Medicare will cover your enteral infusion pump from a Medicare-enrolled doctor or supplier. If a supplier doesn't accept assignment, there’s no limit on the amount they can charge you. You may also have to pay the entire bill (both your share and Medicare's share) at the time you get the pump.
Can I continue Medicare Part A for the PEG tube?
Can I continue Medicare Part A, related to the PEG tube? A: As long as 26% of the calories and 500 ml of fluid are going through the tube, it qualifies for as a skilled tube and for Medicare Part A benefits. We were unable to load Disqus.
Does Medicaid pay for feeding tube bags?
Thank you for the information! I have two reasons for asking. My son who is 18 He was a preemie with many complications and has been on a feeding tube all his life So far Medicaid has paid for all his feeding needs including the bags, tubes, etc.
How long can a tube fed patient go without Medicare reimbursement?
After the 100 days of Medicare Part A benefits are exhausted, the 60 days of wellness does not begin until the tube is no longer skilled. The fact the resident went 60 days without Medicare reimbursement does not satisfy the 60 days of wellness requirement as long as he is 100% tube fed.
Does Medicare cover tube feeding formula?
As a rule Medicare cover tube feeding formula and supplies if the it is 1)going through a feeding tube 2)expected to be needed for longer than 3 months 3)there is a "permanent" non-function of the intestines or the organs required to get the food to the intestines (ie dysphagia, esophageal fistula, head and neck cancer).

Is a feeding tube considered skilled nursing?
The services that Medicare defines as skilled are: Intravenous or intramuscular injections and intravenous feeding. Enteral feeding (i.e., “tube feedings”) that comprises at least 26 per cent of daily calorie requirements and provides at least 501 milliliters of fluid per day.
How do you bill for enteral formula?
Products that are only administered orally should be coded as A9270. Code B4149 describes formulas containing natural foods that are blenderized and packaged by a manufacturer. B4149 formulas are classified based upon this manufacturer requirement, not on the composition of the enteral formula.
Does Medicare cover B4034?
Coverage for these products is at the discretion of the individual carrier in alignment with the patient's benefits. Note for medicare patients: Enteral feeding supply kits (B4034-B4036) have a one unit daily allowance, therefore refill requirements are not applicable to these HCPCS codes.
Is total parenteral nutrition covered by Medicare?
The HPN Policy Under Medicare Parenteral nutrition is covered for a beneficiary with permanent, severe pathology of the alimentary tract which does not allow absorption of sufficient nutrients to maintain weight and strength commensurate with the beneficiary's general condition.”
Does Medicare cover PEG tube feedings?
Both Medicare and other-payers routinely cover enteral nutrition therapy when the patient requires tube feeding, when enteral nutrition is the patient's exclusive source of nutrition, and if the patient has an anatomical or physiological malfunction of the gastrointestinal tract.
How do I bill Medicare for enteral nutrition?
Enteral Nutrition Coding Guidelines Enteral feeding supply allowances (B4034, B4035, and B4036) include all supplies, other than the feeding tube and nutrients, required for the administration of enteral nutrients to the beneficiary for one day. Only one unit of service may be billed for any one day.
What is B4034?
B4034 is a valid 2022 HCPCS code for Enteral feeding supply kit; syringe fed, per day, includes but not limited to feeding/flushing syringe, administration set tubing, dressings, tape or just “Enter feed supkit syr by day” for short, used in Enteral/parenteral nutrients/supplies.
What is included in B4224?
B4224 is a valid 2022 HCPCS code for Parenteral nutrition administration kit, per day or just “Parenteral administration ki” for short, used in Enteral/parenteral nutrients/supplies.
What is CPT code B4150?
Short Description: EF complet w/intact nutrient. Long Description: ENTERAL FORMULA, NUTRITIONALLY COMPLETE WITH INTACT NUTRIENTS, INCLUDES PROTEINS, FATS, CARBOHYDRATES, VITAMINS AND MINERALS, MAY INCLUDE FIBER, ADMINISTERED THROUGH AN ENTERAL FEEDING TUBE, 100 CALORIES = 1 UNIT.
Does Medicare pay for TPN at home?
Medicare coverage: Medicare covers TPN both at home and in the hospital. When TPN is administered in the hospital, payment for it is included in the diagnosis-related group (DRG) payment.
Is TPN covered by Medicare Part B?
For parenteral nutrition therapy to be covered under Part B, the claim must contain a physician's written order or prescription and sufficient medical documentation to permit an independent conclusion that the requirements of the prosthetic device benefit are met and that parenteral nutrition therapy is medically ...
How much does a TPN cost?
The cost for TPN Electrolytes intravenous solution ((Lypholyte II/Nutrilyte II/TPN Electrolytes)) is around $186 for a supply of 500 milliliters, depending on the pharmacy you visit.
What is the phone number for feeding tubes?
In this article, we’ll go through the basics and must-know info surrounding feeding tubes. If you'd rather chat in person, give us at call at 855-879-2366. We have been providing patients with enteral feeding and nutrition supplies and helping our customers get covered by insurance since 1984.
What is a feeding tube?
A feeding tube is a flexible, medical grade tube that delivers essential nutrition to your body when consuming food by mouth is not an option. The feeding tube, also known as an enteral tube, carries a tube feeding formula into the body.
What is tube feed?
Tube feeding formula, also known as tube feed, is a formulation of liquid nutrients to provide your body with the nutrition it needs via a feeding tube. The tube feed formula will contain all the essential macro and micronutrients your body requires, including carbs, fat, protein, vitamins and minerals, and water for hydration.
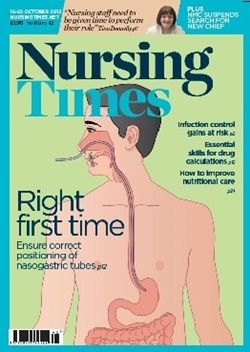
How long does a nasogastric tube last?
Nasogastric feeding tube (NG): The feeding tube is inserted through the nose, down the esophagus, into the stomach. It is typically used for short-term (6-8 weeks max) tube feeding.
When to use Gastrostomy tube?
This is used most often for short-term feeding (6-8 weeks) when the patient’s stomach isn’t able to handle receiving the tube feed directly. Gastrostomy tube: The feeding tube is surgically inserted (through a small incision) into the stomach. This is used when a patient needs a feeding tube for long-term use.
Does insurance pay for feeding tubes?
Getting insurance to pay for feeding tube formula, feeding tubes. There are lots of rules and regulations surrounding feeding tubes, and they can be confusing and frustrating. Insurance companies are very particular about when they will pay for feeding tube nutrition. As a long-standing medical supply company, we can shed a little light on those ...
Does insurance cover gravity bags?
For some people who are continuously tube fed, insurance will cover a backpack that holds the feeding pump. Some insurance companies will also cover gravity bags. These hold the enteral nutrition while it hangs by an IV drip. However, because a gravity bag only delivers nutrition intermittently and not continuously like a pump, other insurance companies deem them “not medically necessary.” Those companies typically only pay for syringes, which can also be used to feed a patient intermittently.
Does Medicare cover enteral nutrition?
Medicare covers enteral nutrition therapy, commonly called tube feeding, for beneficiaries who cannot swallow due to a permanent medical problem or an impairment of long and indefinite duration. Medicare Part B coverage of enteral nutrition therapy is provided under the prosthetic device benefit for beneficiaries residing at home, or in a nursing facility when the stay is not covered by Medicare Part A. Medicare Part B payments for enteral nutrition formulas totaled more than $311 million in calendar year 2001.
Is enteral formula lower than Medicare?
The findings of this report suggest that the supplier community obtains Category I enteral nutrition formula products at prices that are lower than Medicare’s reimbursement amount. If Medicare’s reimbursement amount had been based more closely on these prices, the program and its beneficiaries could have realized savings.
How much will walk-in tub cost with Medicare coverage?
If Medicare accepts reimbursement for your walk-in tub, they only going to reimburse the full purchase price of the walk-in tub. It’s very rare they pay the installation costs and other modifications at home that you maybe need to fit your walk-in tub in your bathroom, like accessibility modifications.
What is a medical report for a walk in tub?
Either a medical report showing diagnosis or a prescription written by a registered physician may serve the purpose well. The prescription or diagnostic report should essentially outline some authentic reasons which may prove the necessity of getting a walk-in tub.
What is a walk-in tub, and why would I need one?
A walk-in tub has been modified so you no longer have to worry about this issue! They also come equipped with safety features such as seats which allow you to take advantage of all their benefits while keeping yourself safe at all times.
What is Medicare 2021?
Learn How (2021) Medicare is a federal health insurance program administered by the U.S. Department of Health and Human Services (HHS). Medicare sometimes considers walk in tub as durable and effective medical equipment for seniors who need special care when looking for a comfortable and safe bath. Medicare provide coverage for lower-income people ...
Does Medicare cover surgical supplies?
Pre-2018, Medicare did not cover any surgical supplies for men or women age 55 and older. Now, they do cover them.
Does gathering all the above support documents mean Medicare guarantees its assistance?
Gathering all the above supportive documents does not necessarily mean that Medicare guarantees its assistance.
Does Medicare cover blind people?
Medicare provide coverage for lower-income people and people with barriers to care. For example, people with certain medical conditions, undocumented immigrants, and people who are blind or disabled may not be eligible for coverage through their state’s private insurance market.
How many days does a person get tube fed?
Here is one example: A person getting tube fed uses 100 days of their benefit, goes off Medicare Part A, has a 60 day break in illness, and was then readmitted to hospital with a hip fracture. He is getting 100% of his caloric intake through the tube feeding.
How long does a resident stay in the community after being 100% tube fed?
2. The resident is discharged to the community after using 100 days, whether or not he is 100% tube fed. He is not hospitalized in the next 60 days and then gets pneumonia, is admitted to the hospital for three consecutive midnights and then transferred to the SNF. Now, in all likelihood, Medicare A will cover the stay with a new benefit period since he went 60 consecutive days without a hospital stay.
How long can a resident go without Medicare?
The fact the resident went 60 days without Medicare reimbursement does not satisfy the 60 days of wellness requirement as long as he is 100% tube fed. Let’s look at a few different scenarios: 1. The resident remains in the facility after exhausting their Medicare Part A days.
Is a resident still skilled for tube feeding?
The resident is still skilled for tube feeding in accordance with the guidelines, regardless of the current payer. The facility is required to send in benefit exhaust bills on a monthly basis until the resident is no longer skilled (in this case, the resident is weaned from the tube or is provided less than 26% of the calories or less ...
Is tube feeding skilled?
A: The issue here is whether the tube feeding is skilled or not. If 26% of the calories and 500 cc of fluid are going through the tube, then the tube feeding is skilled. After the 100 days of Medicare Part A benefits are exhausted, the 60 days of wellness does not begin until the tube is no longer skilled. The fact the resident went 60 days without ...
