The “primary payer” pays what it owes on your bills first, and then your provider sends the rest to the “secondary payer” to pay. In some cases, there may also be a “third payer.” Whether Medicare pays first depends on a number of things.
Full Answer
Who pays first in a Medicare case?
If you have Medicare and other health insurance or coverage, each type of coverage is called a "payer." When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) to pay.
Does Medicare pay first when you become eligible?
If you originally got Medicare due to your age or a disability other than ESRD, and your group health plan was your primary payer, then it still pays first when you become eligible because of ESRD.
How do I find out who pays first for Medicare?
Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should've made. Find out which insurance pays first. Call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627) if: You have questions about who pays first.
Does Medicare pay first and no-fault insurance second?
No-fault insurance or liability insurance pays first and Medicare pays second. No-fault insurance pays for health care services resulting from injury to you or damage to your property in an accident, regardless of who is at fault for causing the accident.
Will Medicare pay secondary if primary denies?
If your primary insurance denies coverage, secondary insurance may or may not pay some part of the cost, depending on the insurance. If you do not have primary insurance, your secondary insurance may make little or no payment for your health care costs.
Does Medicare pay anything toward eyeglasses?
Generally, Original Medicare does not cover routine eyeglasses or contact lenses. However, following cataract surgery that implants an intraocular lens, Medicare Part B helps pay for corrective lenses; one pair of eyeglasses or one set of contact lenses provided by an ophthalmologist.
Can I have dual coverage with VSP?
DUAL COVERAGE A married enrollee whose spouse is also an enrollee under his/her own VSP Plan may coordinate benefits between their respective VSP Plans. Such “dual coverage” will be subject to the same procedures and limitations applicable to coordination of benefits with non-VSP plans.
Is Medicare always primary?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
How often will Medicare pay for glasses?
Medicare only pays for one new pair of eyeglasses per lifetime, per eye you have surgery on. So, if you have surgery to correct one eye, you can get a pair of eyeglasses at that time. If you have cataract surgery on another eye at a later time, you can get another new pair of eyeglasses.
Does Medicare pay for cataract surgery and glasses afterwards?
for corrective lenses after each cataract surgery with an intraocular lens. You pay any additional costs for upgraded frames. Medicare will only pay for contact lenses or eyeglasses from a supplier enrolled in Medicare, no matter if you or your supplier submits the claim.
Can I have 2 different vision insurance plans?
VSP allows coordination of benefits for patients eligible for coverage by more than one vision plan. When coordinating benefits, it must be determined which plan is billed first. The plan that covers the member as an employee is “primary”. The plan that covers the member as a dependent is “secondary”.
Is VSP good at Costco?
Unfortunately, we already know that Costco doesn't accept all major insurance plans, since VSP is the largest vision care insurance provider in the country.
How does double vision coverage work?
When an employee has two different insurance plans at the same time, they have dual coverage. One plan will be designated as the primary plan and will pay first, the other will be designated as the secondary plan and will pay second.
Which insurance is primary when you have two?
If you have two plans, your primary insurance is your main insurance. Except for company retirees on Medicare, the health insurance you receive through your employer is typically considered your primary health insurance plan.
How do you determine which insurance is primary and which is secondary?
The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" to pay. The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer.
What happens when Medicare is secondary?
The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the remaining costs. If your group health plan or retiree coverage is the secondary payer, you may need to enroll in Medicare Part B before they'll pay.
Why do I need vision insurance if I have Medicare?
Why would I need a vision insurance plan if I have a Medicare plan? Because in many cases Medicare plans (like Original Medicare) do not provide comprehensive vision coverage. If you have a Medicare plan that doesn’t provide comprehensive vision coverage, you can supplement it with a VSP Individual Vision Plan.
Can I use a VSP with Medicare?
Can I coordinate a VSP Individual Vision Plan with my Medicare plan? VSP Vision Care does not coordinate benefits with Medicare. In other words, you can't use $150 of frame allowance from a VSP plan and add $50 of allowance from a Medicare plan to get a $200 frame fully covered. You would use one plan's benefit or the other.
Which pays first, Medicare or ESRD?
The group health plan pays first for qualified services, and Medicare is the secondary payer. You have ESRD and COBRA insurance and have been eligible for Medicare for 30 months or fewer. COBRA pays first in this situation.
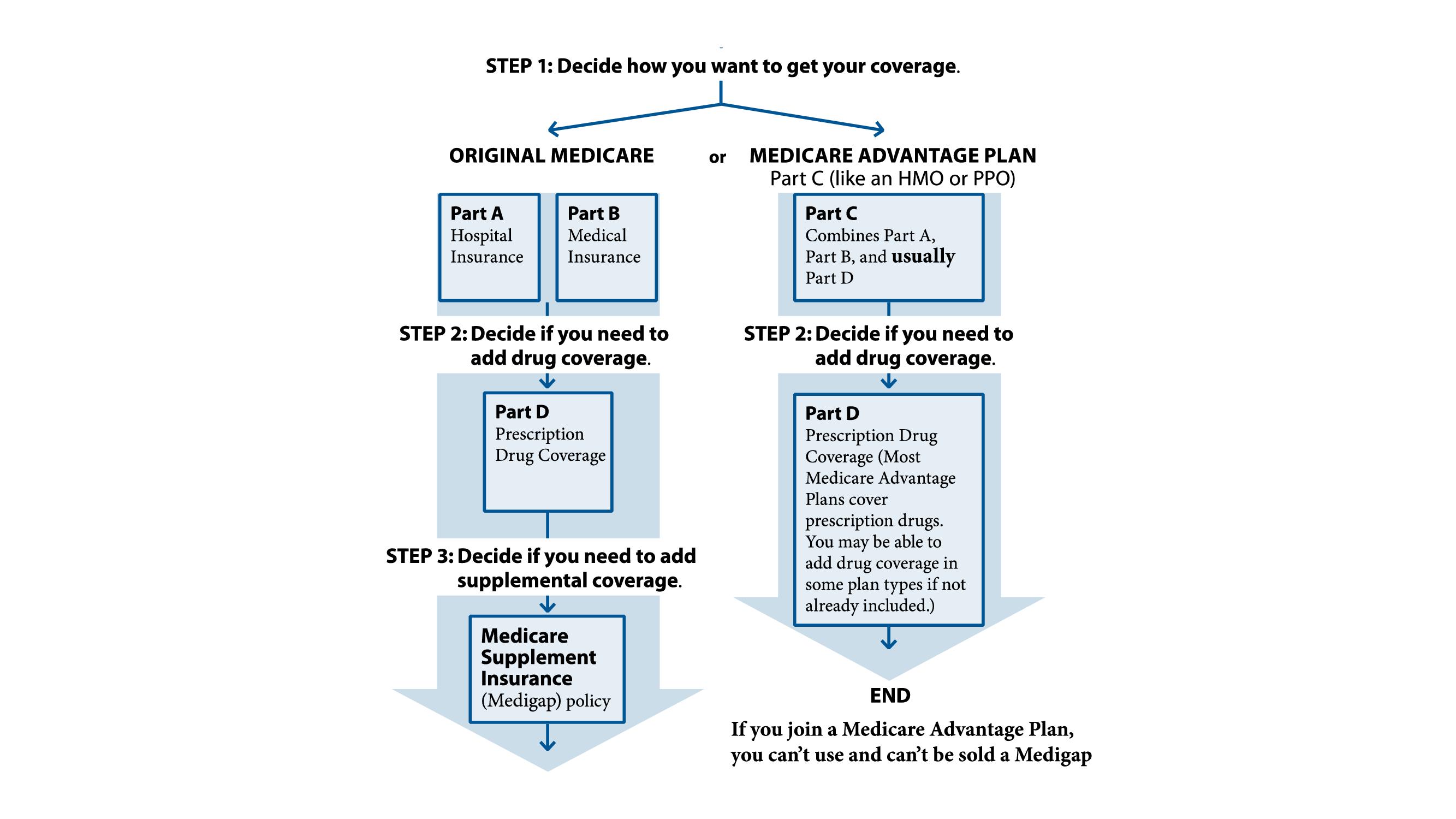
What is Medicare Advantage?
A Medicare Advantage plan replaces your Original Medicare coverage. In addition to those basic benefits, Medicare Advantage plans can also offer some additional coverage for things like prescription drugs, dental, vision, hearing aids, SilverSneakers programs and more.
How long do you have to be on Cobra to get Medicare?
You have ESRD and COBRA insurance and have been eligible for Medicare for at least 30 months. COBRA is the secondary payer in this situation, and Medicare pays first for qualified services. You are 65 or over – or you are under 65 and have a disability other than ESRD – and are covered by either COBRA insurance or a retiree group health plan.
What is a group health plan?
The group health plan is your secondary payer after Medicare pays first for your health care costs. You have End-Stage Renal Disease (ESRD), are covered by a group health plan and have been entitled to Medicare for at least 30 months. The group health plan pays second, after Medicare. You have ESRD and COBRA insurance and have been eligible ...
Is Medicare a secondary payer?
Medicare serves as the secondary payer in the following situations: You are 65 or older and are covered by a group health plan because you or your spouse is still working and the employer has 20 or more employees. The group health plan is the primary payer, and Medicare pays second.
Does tricare work with Medicare?
You may use both types of insurance for your health care , but they will operate separately from each other. TRICARE does work with Medicare. Active-duty military personnel who are enrolled in Medicare may use TRICARE as a primary payer, and then Medicare pays second as a secondary payer. For inactive members of the military who are enrolled in ...
Is Medicare Part A or Part B?
While you must remain enrolled in Medicare Part A and Part B (and pay the associated premiums), your Medicare Advantage plan serves as your Medicare coverage. Medicare Part D, which provides coverage for prescription drugs, is another type of private Medicare insurance.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
How to learn more about Medicare?
How to Learn More About Your Medicare Options. Primary insurance isn't too hard to understand; it's just knowing which insurance pays the claim first. Medical billing personnel can always help you figure it out if you're having trouble. While it's not hard to understand primary insurance, Medicare is its own beast.
Is Medicare primary insurance in 2021?
Updated on July 13, 2021. Many beneficiaries wonder if Medicare is primary insurance. But, the answer depends on several factors. While there are times when Medicare becomes secondary insurance, for the most part, it’s primary. Let’s go into further detail about what “primary” means, and when it applies.
Is Medicare a primary or secondary insurance?
Mostly, Medicare is primary. The primary insurer is the one that pays the claim first, whereas the secondary insurer pays second. With a Medigap policy, the supplement is secondary. Medicare pays claims first, and then Medigap pays. But, depending on the other policy, you have Medicare could be a secondary payer.
Does Medicare pay your claims?
Since the Advantage company pays the claims, that plan is primary. Please note that Medicare WON’T pay your claims when you have an Advantage plan. Medicare doesn’t become secondary to an Advantage plan. So, you’ll rely on the Advantage plan for claim approvals.
Can you use Medicare at a VA hospital?
Medicare and Veterans benefits don’t work together; both are primary. When you go to a VA hospital, Veteran benefits are primary. Then, if you go to a civilian doctor or hospital, Medicare is primary. But, you CAN’T use Veterans benefits at a civilian doctor. Also, you can’t use Medicare benefits at the VA.
Is Medicare a part of tricare?
Medicare is primary to TRICARE. If you have Part A, you need Part B to remain eligible for TRICARE. But, Part D isn’t a requirement. Also, TRICARE covers your prescriptions. Your TRICARE will be similar to a Medigap plan; it covers deductibles and coinsurances.
VSP and medicare (using both insurances on same day)
Initially I was under the impression that you could not bill VSP and another insurance on the same day. However, in the VSP provider manual there is a flowchart which indicates that if you see a patient who has both VSP and medicare, then you can bill medicare for the medical exam and VSP for the refraction on the same day.
double dipping?
hypothetically... if a patient has medicare AND a supplemental insurance that will pick up the refraction...and if the patient pays for the refraction up front...and then the supplement pays as well...and the OD doesn't reimburse one of them...that's FRAUD, right?
What is Medicare Part A?
Medicare Part A is intended to serve individuals strictly as a hospital insurance. If you are admitted to the hospital because of an accident involving your eyes, your plan benefits would apply; otherwise, you are responsible for all costs associated with routine vision corrections and eye exams. Oftentimes, individuals with Medicare Part A enroll ...
Do Part C plans include vision insurance?
Many Part C plans include routine vision benefits, but you should make sure this is the case ahead of time. Part C plans help individuals group everything into one plan, but you should expect to pay more per month for plans with vision coverage.
Does Medicare cover glaucoma screening?
Medicare Part B does cover annual glaucoma screenings for high-risk patients. These include individuals with diabetes or a family history of glaucoma, African-Americans over the age of 50, and Hispanics over the age of 65.
Does Medicare cover eye exams?
Medicare Part B does not cover routine eye examinations and vision correction. That means prescription glasses and contact lenses will not be covered by your plan, unless you have had a necessary cataract surgery. Medicare Part B does cover annual glaucoma screenings for high-risk patients. These include individuals with diabetes ...
Is BCBS a primary or secondary insurance?
Depends on what type of insurance that is. If it’s commercial insurance (usually via employer); then that is primary. If BCBS is a Medicare advantage plan, then it is first as it combines Medicare A, B, and Prescriptions all in one, Secondary would be like Medicaid. If it’s
Is Medicare first billed?
Medicare is always first billed. Is the BCBS a Medigap supplement insurance or is it an employer insurance plan? Medicare covers 100% for 20 days, then there is a co-payment to 100 days. Then you have to pay full price or leave.