
Open the patient file, and select Transactions. Right-click the appropriate transaction and select 'Medicare Online', followed by the type of claim to be submitted (Patient Claim, Medicare BB or DVA). Complete the Medicare/DVA claiming wizard to resubmit the claim using the corrected information.
Full Answer
How do I resubmit a claim?
Make Changes, Add Reference/Resubmission Numbers, and Then Resubmit: To resolve a claim problem, typically you will edit the charges or the patient record, add the payer claim control number, and then resubmit or “rebatch” the claim. Make sure you always perform that final step–otherwise the changes you made to the charges won’t make a difference.
How do I file a Medicare claim?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
How do I get a copy of my Medicare redetermination form?
You can also use the Medicare Redetermination Form (20027) for this step. If you can’t download the form, call 800-MEDICARE (800-633-4227) to request a copy by mail. The process for appealing a Part A or B claim has several steps
Can I resubmit a Medicaid claim that has been denied?
Do not resubmit a claim denied because of Medicaid program limitations or policy regulations. Computer edits ensure that it will be denied again. · Check recently received remittance voucher dates.
Can you resubmit a Medicare claim?
The claim is missing information necessary to process the claim. The claim can be corrected or resubmitted. All line items on the claim are rejected.
How do I resubmit a rejected Medicare claim?
When a claim is denied because the information submitted was incorrect, often the claim can be reopened using a Clerical Error Reopening (CER). CERs can be used to fix errors resulting from human or mechanical errors on the part of the party or the contractor.
How long do I have to submit a corrected claim to Medicare?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share.
How do I reopen a Medicare claim?
The Reopening process allows providers to correct clerical errors or omissions without having to request a formal appeal. Most reopenings can be initiated through Self Service Reopenings via the Noridian Medicare Portal (NMP). All other requests can be initiated by telephone or in writing.
How do I correct a denied Medicare claim?
File your appeal within 120 days of receiving the Medicare Summary Notice (MSN) that lists the denied claim. Circle the item on your MSN that you are appealing and clearly explain why you think Medicare's decision is wrong. You can write on the MSN or attach a separate page.
How do I correct a Medicare billing error?
If the issue is with the hospital or a medical provider, call them and ask to speak with the person who handles insurance. They can help assist you in correcting the billing issue. Those with Original Medicare (parts A and B) can call 1-800-MEDICARE with any billing issues.
How do you correct a claim?
Make Changes, Add Reference/Resubmission Numbers, and Then Resubmit: To resolve a claim problem, typically you will edit the charges or the patient record, add the payer claim control number, and then resubmit or “rebatch” the claim.
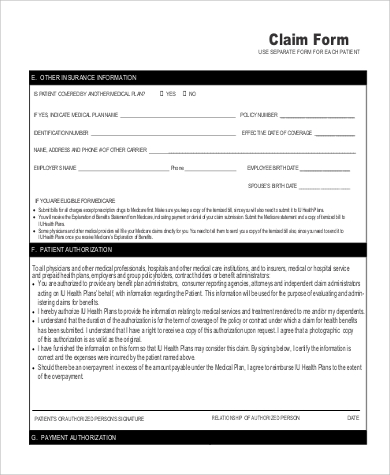
What is the resubmission code for a corrected claim?
7Complete box 22 (Resubmission Code) to include a 7 (the "Replace" billing code) to notify us of a corrected or replacement claim, or insert an 8 (the “Void” billing code) to let us know you are voiding a previously submitted claim.
What is the difference between a corrected claim and a replacement claim?
A corrected or replacement claim is a replacement of a previously submitted claim (e.g., changes or corrections to charges, clinical or procedure codes, dates of service, member information, etc.). The new claim will be considered as a replacement of a previously processed claim.
What is the difference between a redetermination and an reopening?
2:545:03Reopening vs. Redetermination - YouTubeYouTubeStart of suggested clipEnd of suggested clipAnd assert smirk and/or rack denials no please keep in mind that a redetermination is the firstMoreAnd assert smirk and/or rack denials no please keep in mind that a redetermination is the first level of appeals providers must adhere to the following stipulations.
What is corrected claim?
A corrected claim is a replacement of a previously submitted claim. Previously submitted claims that were completely rejected or denied should be sent as a new claim.
What is a Medicare clerical reopening?
A clerical error reopening is a process that allows you to change claim data without submitting a written appeal. You can fax a clerical error reopening form. You cannot submit a reopening to add items or services not previously billed.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
What to call if you don't file a Medicare claim?
If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227) . TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and your doctor or supplier still hasn't filed the claim, you should file the claim.
How to file a medical claim?
Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1 The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2 The itemized bill from your doctor, supplier, or other health care provider 3 A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare 4 Any supporting documents related to your claim
How do I file a claim?
Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What is an itemized bill?
The itemized bill from your doctor, supplier, or other health care provider. A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare.
How long does it take for Medicare to pay?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
What happens after you pay a deductible?
After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). , the law requires doctors and suppliers to file Medicare. claim. A request for payment that you submit to Medicare or other health insurance when you get items and services that you think are covered.
When do you have to file Medicare claim for 2020?
For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020. Check the "Medicare Summary Notice" (MSN) you get in the mail every 3 months, or log into your secure Medicare account to make sure claims are being filed in a timely way.
Time Frames To Submit A Claim
Please note the following time frames for submitting Medicare Advantage or commercial claims:
When Should I Be Filing A Claim For Myself
Another specific and unusual circumstance in which you may need to file a Medicare claim on your own is if your medical provider has not filed the claim within the appropriate timeline. Medicare claims are expected to be filed within 12 months of the original date of service.
How To Get Reimbursed From Medicare
To get reimbursement, you must send in a completed claim form and an itemized bill that supports your claim. It includes detailed instructions for submitting your request. You can fill it out on your computer and print it out. You can print it and fill it out by hand.
Obtain An Itemized Bill For Your Medical Treatment
Your itemized bill or bills for medical treatment proves your claims validity. Make sure your itemized bill contains the following information to ensure your claim is processed smoothly:
Billing Guidelines For Submitting A Roster Bill On A Paper Claim
Healthcare providers should follow the billing guidelines below when submitting roster bills to Humana:
Before You Submit A Claim
Payment of claims for MNT provided in the outpatient environment is dependent on several factors, including an individual’s benefits for MNT for their condition or reason , approved settings, and the network status of the RDN with the client/patient’s payer.
How To: Submit Claims To Priority Health
We accept claims from out-of-state providers by mail or electronically. Paper claims should be mailed to: Priority Health Claims, P.O. Box 232, Grand Rapids, MI 49501. Electronic claims set up and payer ID information is available here.
What to do if insurance company requests refund?
If the insurance company requests a refund because of the claim correction, you can post a different accounting adjustment, such as “Insurance Take-Back” and relink the payment to that adjustment.
What to do if a visit has wrong charges?
You may need to first handle any payments or adjustments attached to the charge as described above. Then you can delete the incorrect charges and post the correct charges. (As noted above, if the claim has already been sent, you’ll need to include the Payer Claim Control Number for resubmission.)
Can you delete an adjustment from insurance?
What About Adjustments From the Insurance Company?: If you are correcting a claim and there are already adjustments linked to charges you need to delete, you can safely delete them. Payments need to be accounted for later in your balance and reports, but adjustments do not.
Can a future check be reduced for an unrelated encounter?
That means that a future check, for an unrelated encounter, may be reduced for the amount of a payment sent to you in error. Follow the procedure below to post a temporary refund to hold the payments or adjustments for a claim you need to resubmit.
Can you adjust the place of service for charges on an encounter without deleting and reposting charges?
You can adjust the place of service for charges on an encounter without deleting and reposting charges.
Do you have to change the responsible party on a medical claim?
You may need to change the responsible party (an insurance policy, Medicaid, or personal) for some or all of the charges on a claim. You may also need to change the copay amount connected with the office visit charge.
Do you need to unlink an adjustment?
If payments and/or adjustments have already been posted against the charges, you may need to unlink the payments and post an accounting adjustment. The insurance payer will likely ask for the money refunded back as a “take back” on future ERAs. That means that a future check, for an unrelated encounter, may be reduced for the amount of a payment sent to you in error.
How to correct errors with correction tape?
Correct errors with correction tape by covering the incorrect information and writing the correct information on top of the tape. Do not use whiteout or highlight areas because they cannot be imaged correctly. Attach requested documentation prior to resubmitting. Photocopies must contain an original signature and date.
Can a remittance voucher be lost?
A remittance voucher may have been mailed but lost in transit. If the provider believes this is the case, call ACS Provider Inquiry. · If there is not a gap in the dates of remittance vouchers received, please call the Medicaid fiscal agent, Provider Inquiry. An associate will research the claim.
How to submit Medicare claims electronically?
How to Submit Claims: Claims may be electronically submitted to a Medicare Administrative Contractor (MAC) from a provider using a computer with software that meets electronic filing requirements as established by the HIPAA claim standard and by meeting CMS requirements contained in the provider enrollment & certification category area of this web site and the EDI Enrollment page in this section of the web site. Providers that bill institutional claims are also permitted to submit claims electronically via direct data entry (DDE) screens.
What chapter is Medicare claim processing manual?
For more information please contact your local MAC or refer to the Medicare Claims Processing Manual (IOM Pub.100-04), Chapter 24.
When a doctor submits a claim to be reimbursed for that test, what does Medicare determine?
When the doctor submits a claim to be reimbursed for that test, Medicare determines it was not medically necessary and denies payment of the claim. Denials of a request you or your doctor made for a health care service, supply or prescription. For example: Medicare determines that a wheelchair is not medically necessary for your condition.
Why does Medicare reject my doctor's recommendation?
For example: Your Medicare Part D drug plan rejects your doctor’s recommendation that you receive a discount on an expensive medication because the available lower-cost drugs are not effective for your condition.
What happens if you disagree with a Medicare decision?
If you disagree with a decision about one of your Medicare claims, you have the right to challenge that decision and file an appeal. Situations in which you can appeal include: Denials for health care services, supplies or prescriptions that you have already received. For example: During a medical visit your doctor conducts a test.
How to report Medicare not paying?
If you still have questions about a claim you think Medicare should not have paid, report your concerns to the Medicare at 1-800-MEDICARE. Make copies for your records of everything you are submitting. Send the MSN and any additional information to the address listed at the bottom on the last page of your MSN.
How long does it take to appeal a denied Medicare claim?
File your appeal within 120 days of receiving the Medicare Summary Notice (MSN) that lists the denied claim.
What to do if Medicare decision is not in your favor?
If that decision is not in your favor, you can proceed up the appeals levels to an administrative law judge, the Medicare Appeals Council and federal court.
How long does it take to appeal Medicare?
The final level of appeal is to the federal courts. You generally have 60 days to file appeals before an ALJ, the Medicare Appeals Council and to federal court.
When Do I Need to File A Claim?
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them anytime. You need to fill out an "Author…