RREs using the DDE method must submit claim information using the Section 111 Coordination of Benefits Secure Website (COBSW) one report at a time, within 45 calendar days of the Total Payment Obligation to Claimant (TPOC) or assumption or termination of Ongoing Responsibility for Medicals (ORM).
Full Answer
Is there a Medicare program manual for DDE?
However, since the Medicare program is constantly changing, it is the responsibility of each provider to remain abreast of changes in the Medicare program. This manual serves as a reference and is ideal for users (both experienced and inexperienced) of DDE.
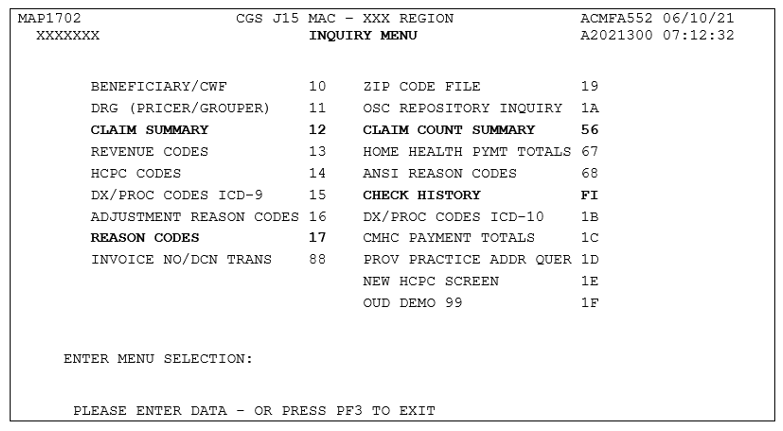
How can I see Medicare secondary payer claims in DDE?
DDE. Note: You will be able to see Medicare Secondary Payer claims in the claims history (Inquiry option 12), but the claims cannot process through DDE. 14. How can I find out if a revenue code is valid for Medicare? a. A listing of UB-04 revenue codes is found in the CMS Internet Only Manuals (IOM)
What is DDE for Medicare&Medicaid?
Medicare & Medicaid (CMS) to be used for Medicare Part A claims and Part B facility claims. DDE is a real-time FISS application giving providers interactive access for inquiries, claims entry and correction purposes. It also is a valuable tool for providers who use batch submissions to transmit electronic claims,
What are the status/location codes for Medicare DDE?
8 Status/Location Codes The Status/Location (S/LOC) code for Medicare DDE screens indicates whether a particular claim is paid, suspended, rejected, returned for correction, etc. The six-character alphanumeric code is made up of a combination of four sub-codes: the claim status, processing type, location, and additional location information.
What is DDE in billing?
DDE is a real-time Fiscal Intermediary Shared System (FISS) application giving providers interactive access for inquiries, claims entry and correction purposes. Functions include: Eligibility. Claims: Submission, Status, Corrections, Cancellations, Related Attachments and Roster Billing.
What is DDE for Medicare?
The Direct Data Entry (DDE) system was designed as an integral part of the Fiscal Intermediary Standard System (FISS) to be used by all Medicare A providers. DDE will offer various tools to help providers obtain answers to many questions without contacting Medicare Part A via telephone or written inquiry.
What type of Medicare claims is DDE Fiss used for?
The Fiscal Intermediary Shared System (FISS) is the processing system designated by the Centers for Medicare & Medicaid (CMS) to be used for Medicare Part A claims and Part B facility claims. DDE is a real-time FISS application giving providers interactive access for inquiries, claims entry and correction purposes.
How do I correct a Medicare claim in DDE?
Make your correction and press F9. Repeat this process (F1, F3, F9) until the claim has been corrected, and you are returned to Map 1741. - More than one reason code may appear in the lower left-hand corner of Page 01 of the claim. Pressing F1 displays the narrative for the first reason code.
How do I get access to DDE?
To access DDE, a request must be submitted electronically by the Authorized Signer using the DDE Electronic Access Request Form. Each facility will have an Authorized Signer. The DDE Authorized Signer is determined by the facility.
What is included in an electronic remittance advice?
An electronic remittance advice, or ERA, is an explanation from a health plan to a provider about a claim payment. The ERA provides payment information about the transfer of funds and payment processing from a health plan to a health care provider's bank, or the explanation of benefits or remittance advice.
What is Medicare Fiss?
The Fiscal Intermediary Standard System (FISS) is the standard Medicare Part A. claims processing system. It allows you to perform the following functions: • Enter, correct, adjust, or cancel your Medicare home health and hospice. billing transactions.
How many major methods are there for transmitting claims electronically?
three major methodsReview the three major methods used to transmit claims electronically: direct transmission to the payer, clearinghouse use, and direct data entry.
What does T B9997 mean?
The Claims Correction Menu (FISS Main Menu option 03) allows you to: ☑ Correct claims in the return to provider (RTP) status/location (T B9997) ☑ Adjust paid or rejected claims. ☑ Cancel paid claims or Requests for Anticipated Payments (RAPs)
How do I check my DDE ADR?
How Do I Check DDE for an ADR?Enter your national provider identifier (NPI) and the status location (S B6000/S B6001).Choose Claims option 12.Place an "S" in the SEL field in front of the desired claim and press enter. ... See the DDE User's Manual for Medicare Part A for additional information on accessing.
How do I correct a Medicare billing error?
If the issue is with the hospital or a medical provider, call them and ask to speak with the person who handles insurance. They can help assist you in correcting the billing issue. Those with Original Medicare (parts A and B) can call 1-800-MEDICARE with any billing issues.
What is the resubmission code for a corrected claim?
Complete box 22 (Resubmission Code) to include a 7 (the "Replace" billing code) to notify us of a corrected or replacement claim, or insert an 8 (the “Void” billing code) to let us know you are voiding a previously submitted claim.
Who is responsible for assigning user IDs and terminating access for DDE?
Noridian is responsible for assigning user IDs and terminating access for DDE. The MCPS Form is used for all security changes/updates.
How long does it take to check a DDE?
DDE allows providers to check eligibility and claim status (paid, denied or pending). Providers can check the status of claims within three days of a successful transmission. Navigation.
Is DDE available on weekends?
DDE will not be available during quarterly releases, holidays, and system purge weekends.
What is the purpose of the DDE manual?
The purpose of this manual is to give DDE users an understanding of the information available in the
Who must request access from Noridian Healthcare Solutions?
The facility must request access from Noridian Healthcare Solutions (Noridian) for each user. Users
What is a reason code?
The Reason Code inquiry screens list the reason codes assigned to a claim to define something about the . claim. Sometimes the reason code simply gives information about the claim, such as it is a finalized . claim. In other situations, the reason code defines why a claim and/or line item was denied, rejected, or .
How to contact AHA about UB-04?
UB-04 Data Specifications, contact AHA at (312) 893-6816. You may also contact AHA at
Can descriptions be removed?
descriptions may not be removed, copied, or utilized within any software, product, service, solution or
What happens when a claim is submitted to DDE?
When a claim has been submitted, the DDE submitter must monitor the Status and Disposition of the claim report on the DDE Claim Listing page to see if the claim was accepted or not and react accordingly.
What does DDE monitor?
When a claim has been submitted, the DDE submitter must monitor the Status and Disposition of the claim report on the DDE Claim Listing page to see if the claim was accepted or not and react accordingly.
What field do DDE submitters need to monitor?
DDE submitters must monitor the value returned in the Disposition field which will show them the results of processing the claim report.
Why was the DDE 111 module created?
This module was created to share best practices to be used by DDE submitters so that they are successful in submitting Section 111 claim reports.
What is the 01 disposition?
The 01 Disposition shows that the claim report was accepted by the BCRC, the injured party was identified as a Medicare beneficiary and ORM was indicated.
When do RREs have to submit information for self-insurance?
RREs must submit information for all liability insurance (including self-insurance), no-fault insurance, and workers’ compensation claims involving a Medicare beneficiary as the injured party where ORM payments exist as of January 1, 2010 and subsequent , regardless of the date of an initial acceptance of payment responsibility.
Does the RRE maintain a record of the final disposition received?
It is also recommended that the RRE maintain a record of the final Disposition received for the claim report which will be displayed on the Claim Listing page when the Status is Completed.
How many chapters are there in the FISS DDE guide?
FISS DDE Guide – This guide includes five different chapters with information about how to access the DDE screens, and details, including screen prints and field descriptions, about each of the main menu selections.
Does CGS EDI support FISS DDE?
The CGS EDI department does not provide support for your connectivity product; therefore, you will need to contact your connectivity vendor for any issues related to your direct connection. Please review the following resources for details information about FISS DDE.