How to Read Your Part A Medicare Summary Notice (full text)
- 1. Medicare Summary Notice Medicare sends out statements like this example quarterly. ...
- 2. Name and Address If the name or address listed here is not correct, visit your local Social Security Administration office or call 800-772-1213 (TTY 800-325-0778 for the deaf or ...
- 3. This Is Not a Bill Yes, that's right! ...
- 4. ...
- 5. ...
- 6. ...
- 7. ...
- 8. ...
- 9. ...
- 10. ...
Full Answer
How long to keep Medicare summary notices?
Most experts recommend saving your Medicare summary notices for one to three years. At the very least, you should keep them while the medical services listed are in the process of payment by Medicare and supplemental insurance. How long you keep these records depends on your personal preference.
How to understand Medicare summary notices?
What should I do if I get this notice?
- If you have other insurance, check to see if it covers anything that Medicare didn’t.
- Keep your receipts and bills, and compare them to your MSN to be sure you got all the services, supplies, or equipment listed.
- If you paid a bill before you got your notice, compare your MSN with the bill to make sure you paid the right amount for your services.
How to read your Medicare summary Notice (MSN)?
The Medicare Summary Notice
- Authenticity. An MSN is a detailed statement about services that have been charged to Medicare during that time frame but is not a bill in and of itself.
- Deductibles. Your deductible status will be listed in the left-hand column on Page 1. ...
- Claims. Page 1 of your Medicare Summary Notice lists a brief overview of "Your Claims & Costs This Period". ...
What is a concern about the future of Medicare?
The shift to pay for performance, with its additional burdens on providers to document quality outcomes, is what Norrell sees as the next major hurdle for Medicare. Tying in to that is the public's greatest concern: the future financial viability of Medicare.
How do I read a Medicare Summary Notice?
The Part A Medicare summary notice shows the dates of the claims, how much of the deductible you have met, whether Medicare approved all of the claims, and the total amount you may be billed from the facility. It also lists the facilities where you have had claims this period and the dates you received services there.
What does the Medicare Summary Notice list?
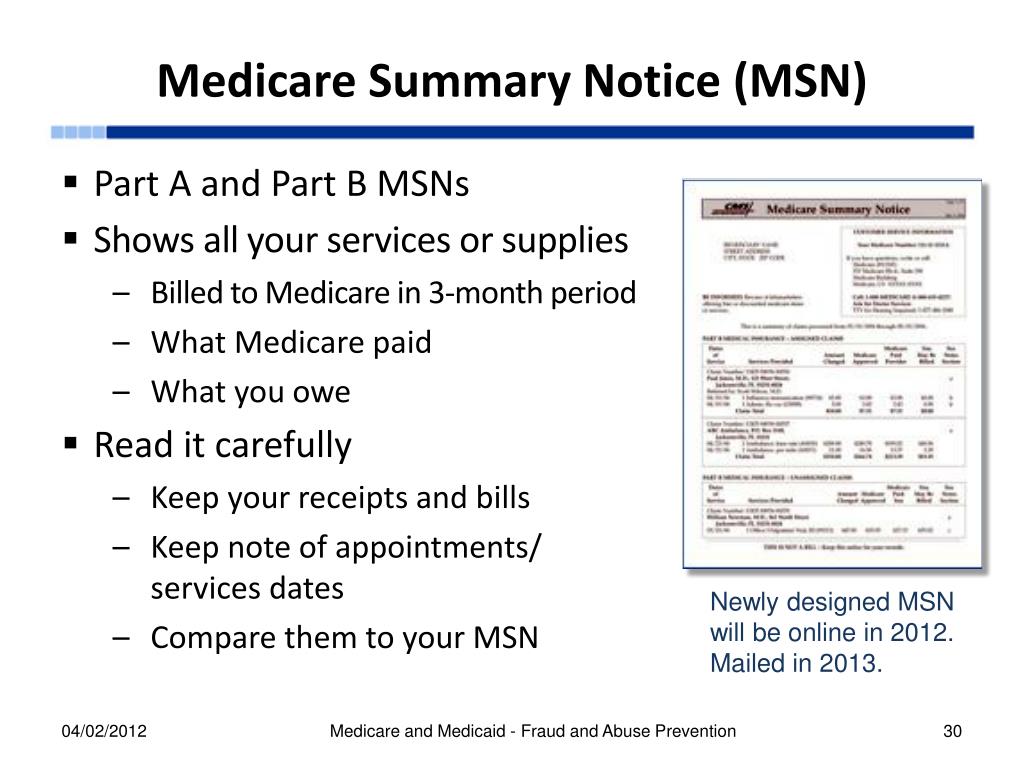
It's a notice that people with Original Medicare get in the mail every 3 months for their Medicare Part A and Part B-covered services. The MSN shows: All your services or supplies that providers and suppliers billed to Medicare during the 3-month period.
How do you read a Medicare EOB?
How to Read Medicare EOBsHow much the provider charged. This is usually listed under a column titled "billed" or "charges."How much Medicare allowed. Medicare has a specific allowance amount for every service. ... How much Medicare paid. ... How much was put toward patient responsibility.
Should I keep Medicare summary notices?
How Long Should You Keep Medicare Summary Notices? Most experts recommend saving your Medicare summary notices for one to three years. At the very least, you should keep them while the medical services listed are in the process of payment by Medicare and supplemental insurance.
Which is an easy to read monthly statement that clearly lists Medicare claims information?
The MSN is an easy‑to‑read statement that clearly lists your health insurance claims information. For more information on filing an appeal, visit Medicare.gov/appeals, or call 1‑800‑MEDICARE (1‑800‑633‑4227). TTY users can call 1‑877‑486‑2048.
How do providers check Medicare claim status?
Providers can enter data via the Interactive Voice Response (IVR) telephone systems operated by the MACs. Providers can submit claim status inquiries via the Medicare Administrative Contractors' provider Internet-based portals. Some providers can enter claim status queries via direct data entry screens.
How do you read an EOB for dummies?
1:342:35How to Read Your Medical EOB - YouTubeYouTubeStart of suggested clipEnd of suggested clipThe amount you pay for the service this is the amount that you will be billed. Remember the EOB isMoreThe amount you pay for the service this is the amount that you will be billed. Remember the EOB is not a bill it just shows you how the costs are distributed. If you have any questions by your EOB.
What is a summary of benefits and coverage?
An easy-to-read summary that lets you make apples-to-apples comparisons of costs and coverage between health plans. You can compare options based on price, benefits, and other features that may be important to you.
What do you do with explanation of benefits?
What should you do with an EOB? You should always save your Explanation of Benefits forms until you get the final bill from your doctor or health care provider. Compare the amount you owe on the EOB to the amount on the bill. If they match, that's the amount you'll need to pay.
Do I need to shred Medicare summary notices?
Save your Medicare Summary Notices and related statements until they are no longer useful. But, don't just throw them in the trash-- be sure to shred them. Shredding important documents like your MSN and other health care bills will ensure that thieves cannot get their hands on your private information.
What is a summary notice?
Summary Notice means the summary notice of proposed settlement and hearing for publication acceptable to the Parties and approved by the Court.
Should I keep Explanation of Benefits?
Comparing your EOBs to your monthly statements is a good way to understand what you are being charged for, and it gives you another opportunity to look for overcharges. Unlike medical bills, EOBs should be kept from three to eight years after your procedure, or indefinitely if you have a reoccurring condition.
What is the summary notice for Medicare?
This summary is in the right-hand column and lets you know if Medicare denied coverage for any services that quarter and how much you can expect to be billed. Page 3 provides a more detailed summary of each service and its charges.
How often do you get a Medicare summary notice?
The Medicare Summary Notice. If you are on Original Medicare (Part A and Part B), you will receive a Medicare Summary Notice (MSN) quarterly, i.e., every 3 months. You will receive separate MSNs for Part A and Part B coverage.
What is an ABN for Medicare?
The ABN is an acknowledgment that Medicare may not cover the service and that you are willing to pay out of pocket for the service. If you did sign an ABN, it is not valid if it is illegible, if it is signed after the service was performed, or if it is otherwise incomplete.
What is MSN bill?
An MSN is a detailed statement about services that have been charged to Medicare during that time frame but is not a bill in and of itself. THIS IS NOT A BILL will be printed in bold capitalized letters at the top of the statement.
How long does a deductible last for a nursing home?
It ends when you have not received inpatient hospital or skilled nursing facility care for 60 days in a row. You will pay a deductible for each benefit period and multiple deductibles may be listed here. In 2020, each deductible costs $1,408.
What to do if your Medicare records don't match?
Whenever you see something that does not match up with your records, reach out to your doctor or medical office for clarification. There could have been a misunderstanding or a true billing error. In the worst-case scenario, it could be a sign of Medicare fraud and abuse.
Does Medicare cover limiting charges?
Medicare does not cover the limiting charge. Amount Medicare Paid: This lets you know the total amount Medicare paid for covered services. Medicare covers 80% of the cost for most services but will pay for 100% of costs for preventive care services if they are ordered by a participating provider.
What is the most important part of a Medicare notice?
Let’s talk a bit about the notes column. In our opinion, the footnotes are the most important part of the notice. Medicare is required to give an explanation for every claim that is denied, every charge you may be incurring. Each charge usually has one footnote, sometimes even more than that.
What is the gray box on Medicare Part A?
Under the gray box is your deductible status. Please do not get the deductibles for Medicare Part A and Part B confused. A deductible period for part A can happen multiple times in a year and is significantly higher than the Medicare Part B deductible.
What is a Medicare Part A deductible?
Remember the definition of deductible: this is the amount that someone must pay before Medicare pays its share.
What does "assigned claim" mean?
An assigned claim means a doctor has agreed to accept Medicare’s charges in full and may not bill you the difference. Please be aware this is not the same as the typical 20% amount owed. That may still be charged as it is part of the assignment-agreed upon amount. Under the top section are definitions.
Is Part A an annual period?
This is especially important under the Part A notice, because many people are unaware how Part A’s benefit period works. It is not an annual period. The last section on page two is a message from Medicare. Medicare typically has two or three advisories on each notice for you each time you get one.
Do Medicare Advantage members get notices?
Please note that Medicare Advantage members will NOT receive notices like these. If you have a Medicare Advantage plan and need help understanding your bills, it will be in your best interest to speak with your qualified insurance broker or a member of that company’s customer service team for assistance.
Introduction
If you are enrolled in Medicare, you should be receiving Medicare plan documents like the Medicare Explanation of Benefits (EOB) or Medicare Summary Notices (MSN) when you receive care or use your plan’s benefits.
What information is included in the Medicare EOB?
The Explanation of Benefits contains your plan’s description and claim-related details like:
What is the purpose of the Medicare EOB?
These Medicare plan documents help you save money and track fraud. Here’s how:
What should you expect to see in the MSN?
If you’re enrolled in Original Medicare, you will receive an MSN instead of an EOB. An MSN shows similar information to an EOB.
Conclusion
In summary, Medicare EOBs and MSNs are important notices to help you keep track of your healthcare expenses and what your insurance covers, amongst other things. They’re also important documents if you want to make a claim or contest a charge. Remember to keep these Medicare plan documents for at least one calendar year.
How often is Medicare mailed?
account. Each MSN includes instructions to file an appeal if one of your claims is denied. MSNs are mailed every three months if you’ve received any Medicare-covered services.
What is an MSN statement?
Medicare Summary Notices are detailed statements mailed by Medicare every three months. Your MSN will include your account’s claims, the doctors you visited, how much was paid, and more. An MSN is not a bill. Think of your MSNs as Medicare statements. As with your bank statements, you can use an MSN to verify that your account’s activity matches ...
Is Medicare a bill?
A Medicare Summary Notice (MSN) is not a bill. Original Medicare is a fee-for-service health insurance program available to Americans aged 65 and older and some individuals with disabilities. Original Medicare is provided by the federal government and is made up of two parts: Part A (hospital insurance) and Part B (medical insurance). account.
Is Medicare Supplement endorsed by the government?
Medicare Supplement insurance plans are not connected with or endorsed by the U.S. government or the federal Medicare program. Our mission is to help every American get better health insurance and save money. If you’re looking for the government’s Medicare site, please navigate to www.medicare.gov.
Does Medicare Advantage have an EOB?
Private health insurance companies provide Medicare Advantage and Part D plans, and each company creates its own EOB to send to its customers. That means an EOB from one company can look very different from another company’s EOB. MSNs, however, are all formatted the same way.