Yes. If you aren’t covered by one of the exceptions listed below, you can be charged up to 10 percent more for Medicare Part B — the part of Medicare that provides standard medical insurance — for each full year past the eligibility age of 65 that you delay enrolling.
Will you be penalized for not getting Medicare at 65?
If you didn’t get Medicare at 65, you would not be later charged with late-enrollment penalties, so long as your employer signed this form indicating you’ve had insurance coverage. The form would...
Is it mandatory to go on Medicare at 65?
In this circumstance, it is mandatory to sign up for Medicare unless you are one of the few people who pay premiums for Part A. You’ll still want to sign up for Medicare at age 65 to avoid late penalties, delayed coverage, and loss of Social Security benefits.
What to do before you turn 65 Medicare?
at least 3 months BEFORE you turn 65. EVERYONE WHO IS TURNING 65 should complete these tasks: Get familiar with Medicare and its “parts” To learn about Medicare, see the “ Introduction to Medicare ” fact sheet. You can also visit Medicare.gov or call 1-800-MEDICARE (1-800-633-4227); TTY users should call 1-877-486-2048.
Does Medicare cover all medical expenses after age 65?
The short answer is “no”; however, it will cover a significant portion of a person’s medical expenses. Thus, the challenge for the patient is to understand what Medicare, Medigap, prescription plans, and other plans will cover. Medicare is a federal insurance program that guarantees health coverage for people 65 and older, those with extreme disabilities and infants who have significant medical problems at birth.

What happens if you don't enroll in Medicare Part A at 65?
The Part A penalty is 10% added to your monthly premium. You generally pay this extra amount for twice the number of years that you were eligible for Part A but not enrolled. For example, suppose that: You were eligible for Medicare in 2020, but you didn't sign up until 2022.
How do I avoid Medicare Part B penalty?
If you don't qualify to delay Part B, you'll need to enroll during your Initial Enrollment Period to avoid paying the penalty. You may refuse Part B without penalty if you have creditable coverage, but you have to do it before your coverage start date.
What happens if you enroll late for Medicare?
If you don't enroll when you're first eligible for Medicare, you can be subject to a late-enrollment penalty, which is added to the Medicare Part A premium. The penalty is 10% of your monthly premium, and it applies regardless of the length of the delay.
How long is a member responsible for a late enrollment penalty for Medicare?
63 daysMedicare beneficiaries may incur a late enrollment penalty (LEP) if there is a continuous period of 63 days or more at any time after the end of the individual's Part D initial enrollment period during which the individual was eligible to enroll, but was not enrolled in a Medicare Part D plan and was not covered under ...
Can Medicare penalties be waived?
You may qualify to have your penalty waived if you were advised by an employee or agent of the federal government – for example by Social Security or 1-800-MEDICARE – to delay Part B. Asking for the correction is known as requesting equitable relief.
How is the Medicare Part B penalty calculated?
Calculating Lifetime Penalty Fees Calculating your Part B penalty is fairly straightforward. You simply add 10% to the cost of your monthly premium for each year-long period you didn't have Medicare. It's simple to get a snapshot of what you will have to pay each month.
How do I avoid Part D Penalty?
3 ways to avoid the Part D late enrollment penaltyEnroll in Medicare drug coverage when you're first eligible. ... Enroll in Medicare drug coverage if you lose other creditable coverage. ... Keep records showing when you had other creditable drug coverage, and tell your plan when they ask about it.
What is Lifetime late enrollment penalty?
The late enrollment penalty is an amount that's permanently added to your Medicare drug coverage (Part D) premium. You may owe a late enrollment penalty if at any time after your Initial Enrollment Period is over, there's a period of 63 or more days in a row when you don't have Medicare drug coverage or other.
How does the late enrollment penalty work?
The late enrollment penalty amount typically is 1% of the “national base beneficiary premium” (also called the base beneficiary premium) for each full, uncovered month that the person didn't have Medicare drug coverage or other creditable coverage. The national base beneficiary premium for 2022 will be $33.37.
When did Medicare Part D become mandatory?
The MMA also expanded Medicare to include an optional prescription drug benefit, “Part D,” which went into effect in 2006.
Why are there Medicare penalties?
Medicare charges several late-enrollment penalties. They're meant to discourage you from passing up coverage, then getting hit with costly medical bills. To avoid higher Medicare premiums, you need to know about these penalties and take steps to avoid them.
Do I need Medicare Part D if I don't take any drugs?
No. Medicare Part D Drug Plans are not required coverage. Whether you take drugs or not, you do not need Medicare Part D.
What happens if I don't sign up for Medicare at 65?
What happens if I don’t sign up for Medicare when I’m 65? A. Joining Medicare is voluntary. But there may be consequences—in the form of a late penalty—if you don’t enroll at the “right” time, depending on your circumstances.
What happens if you delay a car insurance payment for 5 years?
For example, if you delay five years, you’ll pay an extra 50 percent of the cost of that year’s premium. The penalty amount grows larger over time because it’s pegged to the cost of each year’s Part B premiums, which generally rise every year.
What happens if you delay signing up for Part B?
You need to carefully consider your rights and options .) Part B (doctors and outpatient services): If you delay signing up for Part B beyond the time when you’re first eligible for it, you could incur a late penalty. (The exception is if you’re still working and have “primary” health insurance from your employer.)
Is there a penalty for not signing up for Part A?
Part A (hospital insurance) : There is no penalty for delaying to enroll in Part A if you qualify for it automatically on the basis of you or your spouse’s work record. But in most circumstances, there’s no reason not to sign up as soon as you’re eligible.
Do you have to pay a late penalty for prescription drugs?
There are exceptions. You would not risk a late penalty for as long as you have other insurance for prescription drugs (such as coverage under an employer health plan or retiree benefits) that is considered at least as good as Part D. If this is the case, you won’t need Part D unless you lose or drop such coverage.
When is the Medicare enrollment period?
General Enrollment Period (GEP) If you miss the deadline for your IEP or SEP (or if you don’t qualify for a SEP), you can enroll in Medicare only during a general enrollment period, which runs from Jan. 1 to March 31 each year, with coverage not beginning until July 1 of the same year. If you need Medicare prescription drug coverage, ...
How far in advance can you start Medicare?
While active employment continues, you can specify the date on which you want Medicare coverage to begin, up to three months in advance. Otherwise, your coverage begins on the first day of the month after you enroll.
When is the open enrollment period for Medicare Part A?
Note: You cannot enroll in Medicare Part A or B for the first time during Medicare’s annual open enrollment period, which runs from Oct. 15 to Dec. 7 each year. This period is only for people already in Medicare who want to change their type of coverage for the following year.
What happens if you don't get Part B?
If you didn't get Part B when you're first eligible, your monthly premium may go up 10% for each 12-month period you could've had Part B, but didn't sign up. In most cases, you'll have to pay this penalty each time you pay your premiums, for as long as you have Part B.
How much is the penalty for Part B?
Your Part B premium penalty is 20% of the standard premium, and you’ll have to pay this penalty for as long as you have Part B. (Even though you weren't covered a total of 27 months, this included only 2 full 12-month periods.) Find out what Part B covers.
Medicare Part A
According to the Medicare website, some people have to buy Part A because they don’t qualify for premium-free Part A. If you have to buy Part A — and you don’t buy it when you’re first eligible for Medicare — your monthly premium might go up by 10%. You’ll have to pay the higher premium for twice the number of years you didn’t sign up.
Medicare Part B
If you didn’t get Part B when you were first eligible, your monthly premium might go up 10% for each 12-month period you could’ve had Part B but didn’t sign up for it. In most cases, you’ll have to pay the penalty each time you pay your premiums for as long as you have Part B. The penalty increases the longer you go without Part B coverage.
Medicare Part D
With Medicare Part D, the late enrollment penalty is an amount that’s permanently added to your Medicare drug coverage premium.
What happens if you don't get Medicare at 65?
If you didn’t get Medicare at 65, you would not be later charged with late-enrollment penalties, so long as your employer signed this form indicating you’ve had insurance coverage. The form would be presented when you later needed Medicare. There is an eight-month special enrollment period that begins on the date a person aged 65 ...
How long does Medicare cover after you stop working?
It sounds like you will have retiree coverage and Medicare for five years after you stop working. It would be a good idea for you to find out exactly what your retiree plan covers and how it and Medicare would coordinate payment of any covered insurance claims.
How old do you have to be to qualify for unemployment if you die?
If he died at age 60 or younger, she would qualify for benefits because the agency would adjust the hours needed. Thirty-eight quarters of so-called covered earnings would be enough to qualify for someone who died two years before reaching the earliest age at which benefits normally are available.
Can I collect Social Security at 66?
When you apply for your benefit at age 66, she will be eligible for a spousal benefit. If it’s larger than her survivor benefit, she’d receive an additional payment equal to the difference. If not, her benefit would stay the same. Frank: I’m planning to collect Social Security at age 66 this fall.
Can my wife file for spousal benefits at 62?
Under new rules passed in late 2015, there is no way she can file for a spousal benefit while deferring her own retirement filing.
Should people with Cobra be penalized?
The main concern for people with COBRA should not be penalties but making sure they do not have an unintentional lapse in primary health coverage. Phil Moeller: You should not have to worry about penalties.
What happens if you don't sign up for Medicare?
Specifically, if you fail to sign up for Medicare on time, you’ll risk a 10 percent surcharge on your Medicare Part B premiums for each year-long period you go without coverage upon being eligible.
When do you get Medicare if you leave your job?
In that case, you’ll get an eight-month special enrollment period to sign up for Medicare if and when you leave your job or your employer stops offering coverage. It will start the month after you separate from your employer, or the month after your group health coverage ends – whichever happens sooner.
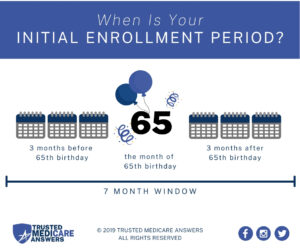
How long does it take to get Medicare?
Learn how to make sure they have health insurance once you’re enrolled. Medicare eligibility starts at age 65. Your initial window to enroll is the seven-month period that begins three months before the month of your 65th birthday and ends three months after it. Seniors are generally advised to sign up on time to avoid penalties ...
Do you have to double up on Medicare?
No need to double up on coverage. Many seniors are no longer employed at age 65, and thus rush to sign up for Medicare as soon as they’re able. But if you’re still working at 65, and you have coverage under a group health plan through an employer with 20 employees or more, then you don’t have to enroll in Medicare right now.
Does Medicare pay for Part A?
That said, it often pays to enroll in Medicare Part A on time even if you have health coverage already. It won’t cost you anything, and this way, Medicare can serve as your secondary insurance and potentially pick up the tab for anything your primary insurance (in this case, your work health plan) doesn’t cover.
What is the late enrollment penalty for Medicare?
Part D late enrollment penalty. The late enrollment penalty is an amount that's permanently added to your Medicare drug coverage (Part D) premium. You may owe a late enrollment penalty if at any time after your Initial Enrollment Period is over, there's a period of 63 or more days in a row when you don't have Medicare drug coverage or other.
What happens if Medicare decides the penalty is wrong?
What happens if Medicare's contractor decides the penalty is wrong? If Medicare’s contractor decides that all or part of your late enrollment penalty is wrong, the Medicare contractor will send you and your drug plan a letter explaining its decision. Your Medicare drug plan will remove or reduce your late enrollment penalty. ...
What happens if Medicare pays late enrollment?
If Medicare’s contractor decides that your late enrollment penalty is correct, the Medicare contractor will send you a letter explaining the decision, and you must pay the penalty.
How long do you have to pay late enrollment penalty?
You must do this within 60 days from the date on the letter telling you that you owe a late enrollment penalty. Also send any proof that supports your case, like a copy of your notice of creditable prescription drug coverage from an employer or union plan.
How long does it take for Medicare to reconsider?
In general, Medicare’s contractor makes reconsideration decisions within 90 days. The contractor will try to make a decision as quickly as possible. However, you may request an extension. Or, for good cause, Medicare’s contractor may take an additional 14 days to resolve your case.
Do you have to pay a penalty on Medicare?
After you join a Medicare drug plan, the plan will tell you if you owe a penalty and what your premium will be. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
Does Medicare pay late enrollment penalties?
, you don't pay the late enrollment penalty.
Does Cobra end with Medicare?
If you have COBRA coverage, you need to know that your COBRA coverage normally will end if you enroll in Medicare. This puts you in an either-or situation, and you need to compare the benefits of keeping your COBRA coverage while it remains available to the benefits of switching to Medicare.
Can I delay enrolling in Medicare if I have Cobra?
That’s a strong sign that you shouldn’t delay enrolling in Medicare if you’re expecting COBRA coverage in the future. And, remember, it’s Medicare and not COBRA that you can expect to stay in your corner for life. 2. I have a Health Savings Account (HSA).