How would repealed Affordable Care Act affect health care and jobs?
How would repealing the Affordable Care Act affect health care and jobs in your state? Across the country, 29.8 million people would lose their health insurance if the Affordable Care Act were repealed—more than doubling the number of people without health insurance.
How many people would lose their health insurance if Obamacare is repealed?
Across the country, 29.8 million people would lose their health insurance if the Affordable Care Act were repealed—more than doubling the number of people without health insurance. And 1.2 million jobs would be lost —not just in health care but across the board. How many people would lose their health insurance if the ACA were repealed?
Will repealing the ACA's Medicare Advantage payment changes increase Medicare spending?
Repealing the ACA’s Medicare Advantage payment changes would be expected to: Increase total Medicare spending as a result of increasing payments to Medicare Advantage plans relative to spending under traditional Medicare.
How has the Affordable Care Act changed Medicaid's role?
ISSUE: The Affordable Care Act enhanced Medicaid's role as a health care purchaser by expanding eligibility and broadening the range of tools and strategies available to states. All states have embraced delivery and payment reform as basic elements of their programs.
Will Medicare be affected if the ACA is repealed?
Repealing the payroll tax increases would reduce revenues to the Medicare Hospital Insurance Trust Fund, which covers the costs of beneficiaries' hospital visits and is currently projected to become insolvent in 2024.
How has the Affordable Care Act affect Medicare?
Cost savings through Medicare Advantage. The ACA gradually reduced costs by restructuring payments to Medicare Advantage, based on the fact that the government was spending more money per enrollee for Medicare Advantage than for Original Medicare.
What would happen if the ACA was repealed?
The health insurance industry would be upended by the elimination of A.C.A. requirements. Insurers in many markets could again deny coverage or charge higher premiums to people with pre-existing medical conditions, and they could charge women higher rates.
Who benefits from repealing ACA?
The Congressional Budget Office (CBO) has estimated that full repeal of the ACA would increase Medicare spending by $802 billion from 2016 to 2025. 1 Full repeal would increase spending primarily by restoring higher payments to health care providers and Medicare Advantage plans.
Is Medicare considered under the Affordable Care Act?
Obamacare's expanded Medicare preventive coverage applies to all Medicare beneficiaries, whether they have Original Medicare or a Medicare Advantage plan.
Is Medicare a part of the Affordable Care Act?
The 2010 Affordable Care Act (ACA) included many provisions affecting the Medicare program and the 57 million seniors and people with disabilities who rely on Medicare for their health insurance coverage.
What would happen if Medicare ended?
Payroll taxes would fall 10 percent, wages would go up 11 percent and output per capita would jump 14.5 percent. Capital per capita would soar nearly 38 percent as consumers accumulated more assets, an almost ninefold increase compared to eliminating Medicare alone.
What effect will the repeal of the Patient Protection and Affordable Care Act have on health insurance markets?
Across the country, 29.8 million people would lose their health insurance if the Affordable Care Act were repealed—more than doubling the number of people without health insurance. And 1.2 million jobs would be lost—not just in health care but across the board.
What are the problems with the Affordable Care Act?
The Problem: Affordability The ACA set standards for “affordability,” but millions remain uninsured or underinsured due to high costs, even with subsidies potentially available. High deductibles and increases in consumer cost sharing have chipped away at the affordability of ACA-compliant plans.
Why we should not repeal the ACA?
Repeal Would Worsen Racial Disparities Black and Hispanic people were also more likely to avoid using health care due to cost. While the ACA did not eliminate these gaps, it narrowed disparities in both coverage and access to care significantly, and striking down the law would widen them once again.
What are the challenges involved in repealing and replacing the Affordable Care Act?
As repeal-and-replace efforts persist, the EHBs face three main challenges: (1) regulatory implementation of the EHBs, (2) struggling individual and small-group markets in many state insurance exchanges, and (3) the Trump administration's push for selling health insurance across state lines.
Why did ACA fail?
It largely failed. Health insurance markets are only afloat because of massive federal subsidies and premiums and out-of-pocket obligations significantly increased for families. While the ACA has led to about 13 million more people with Medicaid, many more have been harmed.
What would be expected from repealing the ACA?
Repealing the ACA’s Medicare benefit improvements would be expected to: Reduce Medicare Part B spending for preventive services and reduce Part D spending on costs in the coverage gap. Increase beneficiary cost sharing for Part B preventive benefits.
How would ACA repeal affect the solvency of the Medicare Hospital Insurance trust fund?
This would result from higher spending for Part A services due to higher payments to Part A service providers (such as hospitals) and Medicare Advantage plans for services provided under Part A, along with reduced revenues, if the additional 0.9 percent payroll tax on high earners is repealed. As a result, Medicare would not be able to fulfill its obligation to pay for all Part A-covered benefits within a shorter period of time if the ACA is repealed than if the law is retained.
What would happen if Medicare spending increased?
The increase in Medicare spending would likely lead to higher Medicare premiums, deductibles, and cost sharing for beneficiaries, and accelerate the insolvency of the Medicare Part A trust fund. Policymakers will confront decisions about the Medicare provisions in the ACA in their efforts to repeal and replace the law.
How much will Medicare increase over 10 years?
Increase Part A and Part B spending. CBO has estimated that roughly $350 billion 3 of the total $802 billion in higher Medicare spending over 10 years could result from repealing ACA provisions that changed provider payment rates in traditional Medicare.
What is CMS in Medicare?
Through a new Center for Medicare & Medicaid Innovation (CMMI, or Innovation Center) within the Centers for Medicare & Medicaid Services (CMS), the ACA directed CMS to test and implement new approaches for Medicare to pay doctors, hospitals, and other providers to bring about changes in how providers organize and deliver care. The ACA authorized the Secretary of Health and Human Services to expand CMMI models into Medicare if evaluation results showed that they either reduced spending without harming the quality of care or improved the quality of care without increasing spending. CMMI received an initial appropriation of $10 billion in 2010 for payment and delivery system reform model development and evaluation, and the ACA called for additional appropriations of $10 billion in each decade beginning in 2020.
What is the ACA payment?
Payments to Health Care Providers. The ACA reduced updates in Medicare payment levels to hospitals, skilled nursing facilities, hospice and home health providers, and other health care providers. The ACA also reduced Medicare Disproportionate Share Hospital (DSH) payments that help to compensate hospitals for providing care to low-income ...
Why is the ACA important?
The Medicare provisions of the ACA have played an important role in strengthening Medicare’s financial status for the future, while offsetting some of the cost of the coverage expansions of the ACA and also providing some additional benefits to people with Medicare.
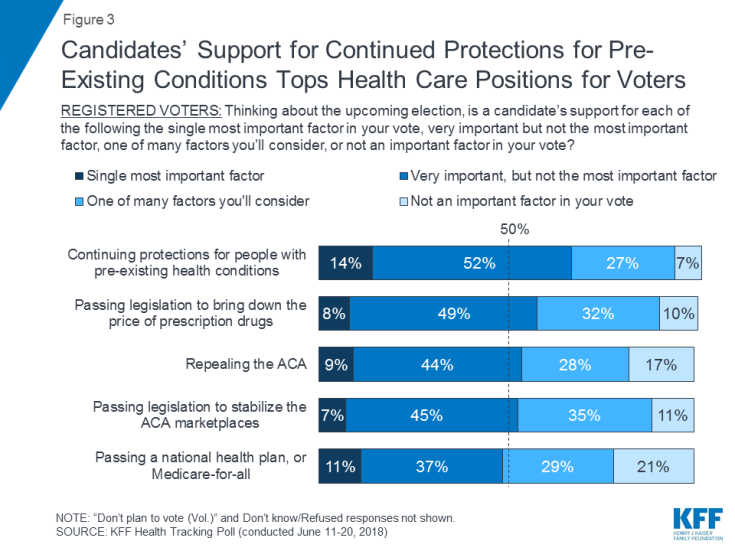
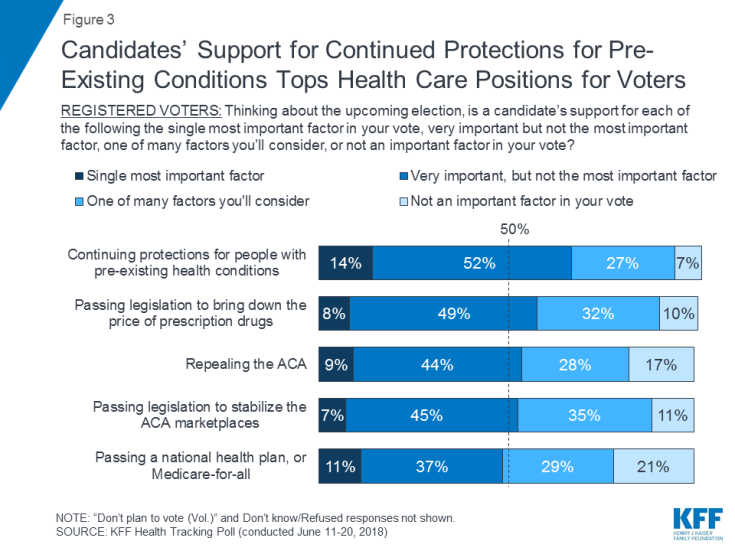
How many Americans support repeal of Obamacare?
Supporters of Obamacare also note that a recent survey by the Kaiser Family Foundation found that only a quarter of Americans support total repeal. Medicare, of course, is overwhelmingly popular with the 57 million seniors and disabled Americans who depend on it.
Who is the speaker of the House who wants to repeal Obamacare?
David Certner, a legislative expert with AARP, said the lack of specifics in Republican calls to repeal Obamacare were of great concern, as are proposals by House Speaker Paul Ryan to provide Medicare enrollees with premium-support payments, or vouchers, and let them buy health insurance in the private market.
How many votes are needed to repeal the individual mandate?
For example, while 60 votes would be required in the Senate to repeal the individual mandate, the financial penalties for not getting insurance might be removed via a reconciliation measure. Without penalties, the mandate would lack enforcement power and could be effectively killed without formal changes to the law.
What would happen if people didn't get health insurance?
If people were not required to get health insurance and insurance companies could not reject someone for coverage on health grounds, then only healthy people would get insurance and insurance companies could not make money insuring sicker persons unless they charged them unaffordably high premiums.
When is Medicare Advantage disenrollment period?
For those who’ve signed up for a Medicare Advantage plan, there also is a Medicare Advantage disenrollment period that runs from Jan. 1 to Feb. 14. You have the option then of moving into basic Medicare (Parts A and B) and also getting a stand-alone Part D prescription drug plan.
Can insurance companies deny coverage based on pre-existing conditions?
Health care and insurance experts don’t see how any serious effort to unwind the law could proceed if it kept both the individual mandate, which requires people be insured, and the ban on insurers being able to deny coverage to a person based on pre-existing medical conditions.
Will the Affordable Care Act be repealed?
It now looks like Republicans want to approve repealing the ACA early next year. Replacing it, however, could take years, assuming this is even possible.
How many people would lose their health insurance if the Affordable Care Act was repealed?
A cross the country, 29.8 million people would lose their health insurance if the Affordable Care Act were repealed—more than doubling the number of people without health insurance. And 1.2 million jobs would be lost —not just in health care but across the board.
How would losing health insurance affect the economy?
By helping pick up the tab for individual insurance and expanding coverage on Medicaid, the ACA has helped millions of Americans afford their care. If this support were withdrawn, people would have less money to spend on other basic necessities like food and rent. Fewer dollars spent at grocery stores and other businesses means 1.2 million jobs would be lost.
How much of Medicare Part C is spent on other health care?
Under the ACA, Medicare Advantage (Medicare Part C) plans are required to spend at least 85% of the revenue generated by plan premiums on other plan health care costs, and not toward company profits or overhead.
Does Medicare pay for a wellness exam?
Because of provisions within the ACA, Medicare beneficiaries pay no deductibles or coinsurance for certain preventive screenings for conditions such as cancer, heart disease and diabetes. Annual Medicare wellness exams are free of charge, as are flu shots and certain other vaccines.
How did the ACA help the states?
The ACA encouraged states to view Medicaid as a vehicle for health care transformation in other ways. “Health homes,” for example, represent an explicit effort on the part of Congress to give states additional improvement tools for their most vulnerable patients. 6 Additionally, many of the ACA’s delivery and payment reforms—initially targeted chiefly at Medicare—were incorporated into Medicaid through regulations that gave states additional flexibility. These reforms include: promoting payment reform; 7 promoting use of integrated delivery and accountable care models 8 that already have begun to show measurable savings; 9 establishing a “state innovation model” initiative within the Center for Medicare and Medicaid Innovation; 10 and establishing a Medicaid Innovation Accelerator program, which aims to ensure that innovations in care are more rapidly disseminated to all states, with technical support available. 11 The ACA also acted to promote Medicaid managed care plans to better care for high-need, high-cost beneficiaries and to improve health care quality, efficiency, and health outcomes for people eligible for both Medicare and Medicaid. 12,13
What impact did the American Health Care Act have on the health care system?
The American Health Care Act, reported by the House Energy and Commerce and Ways and Means committees in March 2017, would eliminate the ACA’s enhanced funding to support the expansion population, among other changes.
How many people are on medicaid in 2016?
According to government statistics, as of October 2016, Medicaid enrollment surpassed 74 million. More than 17 million people—an increase of 30 percent—gained eligibility since October 2013, just before full implementation of the ACA. Although 19 states have not yet chosen to adopt the ACA’s adult Medicaid eligibility expansion, ...
How does fixed limit Medicaid funding help?
At least in theory, fixed limits on per person Medicaid funding could help foster innovation by encouraging strategies that substitute less costly but equally appropriate care, reduce excessive use of services of questionable value, or lower the price paid for care.
What are the implications of the House bill?
Cuts of the type contained in the House bill carry major implications for payment and delivery reform. First and foremost, the CBO projects that elimination of enhanced funding for the ACA expansion population would lead states to roll back their expansions or forgo expansion in the first place, ultimately reducing the number of people covered by 17 percent by 2026—14 million fewer people annually. Without coverage there can be no delivery and payment reform.
How would Medicaid be transformed?
House of Representatives that would transform Medicaid, not only by eliminating enhanced federal funding for eligibility expansion but also by reducing the amount of funding states receive to run their traditional programs.
Is Medicaid more expensive per capita?
On a per capita basis, Medicaid is significantly less costly than comparable coverage purchased in the employer market. Even without the introduction of federal spending caps, experts had projected that future Medicaid per person spending would be lower than spending for comparable services under either Medicare or private insurance. Medicaid spending is largely explained by enrollment. From 1975 to 2012, over 70 percent of Medicaid spending growth was linked to enrollment rather than rising costs per enrollee; since 2012, Medicaid spending growth has been spurred by a 30 percent increase in program enrollment coupled with enhanced funding for the expansion population. 22
What would happen if the ACA was left in place?
Leaving the ACA’s market reforms in place would limit insurers’ ability to use strategies that were common before the ACA was enacted. For example, insurers would not be able to vary premiums to reflect an individual’s health care costs or offer health insurance plans that exclude coverage of preexisting conditions, plans that do not cover certain types of benefits (such as maternity care), or plans with very high deductibles or very low actuarial value (plans paying a very low share of costs for covered services).
How long after the repeal of the Medicaid expansion did the subsidies take effect?
The bill’s effects on insurance coverage and premiums would be greater once the repeal of the Medicaid expansion and the subsidies for insurance purchased through the marketplaces took effect, roughly two years after enactment. Effects on Insurance Coverage.
How will H.R. 3762 affect health insurance?
By CBO and JCT’s estimates, enacting H.R. 3762 would increase the number of people without health insurance coverage by about 27 million in the year following the elimination of the Medicaid expansion and marketplace subsidies and by 32 million in 2026, relative to the number of uninsured people expected under current law. (The number of people without health insurance would be smaller if, in addition to the changes in H.R. 3762, the insurance market reforms mentioned above were also repealed. In that case, the increase in the number of uninsured people would be about 21 million in the year following the elimination of the Medicaid expansion and marketplace subsidies; that figure would rise to about 23 million in 2026.)
What would happen if we eliminated the penalty for not having health insurance?
But eliminating the penalty for not having health insurance would reduce enrollment and raise premiums in the nongroup market. Eliminating subsidies for insurance purchased through the marketplaces would have the same effects because it would result in a large price increase for many people.
How would H.R. 3762 affect premiums?
3762’s changes into their premium pricing in the first new plan year after enactment. The majority of that increase would stem from repealing the penalties associated with the individual mandate. Doing so would both reduce the number of people purchasing health insurance and change the mix of people with insurance—tending to cause smaller reductions in coverage among older and less healthy people with high health care costs and larger reductions among younger and healthier people with low health care costs. Thus, average health care costs among the people retaining coverage would be higher, and insurers would have to raise premiums in the nongroup market to cover those higher costs. Lower participation by insurers in the nongroup market would place further upward pressure on premiums because the market would be less competitive.
What was the impact of H.R. 3762?
3762, the Restoring Americans’ Healthcare Freedom Reconciliation Act of 2015, which would repeal portions of the Affordable Care Act (ACA) eliminating, in two steps, the law’s mandate penalties and subsidies but leaving the ACA’s insurance market reforms in place. At that time, CBO and JCT offered a partial assessment of how H.R. 3762 would affect health insurance coverage, but they had not estimated the changes in coverage or premiums that would result from leaving the market reforms in place while repealing the mandate penalties and subsidies. This document—prepared at the request of the Senate Minority Leader, the Ranking Member of the Senate Committee on Finance, and the Ranking Member of the Senate Committee on Health, Education, Labor, and Pensions provides such an estimate.
How many people will not have medicaid in 2026?
The estimated increase of 32 million people without coverage in 2026 is the net result of roughly 23 million fewer with coverage in the nongroup market and 19 million fewer with coverage under Medicaid, partially offset by an increase of about 11 million people covered by employment-based insurance.
Which case challenged the Affordable Care Act?
The case, California v. Texas, which was filed by 20 Republican-leaning states, challenges whether the Affordable Care Act can exist without the individual mandate to buy health insurance. A Republican-controlled Congress removed the financial penalty for those without insurance in 2017.
How long will Medicare be insolvent?
The Congressional Budget Office estimates that reversing those changes would cost the program $700 billion over 10 years. “Medicare would face almost immediate insolvency,” predicts the Senior Citizens League in a report.
What is the Medicare doughnut hole?
The Medicare Doughnut Hole Returns. Since 2011 the ACA has been steadily closing the prescription drug coverage gap , known as the doughnut hole, in Medicare Part D by requiring drug manufacturers and insurers to pick up more of the cost.
Does Medicare Advantage pay for chemotherapy?
The ACA requires Medicare Advantage plans to spend 85% of premium dollars on health care, not profits or overhead. The plans also can’t charge more than traditional Medicare for chemotherapy, renal dialysis, skilled nursing care and other specialized services. (Beginning in 2021, Advantage plans must accept enrollees with end stage renal disease.)
Will Medicare premiums rise faster?
Medicare Premiums and Medicare Deductibles Will Rise Faster. Curbing provider payments also lowered costs for seniors, helping to keep Medicare Part A deductibles and copayments in check. Similarly, Part B premiums and deductibles are much lower than projected before the ACA became law.