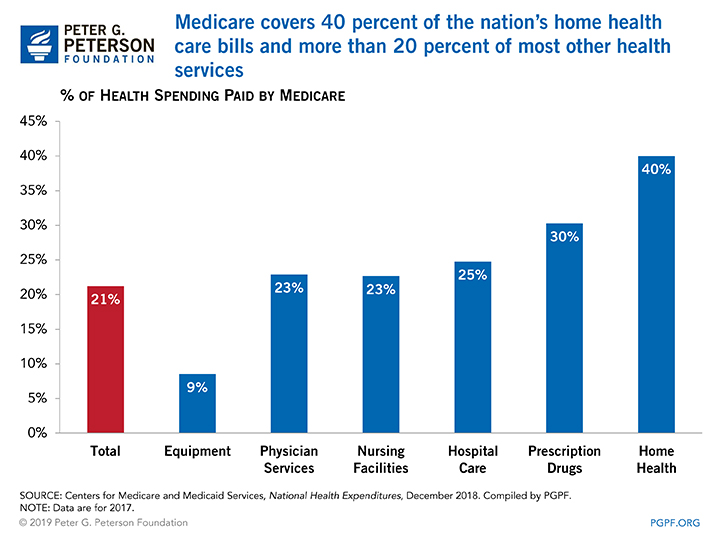
What is the largest source of payment for health care services?
Centers for Medicare and Medicaid ServicesThe Centers for Medicare and Medicaid Services is the largest governmental source of health coverage funding. Medicare is financed through a combination of general federal taxes, a mandatory payroll tax that pays for Part A (hospital insurance), and individual premiums.
What is a doctor in Medicare?
A doctor can be one of these: Doctor of Medicine (MD) Doctor of Osteopathic Medicine (DO) In some cases, a dentist, podiatrist (foot doctor), optometrist (eye doctor), or chiropractor. Medicare also covers services provided by other health care providers, like these: Physician assistants. Nurse practitioners.
What is original Medicare?
Your costs in Original Medicare. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. for most services.
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. . The Part B. deductible.
What does "covered" mean in medical terms?
medically necessary. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
How to find out how much a test is?
To find out how much your test, item, or service will cost, talk to your doctor or health care provider. The specific amount you’ll owe may depend on several things, like: 1 Other insurance you may have 2 How much your doctor charges 3 Whether your doctor accepts assignment 4 The type of facility 5 Where you get your test, item, or service
How much was Medicare reimbursement in 2015?
At the end of last year, it was reported by the American Hospital Association (AHA) that Medicaid and Medicare reimbursement in 2015 was less than the actual hospital costs for treating beneficiaries by $57.8 billion. That is billion with a “B”.
How much money do community hospitals provide?
Community hospitals provided more than $35.7 billion in uncompensated care to patients. The Centers for Medicare and Medicaid Services (CMS) does assist U.S. hospitals with additional funding. The Disproportionate Share Hospital payments help providers that treat large proportions of uninsured and Medicaid individuals.
Does Medicare cover medical expenses?
The ACA survey results showed that Medicaid and Medicare payments do not cover the amounts hospitals pay for personnel, technology, and other goods and services required to provide care to Medicare and Medicaid beneficiaries. This is critical in areas where the population is largely covered by Medicare and Medicaid.
Can hospitals participate in Medicare?
Despite low Medicaid and Medicare reimbursement rates and high uncompensated care costs, the AHA report pointed out that few hospitals can elect not to participate in federal healthcare programs. “Hospital participation in Medicare and Medicaid is voluntary,” noted the AHA.
What is a flat fee for a medical group?
When a doctor, medical group, hospital or integrated health system receives a certain flat fee every month for taking care of an individual enrolled in a managed health care plan, regardless of the cost of that individual’s care.
What is pay for performance?
A pay-for-performance model where the physician’s training, skills and time expended to provide a given service are taken into account when establishing compensation. With this model, the actual care provided by the physician is the driving force of compensation more so than the number of visits.
What is concierge medicine?
An alternative to traditional payment models, where medical practices have a direct financial relationship with patients. They typically charge a monthly or annual fee so that the patient receives additional access and personalized care. These practices are known by a variety of names: concierge healthcare, direct primary care, direct care, direct practice medicine, retainer-based, membership medicine, cash-only medicine, cash-only practice, boutique medicine, personalized healthcare.
What is bundled payment?
Bundled payments encourage value-based medicine and efficiencies required by the Affordable Care Act; however, this model also creates complexity and incentives for hospitals and practices to withhold care and procedures.
Do surgeons get a single payment?
Many surgeons will often receive a single payment for pre-op, post-op and the surgery. However, bundled payments can also be much broader, encompassing longer periods of time and multiple providers. With bundled payments, there are four models: – Retrospective Acute Care Hospital Stay Only.
How to become a Medicare provider?
Become a Medicare Provider or Supplier 1 You’re a DMEPOS supplier. DMEPOS suppliers should follow the instructions on the Enroll as a DMEPOS Supplier page. 2 You’re an institutional provider. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should use the Medicare Enrollment Guide for Institutional Providers.
How long does it take to change your Medicare billing?
To avoid having your Medicare billing privileges revoked, be sure to report the following changes within 30 days: a change in ownership. an adverse legal action. a change in practice location. You must report all other changes within 90 days. If you applied online, you can keep your information up to date in PECOS.
How to get an NPI?
If you already have an NPI, skip this step and proceed to Step 2. NPIs are issued through the National Plan & Provider Enumeration System (NPPES). You can apply for an NPI on the NPPES website.
Do you need to be accredited to participate in CMS surveys?
ii If your institution has obtained accreditation from a CMS-approved accreditation organization, you will not need to participate in State Survey Agency surveys. You must inform the State Survey Agency that your institution is accredited. Accreditation is voluntary; CMS doesn’t require it for Medicare enrollment.
Can you bill Medicare for your services?
You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify. You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify.
What is Medicare insurance?
Medicare insurance is one of the most popular options for those who qualify, and the number of people using this insurance continues to grow as life expectancy continues to increase. Medicare policies come available with many different parts, including Part A, Part B, Part C, and Part D.
When a patient uses Medicare as their primary insurance company, is the hospital required to choose appropriate and accurate diagnoses that
When a patient uses Medicare as their primary insurance company, the hospital is required to choose appropriate and accurate diagnoses that apply to the patient so that they can bill for the associated care.
How long do you have to pay coinsurance for hospital?
As far as out-of-pocket costs, you will be responsible for paying your deductible, coinsurance payments if your hospital stay is beyond 60 days, and for any care that is not deemed medically necessary. However, the remainder of the costs will be covered by your Medicare plan.
Does Medicare pay flat rate?
This type of payment system is approved by the hospitals and allows Medicare to pay a simple flat rate depending on the specific medical issues a patient presents with and the care they require. In addition, In some cases, Medicare may provide increased or decreased payment to some hospitals based on a few factors.
Does Medicare cover inpatient care?
If you receive care as an inpatient in a hospital, Medicare Part A will help to provide coverage for care. Part A Medicare coverage is responsible for all inpatient care , which may include surgeries and their recovery, hospital stays due to illness or injury, certain tests and procedures, and more. As far as out-of-pocket costs, you will be ...