Does Medicaid cover inpatient rehab?
Inpatient rehab programs may be covered by Medicaid, but the amount of coverage and eligible rehab centers will vary by state. Within inpatient or residential treatment, individuals stay onsite at the rehab facility for a number of days or weeks until treatment is completed.
How long will Medicare pay for a rehab facility?
Medicare covers inpatient rehab in a skilled nursing facility – also known as an SNF – for up to 100 days. Rehab in an SNF may be needed after an injury or procedure, like a hip or knee replacement. You usually pay nothing for days 1–20 in one benefit period, after the Part A deductible is met.
How much does inpatient rehab cost?
Some also offer memory care and escalating levels of health care, but not all do ... inpatient in a hospital for at least three days and your doctor feels you need specialized rehab or nursing care after discharge, Medicare may cover part of your costs ...
Will Medicare cover cost of hospital stay and rehabilitation?
Medicare Part A covers most of the cost of care when you stay at an inpatient rehabilitation facility (sometimes called a rehabilitation hospital).
How long does it take to get into an inpatient rehab facility?
What is part A in rehabilitation?
What is the benefit period for Medicare?
Does Medicare cover private duty nursing?
Does Medicare cover outpatient care?
See more
About this website
Which payment system is used for inpatient rehabilitation facilities?
prospective payment system (PPS)The Medicare program in 2002 instituted an inpatient rehabilitation facility (IRF) prospective payment system (PPS). IRFs are specialized hospitals or hospital units that provide intensive rehabilitation in an inpatient setting.
What is the inpatient rehabilitation facility prospective payment system?
Under the IRF prospective payment system (PPS), Medicare's payment rates are intended to cover all operating and capital costs that efficient facilities are expected to incur in furnishing intensive inpatient rehabilitation services.
How Much Does Medicare pay per day for rehab?
Medicare pays part of the cost for inpatient rehab services on a sliding time scale. After you meet your deductible, Medicare can pay 100% of the cost for your first 60 days of care, followed by a 30-day period in which you are charged a $341 co-payment for each day of treatment.
How are IRF reimbursed?
Reimbursement Rates – IRF Payment for IRFs is on a per discharge basis, with rates based on such factors as patient-case mix, rehabilitation impairment categories and tiered case-mix groups. Rates may be adjusted based on the length of stay, geographic area and demographic group.
How are LTCHs reimbursed?
Medicare pays 80 percent of the LTCHs' costs above the fixed loss amount, which is $33,015 in 2022. High-cost outlier payments are funded by reducing the base payment amount for all cases paid under the LTCH PPS by about 8 percent.
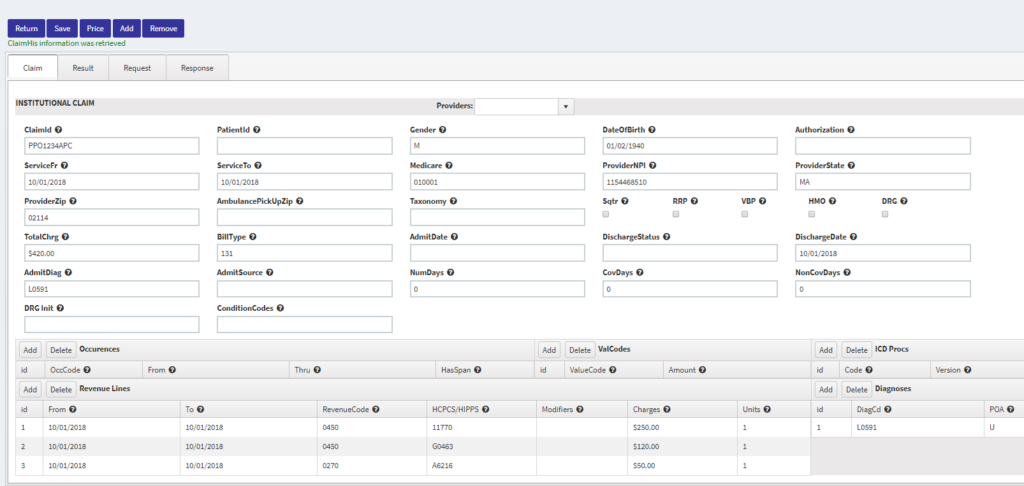
What is the CPT code for inpatient rehab?
Your procedure codes are correct (99221-99233), but the POS code for IP Rehab is 61.
What is the 3 day rule for Medicare?
The 3-day rule requires the patient have a medically necessary 3-consecutive-day inpatient hospital stay. The 3-consecutive-day count doesn't include the discharge day or pre-admission time spent in the Emergency Room (ER) or outpatient observation.
What is the 100 day rule for Medicare?
Medicare pays for post care for 100 days per hospital case (stay). You must be ADMITTED into the hospital and stay for three midnights to qualify for the 100 days of paid insurance. Medicare pays 100% of the bill for the first 20 days.
What is inpatient rehabilitation?
Inpatient rehabilitation generally refers to physician and therapy services you receive during a stay in a hospital. Outpatient rehabilitation refers to services you receive when you are not admitted to the hospital, such as physician services and physical, occupational, and speech therapy.
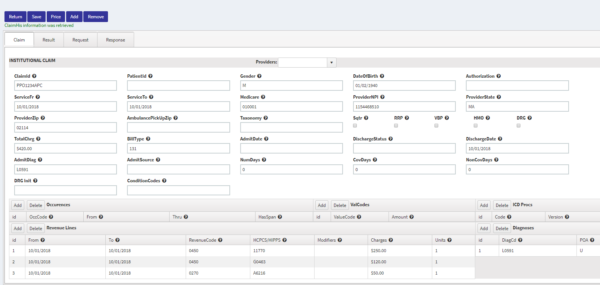
What is IRF claim?
An IRF is a hospital, or part of a hospital, that provides an intensive rehabilitation program to inpatients. Patients who are admitted must be able to tolerate an intensive level of rehabilitation services and benefit from a team approach.
What is the IRF 60% rule?
The 60% Rule is a Medicare facility criterion that requires each IRF to discharge at least 60 percent of its patients with one of 13 qualifying conditions.
What is the CMS 60% rule?
The 60% Rule The current “60% rule” stipulates that in order for an IRF to be considered for Medicare reimbursement purposes, 60% of the IRF's patients must have a qualifying condition. There are currently 13 such conditions, including, stroke, spinal cord or brain injury and hip fracture, among others.
Fact Sheet: Inpatient Rehabilitation Facilities (IRFs) | AHA
Inpatient rehabilitation facilities (IRFs) have faced significant scrutiny from Congress and the Centers for Medicare & Medicaid Services (CMS) in recent years, which has led to multiple interventions, including strict criteria for IRF patients, multiple payment cuts and other policy restrictions. Collectively, these interventions have reshaped the population treated in IRFs by dramatically ...
Fact Sheet #1 Inpatient Rehabilitation Facility Classification ... - CMS
5 requirement for cost reporting periods beginning on or after July 1, 2004 and before July 1, 2005, is 50 percent; for cost reporting periods beginning on or after July 1, 2005 and
Inpatient Rehabilitation Facilities | CMS
This page provides basic information about being certified as a Medicare and/or Medicaid Inpatient Rehabilitation Facility (IRF) and includes links to applicable laws, regulations, and compliance information.
Medicare Coverage for Inpatient Rehabilitation
Medicare covers inpatient rehabilitation in a skilled nursing facility and inpatient rehabilitation facility differently. Learn about the rules and costs.
How Long Does Medicare Pay for Rehab?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. His work has been featured in outlets such as Vox, MSN, and The Washington Post, and he is a frequent contributor to health care and finance blogs.
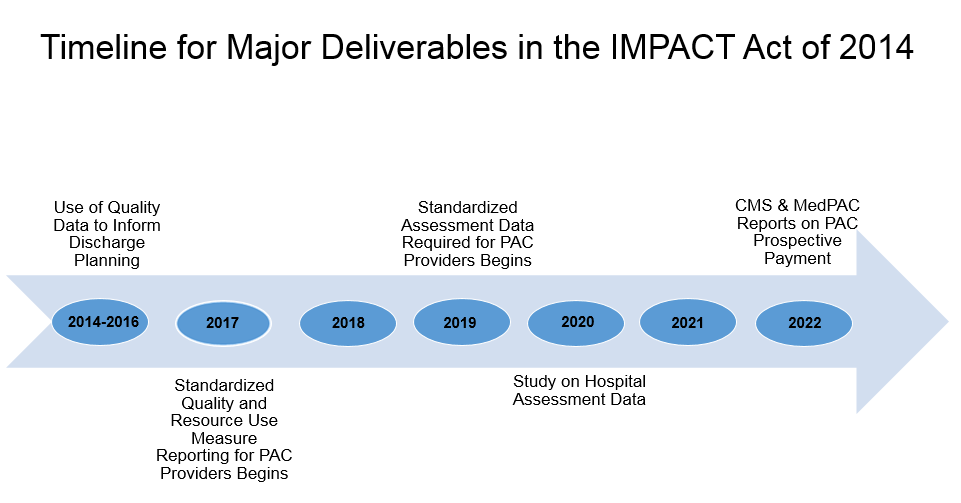
When will CMS 1748-P be released?
CMS-1748-P: Medicare Program; Inpatient Rehabilitation Facility Prospective Payment System for Federal Fiscal Year 2022 and Updates to the IRF Quality Reporting Program is on public display at the Office of Federal Register and will publish on April 12, 2021. The rule and associated wage index file is available on the web page
What is section 3004?
Section 3004 of the Affordable Care Act. CMS has created a website to support Section 3004 of the Affordable Care Act, Quality Reporting for Long Term Care Hospitals, Inpatient Rehabilitation Hospitals and Hospice Programs.
How long does Medicare cover inpatient rehab?
Medicare covers inpatient rehab in a skilled nursing facility – also known as an SNF – for up to 100 days. Rehab in an SNF may be needed after an injury or procedure, like a hip or knee replacement.
What is an inpatient rehab facility?
An inpatient rehabilitation facility (inpatient “rehab” facility or IRF) Acute care rehabilitation center. Rehabilitation hospital. For inpatient rehab care to be covered, your doctor needs to affirm the following are true for your medical condition: 1. It requires intensive rehab.
What is Medicare Part A?
Published by: Medicare Made Clear. Medicare Part A covers medically necessary inpatient rehab (rehabilitation) care , which can help when you’re recovering from serious injuries, surgery or an illness. Inpatient rehab care may be provided in of the following facilities: A skilled nursing facility.
How long does it take to get Medicare to cover rehab?
The 3-day rule for Medicare requires that you are admitted to the hospital as an inpatient for at least 3 days for rehab in a skilled nursing facility to be covered. You must be officially admitted to the hospital by a doctor’s order to even be considered an inpatient, so watch out for this rule. In cases where the 3-day rule is not met, Medicare ...
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
How much does Medicare pay for day 150?
You pay 100 percent of the cost for day 150 and beyond in a benefit period. Your inpatient rehab coverage and costs may be different with a Medicare Advantage plan, and some costs may be covered if you have a Medicare supplement plan. Check with your plan provider for details.
What is the medical condition that requires rehab?
To qualify for care in an inpatient rehabilitation facility, your doctor must state that your medical condition requires the following: Intensive rehabilitation. Continued medical supervision.
How long does Medicare cover inpatient hospital care?
The inpatient hospital benefit covers 90 days of care per episode of illness with an additional 60-day lifetime reserve.
How many days does Medicare cover?
Medicare allows 90 covered benefit days for an episode of care under the inpatient hospital benefit. Each patient has an additional 60 lifetime reserve days. The patient may use these lifetime reserve days to cover additional non-covered days of an episode of care exceeding 90 days. High Cost Outlier.
How long does it take to travel between a hospital and a like hospital?
The hospital is rural and because of distance, posted speed limits, and predictable weather conditions, travel time between the hospital and the nearest like hospital is at least 45 minutes. A like hospital is a hospital that provides short-term, acute care.
When does home health care begin?
Home health care, when the patient gets clinically related care that begins within 3 days after a hospital stay. Rehabilitation distinct part units located in an acute care hospital or a CAH. Psychiatric distinct part units located in an acute care hospital or a CAH. Cancer hospitals.
What is a physician order?
The physician order meets 42 CFR Section 412.3 (b), which states: A qualified, licensed physician must order the patient’s admission and have admitting privileges at the hospital as permitted by state law. The physician is knowledgeable about the patient’s hospital course, medical plan of care, and current condition.
How long does Medicare require for rehabilitation?
In some situations, Medicare requires a 3-day hospital stay before covering rehabilitation. Medicare Advantage plans also cover inpatient rehabilitation, but the coverage guidelines and costs vary by plan. Recovery from some injuries, illnesses, and surgeries can require a period of closely supervised rehabilitation.
What are the conditions that require inpatient rehabilitation?
Inpatient rehabilitation is often necessary if you’ve experienced one of these injuries or conditions: brain injury. cancer. heart attack. orthopedic surgery. spinal cord injury. stroke.
How long does it take for a skilled nursing facility to be approved by Medicare?
Confirm your initial hospital stay meets the 3-day rule. Medicare covers inpatient rehabilitation care in a skilled nursing facility only after a 3-day inpatient stay at a Medicare-approved hospital. It’s important that your doctor write an order admitting you to the hospital.
How many hours of therapy per day for rehabilitation?
access to a registered nurse with a specialty in rehabilitation services. therapy for at least 3 hours per day, 5 days per week (although there is some flexibility here) a multidisciplinary team to care for you, including a doctor, rehabilitation nurse, and at least one therapist.
Does Medicare cover knee replacement surgery?
The 3-day rule does not apply for these procedures, and Medicare will cover your inpatient rehabilitation after the surgery. These procedures can be found on Medicare’s inpatient only list. In 2018, Medicare removed total knee replacements from the inpatient only list.
Does Medigap cover coinsurance?
Costs with Medigap. Adding Medigap (Medicare supplement) coverage could help you pay your coinsurance and deductible costs. Some Medigap plans also offer additional lifetime reserve days (up to 365 extra days). You can search for plans in your area and compare coverage using Medicare’s plan finder tool.
Does Medicare cover rehab?
Medicare Part A covers your inpatient care in a rehabilitation facility as long as your doctor deems it medically necessary. In addition, you must receive care in a facility that’s Medicare-approved. Depending on where you receive your inpatient rehab therapy, you may need to have a qualifying 3-day hospital stay before your rehab admission.
What is an inpatient hospital?
Inpatient hospital care. You’re admitted to the hospital as an inpatient after an official doctor’s order, which says you need inpatient hospital care to treat your illness or injury. The hospital accepts Medicare.
What does Medicare Part B cover?
If you also have Part B, it generally covers 80% of the Medicare-approved amount for doctor’s services you get while you’re in a hospital. This doesn't include: Private-duty nursing. Private room (unless Medically necessary ) Television and phone in your room (if there's a separate charge for these items)
What are Medicare covered services?
Medicare-covered hospital services include: Semi-private rooms. Meals. General nursing. Drugs as part of your inpatient treatment (including methadone to treat an opioid use disorder) Other hospital services and supplies as part of your inpatient treatment.
How much does Medicare pay for inpatient care?
As an inpatient, you will pay 20% of the hospital bill once you have met the deductible for Medicare Part A. Medicare insurance sets the rates for services received as an inpatient in a hospital by diagnostic categories and conditional circumstances of the hospital itself.
How long does a hospital stay in Medicare?
In order to be considered an inpatient stay, a recipient must be admitted for care by a doctor’s orders and that care must last longer than 24 hours.
What is disproportionate share hospital?
Hospitals that treat a large volume of low-income patients are classified as disproportionate share hospitals (DSH) and qualify for a higher percentage payment than hospitals without this classification. Teaching hospitals and hospitals in rural areas can also receive add-ons that increase the rate Medicare pays them.
Is observation only considered outpatient care?
Some patients may be admitted for observation-only services on an overnight basis, but this is classified as outpatient care rather than inpatient care. In those situations, Medicare Part B payment terms apply, which means recipients are accountable for their Part B deductible and corresponding copayment or coinsurance amounts.
How long does it take to get into an inpatient rehab facility?
You’re admitted to an inpatient rehabilitation facility within 60 days of being discharged from a hospital.
What is part A in rehabilitation?
Inpatient rehabilitation care. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
What is the benefit period for Medicare?
benefit period. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services. A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row.
Does Medicare cover private duty nursing?
Medicare doesn’t cover: Private duty nursing. A phone or television in your room. Personal items, like toothpaste, socks, or razors (except when a hospital provides them as part of your hospital admission pack). A private room, unless medically necessary.
Does Medicare cover outpatient care?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.