Usually, the payor of the deductible is either you or an insurance policy such as a Medicare supplement. On the top box on the right hand column of the summary notice is the total you may be billed section. This will tell you if Medicare approved all claims in the notice.
Full Answer
How do I Read my Medicare/HHS notice?
The notice you receive is going to be a minimum or four pages long. Let’s look at the first page. Page 1 is called your “Dashboard.” At the top left corner of the page is the Medicare/HHS logo. Directly under that in a gray box under your address is your information.
How do I Check my Medicare prescription drug costs?
Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. This notice gives you a summary of your prescription drug claims and costs.
How do I Check my Medicare bill status?
Medicare’s Medicare.gov website allows beneficiaries in Original Medicare to log into (or create) a secure Medicare account to view their most recent MSNs, track claims made on their behalf, and check payment status. Creating a free, secure account with Medicare allows you to review all bills processed within the past 36 months.
How can I get help understanding my Medicare Advantage bills?
If you have a Medicare Advantage plan and need help understanding your bills, it will be in your best interest to speak with your qualified insurance broker or a member of that company’s customer service team for assistance.
What is the most important part of a Medicare notice?
What is a Medicare Part A deductible?
What is the gray box on Medicare Part A?
Do Medicare Advantage members get notices?
How do you read a Medicare bill?
It will begin with the date you saw the provider and the provider's name and office. Under that will be the line item for each service. To the right of the approval column is the amount the provider charged Medicare. And to the right of that column is the amount Medicare approved.
How do I read my Medicare EOB?
How to Read Medicare EOBsHow much the provider charged. This is usually listed under a column titled "billed" or "charges."How much Medicare allowed. Medicare has a specific allowance amount for every service. ... How much Medicare paid. ... How much was put toward patient responsibility.
How do I view my Medicare statements?
Log into (or create) your Medicare account. Select "Get your Medicare Summary Notices (MSNs) electronically" under the "My messages" section at the top of your account homepage.
How much does Medicare charge each month?
$170.10 each month (or higher depending on your income). The amount can change each year. You'll pay the premium each month, even if you don't get any Part B-covered services.
Why are the charge and allowable charge different amounts?
Actual charges are a bit different and refer to the amount billed by the provider for the specific service. The allowed amount is the amount your insurance carrier is willing to pay for the rendered service. The difference between these amounts is called a contractual write-off.
How do I find out my deductible?
“Your deductible is typically listed on your proof of insurance card or on the declarations page. If your card is missing or you'd rather look somewhere else, try checking your official policy documents. Deductibles are the amount of money that drivers agree to pay before insurance kicks in to cover costs.
How do I know what Medicare has paid?
Log into (or create) your secure Medicare account. You'll usually be able to see a claim within 24 hours after Medicare processes it....It shows:All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period.What Medicare paid.The maximum amount you may owe the provider.
Why is my first Medicare bill so high?
If you're late signing up for Original Medicare (Medicare Parts A and B) and/or Medicare Part D, you may owe late enrollment penalties. This amount is added to your Medicare Premium Bill and may be why your first Medicare bill was higher than you expected.
How do I get my yearly Medicare statement?
If you have lost your MSN or you need a duplicate copy, call 1-800-MEDICARE or go to your account on www.mymedicare.gov.
How much is the Medicare premium for 2021?
The standard monthly premium for Medicare Part B enrollees will be $148.50 for 2021, an increase of $3.90 from $144.60 in 2020. The annual deductible for all Medicare Part B beneficiaries is $203 in 2021, an increase of $5 from the annual deductible of $198 in 2020.
How do I get my $144 back from Medicare?
Even though you're paying less for the monthly premium, you don't technically get money back. Instead, you just pay the reduced amount and are saving the amount you'd normally pay. If your premium comes out of your Social Security check, your payment will reflect the lower amount.
Is Medicare Part A and B free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
Medicare Summary Notice | CMS
Messages are printed on the MSN to explain both general and claims-specific information to beneficiaries. Contractors responsible for printing MSNs are notified of new or revised MSN messages through Technical Direction Letters or Change Requests.
Medicare Summary Notice (MSN) - Medicare Interactive
The Medicare Summary Notice (MSN) is a summary of health care services and items you have received during the previous three months. The MSN is not a bill. The contractor that processes your claims for Medicare will send you the MSN, so it may have the name and address of a private company on it.. MSNs are usually mailed four times a year (quarterly) and contain information about charges ...
Medicare Summary Notice Part B
Your New MSN: Part B | Page 3. Page 1 – Your Dashboard. Medicare Summary Notice. Page 1 of 4. for Part B (Medical Insurance) The Official Summary of Your Medicare Claims from the Centers for Medicare & Medicaid Services
How to Read Your Part B Medicare Statement
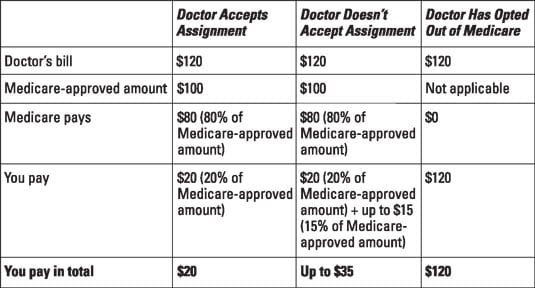
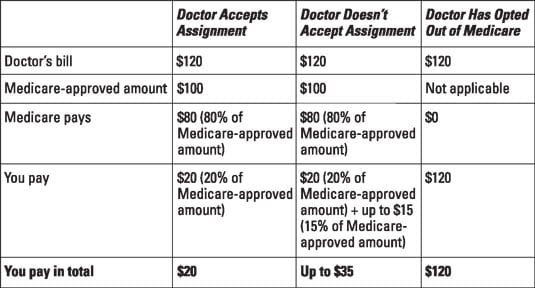
Amount Medicare Paid: This is the amount Medicare paid the provider. This is usually 80% of the Medicare-approved amount. Maximum You May Be Billed: This is the total amount the provider is allowed to bill you. This is usually $0. For durable medical equipment, it can include 20% of the Medicare-approved amount.
Can Dr. bill patient what Medicare did not pay? - AgingCare.com
No. And we just got another bill from the hospital. They did send me a form she signed at the time she had the lab work done and it showed an out of pocket cost of $170 but I still think they are over charging because they acknowledge that Medicare approved $32.77 so they should only be charging her 20%.
What to do if your Medicare records don't match?
Whenever you see something that does not match up with your records, reach out to your doctor or medical office for clarification. There could have been a misunderstanding or a true billing error. In the worst-case scenario, it could be a sign of Medicare fraud and abuse.
How often do you get a Medicare summary notice?
The Medicare Summary Notice. If you are on Original Medicare (Part A and Part B), you will receive a Medicare Summary Notice (MSN) quarterly, i.e., every 3 months. You will receive separate MSNs for Part A and Part B coverage.
What is the summary notice for Medicare?
This summary is in the right-hand column and lets you know if Medicare denied coverage for any services that quarter and how much you can expect to be billed. Page 3 provides a more detailed summary of each service and its charges.
What is an ABN for Medicare?
The ABN is an acknowledgment that Medicare may not cover the service and that you are willing to pay out of pocket for the service. If you did sign an ABN, it is not valid if it is illegible, if it is signed after the service was performed, or if it is otherwise incomplete.
How long does a deductible last for a nursing home?
It ends when you have not received inpatient hospital or skilled nursing facility care for 60 days in a row. You will pay a deductible for each benefit period and multiple deductibles may be listed here. In 2020, each deductible costs $1,408.
How much can a non-participating provider charge for a limiting charge?
Non-participating providers can add a limiting charge up to 15% more than what is recommended on the fee schedule. Medicare Approved Amount: This lets you know the dollar amount for any services approved for coverage by Medicare. Medicare does not cover the limiting charge.
Is balance billing against the law?
That is called balance billing and it is against the law. Check to see if you signed an Advanced Beneficiary Notice (ABN) for any services Medicare did not approve. You are not liable to pay for these services unless you signed an Advanced Beneficiary Notice beforehand.
Introduction
If you are enrolled in Medicare, you should be receiving Medicare plan documents like the Medicare Explanation of Benefits (EOB) or Medicare Summary Notices (MSN) when you receive care or use your plan’s benefits.
What information is included in the Medicare EOB?
The Explanation of Benefits contains your plan’s description and claim-related details like:
What is the purpose of the Medicare EOB?
These Medicare plan documents help you save money and track fraud. Here’s how:
What should you expect to see in the MSN?
If you’re enrolled in Original Medicare, you will receive an MSN instead of an EOB. An MSN shows similar information to an EOB.
Conclusion
In summary, Medicare EOBs and MSNs are important notices to help you keep track of your healthcare expenses and what your insurance covers, amongst other things. They’re also important documents if you want to make a claim or contest a charge. Remember to keep these Medicare plan documents for at least one calendar year.
What is Medicare statement?
Medicare statements outline payments made on a beneficiary’s behalf for Medicare covered services. There are two primary types of statements received by Medicare beneficiaries: Medicare Summary Notices (MSNs) and Explanations of Benefits (EOBs). Beneficiaries enrolled in Original Medicare receive MSNs. Beneficiaries enrolled in Medicare Advantage ...
What is Medicare Summary Notice?
The Medicare Summary Notice (MSN), which provides information on Original Medicare claims, is one of the key tools that the SMP program uses for catching fraud, errors, and abuse. Reviewing and understanding MSNs is crucial for both Medicare beneficiaries and for SMPs.
How to Read Medicare EOBs
Medicare EOBs are sent each time Medicare processes a claim from one of your health care providers. You should receive one a few weeks or so after any medical services.
How to Read Medicare MSNs
You receive a Medicare Summary Notice every quarter that you receive Medicare-covered health care services. The notice summarizes how much Medicare paid for services during that period and how much you may owe out-of-pocket.
What to do if your bill does not include a detailed list of charges?
If your bill does not include a detailed list of charges, call the doctor's or hospital's billing office and ask for an itemized invoice. That's the only way to make sure you're being charged just for services you received.
How many digits are in a medical procedure code?
Every medical procedure has a corresponding five-digit code. These numerical systems, called Current Procedural Terminology (CPT) for insurance and the Healthcare Common Procedure Coding System (HCPCS) for Medicare, determine how much your provider will be paid.
What does "insurance payment" mean?
The “insurance payment” or “plan payment” shows what portion of the charges your insurance company has paid. If no payments appear here, your plan may not yet have paid what it owes — check with your insurer before paying the amount listed as due. If your bill does not include a detailed list of charges, call the doctor's or hospital's billing ...
What is an EOB in Medicare?
Every medical procedure or visit will show up on an explanation of benefits (EOB) from your insurance company or a Medicare Summary Notice (MSN). These list the services performed, what the doctor or hospital charged, what your insurance company or Medicare paid, and what you owe. Make sure the dates and codes on that statement match the bills you receive from medical providers.
What to do if you are admitted after midnight?
If you were formally admitted after midnight, make sure your charges start on that day. Also, most insurance companies don’t allow hospitals to charge room fees for the day you’re discharged. Be on the lookout, too, for billing irregularities that could be signs of fraud.
What is duplicate charge?
Duplicate charges are surprisingly common, Palmer says. A treatment, medication or procedure you didn’t receive. If you were scheduled for a test or procedure but it was canceled, it could still end up on your bill because no one struck it from your chart. Inflated surgery and recovery times.
What happens if a coder adds a 0 to a number?
If a coder mistakenly adds a 0 to a number, you could be charged for 100 pills instead of 10, potentially adding hundreds of dollars to your invoice. Also, make sure a service or procedure isn’t listed more times than it was performed. Duplicate charges are surprisingly common, Palmer says.
How long does it take to see a Medicare claim?
Log into (or create) your secure Medicare account. You’ll usually be able to see a claim within 24 hours after Medicare processes it. A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare.
What is Medicare Part A?
Check the status of a claim. To check the status of. Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. or.
What is MSN in Medicare?
The MSN is a notice that people with Original Medicare get in the mail every 3 months. It shows: All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period. What Medicare paid. The maximum amount you may owe the provider. Learn more about the MSN, and view a sample.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
What is a PACE plan?
PACE plans can be offered by public or private companies and provide Part D and other benefits in addition to Part A and Part B benefits. claims: Contact your plan.
Is Medicare paid for by Original Medicare?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. or other. Medicare Health Plan. Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan.
Does Medicare Advantage offer prescription drug coverage?
Medicare Advantage Plans may also offer prescription drug coverage that follows the same rules as Medicare drug plans. Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. This notice gives you a summary of your prescription drug claims and costs.
What is Medicare Summary Notice?
A Medicare Summary Notice (MSN) is the statement that shows all the services or supplies billed to Medicare on your account, how much of the bill Medicare paid and how much you still owe the provider or supplier.
What is the number to call if you have questions about your MSN?
If you still have questions about your MSN or there's something you and your health care provider cannot resolve, call 800-MEDICARE (800-633-4227). If Medicare has not paid a claim you think should have been paid, you have the right to appeal. (See "Appealing a Medicare Claim Decision.")
What to do if you lost your MSN?
If you've lost an MSN or want a duplicate, you can use the same website to request that a paper copy be sent to you. If there's an entry for services or supplies that Medicare did not cover, but you believe is a covered service, call your medical provider's office to make sure the claim was submitted correctly.
Do you need to send a bill with a Medicare summary notice?
A Medicare Summary Notice is not a bill. You do not need to send anyone a payment when you receive an MSN. You should compare the information on your MSN with bills, statements and receipts from your health care providers and suppliers.
How to determine payment rate for a service?
To determine the payment rate for a service, CMS systems multiply the sum of the geographically adjusted RVUs by a CF in dollars. The statute specifies the formula by which the CF is updated on an annual basis.
Why does Medicare adjust each of the 3 RVUs?
Medicare adjusts each of the 3 RVUs to account for geographic variations in the costs of practicing medicine in different areas of the country. Each kind of RVU component has a corresponding GPCI adjustment.
What is a CMS 460?
s enrolled in Medicare and signed the Form CMS-460, Medicare Participating Physician or Supplier Agreement, agreeing to charge no more than Medicare-approved amounts and deductibles and coinsurance amounts. Participating professionals and suppliers submit assigned claims.
When did Medicare PFS change?
Effective January 1, 2017, the Medicare Access and CHIP Reauthorization Act of 2015 repealed the previous formula to update the Medicare PFS and replaced it with several years of increases to overall payments for PFS services. In conjunction with that change, the law created the QPP, which rewards the delivery of high-quality and cost-ecient beneficiary care.
How to change search criteria?
If you wish to change the search criteria, type in a new code or other factor at the top of the page and then click on Search fees. To download, or copy the link for your search results, select 1 of these options below the Search Results table.
What is the most important part of a Medicare notice?
Let’s talk a bit about the notes column. In our opinion, the footnotes are the most important part of the notice. Medicare is required to give an explanation for every claim that is denied, every charge you may be incurring. Each charge usually has one footnote, sometimes even more than that.
What is a Medicare Part A deductible?
Remember the definition of deductible: this is the amount that someone must pay before Medicare pays its share.
What is the gray box on Medicare Part A?
Under the gray box is your deductible status. Please do not get the deductibles for Medicare Part A and Part B confused. A deductible period for part A can happen multiple times in a year and is significantly higher than the Medicare Part B deductible.
Do Medicare Advantage members get notices?
Please note that Medicare Advantage members will NOT receive notices like these. If you have a Medicare Advantage plan and need help understanding your bills, it will be in your best interest to speak with your qualified insurance broker or a member of that company’s customer service team for assistance.
