If you continue to work, your employer's insurance pays first. And, if you've already left the company and have a retiree plan or COBRA, those plans typically become the primary payer until you turn age 65. Otherwise, you will be the primary payer until your Medicare coverage begins.
What happens when you turn 65 and don’t have Medicare?
The question is, if a person has health insurance either through their employer or through their spouse when they turn 65 and opt not to get healthcare coverage through Medicare immediately, as required by Medicare, will they be penalized when they do get healthcare coverage through Medicare? The short answer is no.
Does retiree insurance work with Medicare?
Your retiree insurance can work with Medicare. It’s best to enroll in Part A and Part B during your Initial Enrollment Period to avoid penalties. In general, Medicare will be your primary insurance, and your retiree insurance will be secondary. What are the costs and coverage of retiree insurance?
Is Medicare Supplement Insurance the same as retiree insurance?
Since Medicare pays first after you retire, your retiree coverage is likely to be similar to coverage under Medicare Supplement Insurance (Medigap). Retiree coverage isn't the same thing as a Medigap policy but, like a Medigap policy, it usually offers benefits that fill in some of Medicare's gaps in coverage—like.
How does retiree coverage work with Medicare Part A and B?
Retiree coverage might not pay your medical costs during any period in which you were eligible for Medicare but didn't sign up for it. When you become eligible for Medicare, you will need to enroll in both Medicare Part A and Part B to get full benefits from your retiree coverage. How does your retiree coverage work with Medicare?

Is Medicare primary over a retiree plan?
Regardless of your retiree insurance, you must make sure to enroll in Medicare Parts A and B because Medicare will always pay first after you retire (called primary insurance) and your retiree plan will pay second (called secondary insurance).
Is Medicare automatically primary?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
Is Medicare Part A primary or secondary?
primaryEven if you have a group health plan, Medicare is the primary insurer as long as you've been eligible for Medicare for 30 months or more.
How do you determine which health insurance is primary?
If you have Medicare and other health insurance or coverage, each type of coverage is called a "payer." When there is more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" to pay.
Does Medicare coverage start the month you turn 65?
The date your coverage starts depends on which month you sign up during your Initial Enrollment Period. Coverage always starts on the first of the month. If you qualify for Premium-free Part A: Your Part A coverage starts the month you turn 65.
What happens when Medicare is secondary?
The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the remaining costs. If your group health plan or retiree coverage is the secondary payer, you may need to enroll in Medicare Part B before they'll pay.
Do retirees pay Medicare premiums?
Although Part A, which pays for hospital care, is free for most beneficiaries, you'll pay a monthly premium for Part B, which covers doctor visits and outpatient services. In 2022, the standard monthly premium will be $170.10, up from $148.50 in 2021.
Is Medicare Part D always primary?
Usually Medicare Part D coverage pays first. For example: Are you retired and have prescription drug coverage through your or your spouse's former employer's or union's retiree Group Health Plan and Medicare Part D coverage? If so, your Medicare Part D coverage is primary and the Group Health Plan is secondary.
Is it necessary to have supplemental insurance with Medicare?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
When two insurance which one is primary?
If you have two plans, your primary insurance is your main insurance. Except for company retirees on Medicare, the health insurance you receive through your employer is typically considered your primary health insurance plan.
Can you have Medicare and another insurance at the same time?
It is possible to have both private insurance and Medicare at the same time. When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer.
How does it work when you have two insurances?
Secondary insurance: once your primary insurance has paid its share, the remaining bill goes to your “secondary” insurance, if you have more than one health plan. Your secondary insurance may cover part or all of the remaining cost.
What is a Medicare leave period?
A period of time when you can join or leave a Medicare-approved plan.
How long can you join a health insurance plan?
You can join a plan anytime while you have job-based health insurance, and up to 2 months after you lose that insurance.
What happens if you miss the 8 month special enrollment period?
If you miss this 8-month Special Enrollment Period, you’ll have to wait to sign up and go months without coverage. You might also pay a monthly penalty for as long as you have Part B. The penalty goes up the longer you wait to sign up.
Do you have to tell Medicare if you have non-Medicare coverage?
Each year your plan must tell you if your non-Medicare drug coverage is creditable coverage. Keep this information — you may need it when you’re ready to join a Medicare drug plan. (Don’t send this information to Medicare.)
Does Cobra end with Medicare?
Your COBRA coverage will probably end when you sign up for Medicare. (If you get Medicare because you have End-Stage Renal Disease and your COBRA coverage continues, it will pay first.)
Do I need to get Medicare drug coverage (Part D)?
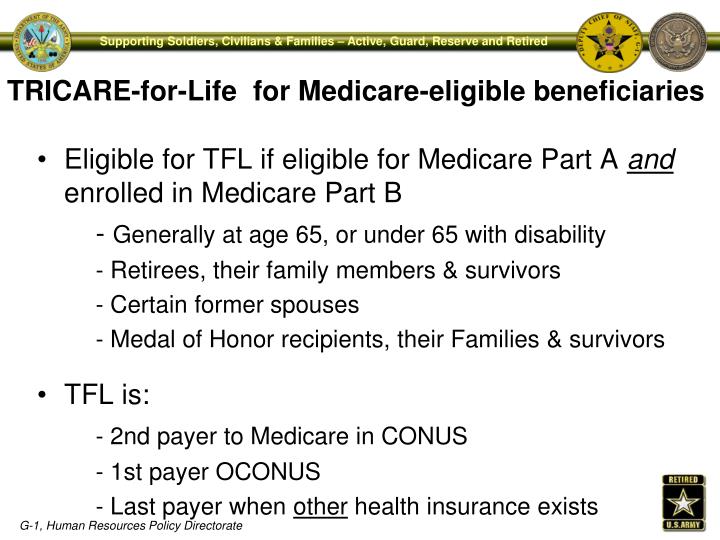
Prescription drug coverage that provides the same value to Medicare Part D. It could include drug coverage from a current or former employer or union, TRICARE, Indian Health Service, VA, or individual health insurance coverage.
When do you need to sign up for Medicare?
If the employer has less than 20 employees: You might need to sign up for Medicare when you turn 65 so you don’t have gaps in your job-based health insurance. Check with the employer.
What is a Medicare leave period?
A period of time when you can join or leave a Medicare-approved plan.
Do I need to get Medicare drug coverage (Part D)?
You can get Medicare drug coverage once you sign up for either Part A or Part B. You can join a Medicare drug plan or Medicare Advantage Plan with drug coverage anytime while you have job-based health insurance, and up to 2 months after you lose that insurance.
What happens if you don't sign up for Part A and Part B?
If you don’t sign up for Part A and Part B, your job-based insurance might not cover the costs for services you get.
Do you have to tell Medicare if you have non-Medicare coverage?
Each year, your plan must tell you if your non-Medicare drug coverage is creditable coverage. Keep this information — you may need it when you’re ready to join a Medicare drug plan.
Does Medicare work if you are still working?
If you (or your spouse) are still working, Medicare works a little differently. Here are some things to know if you’re still working when you turn 65.
Does private insurance pay for services?
Some private insurance has rules that lower what they pay (or don’t pay at all) for services you get if you’re eligible for other coverage, like Medicare.
What is Medicare for people 65 and older?
Medicare. Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD) and. group health plan.
Does retirement insurance include extra benefits?
and deductibles. Sometimes retiree coverage includes extra benefits, like coverage for extra days in the hospital.
When do you have to retire to get Medicare?
Most people become eligible for Medicare at age 65, which is also the age at which many people retire. However, many American seniors are postponing retirement to continue working, and some are retiring early.
What happens when you have Medicare and another type of insurance?
When you have Medicare and another type of insurance, one will be the primary payer and one will be the secondary payer.
How long does it take to file a Medicare claim?
1 10-minute claim is based solely on the time to complete the e-application if you have your Medicare card and other pertinent information available when you apply. The time to shop for plans, compare rates, and estimate drug costs is not factored into the claim. Application time could be longer. Actual time to enroll will depend on the consumer and their plan comparison needs.
When to manually enroll in Medicare?
The best time to manually enroll in Medicare is during your Medicare Initial Enrollment Period.
What happens if you don't sign up for Medicare?
Failure to sign up for Medicare during your Initial Enrollment Period could cause you to pay late enrollment penalties, resulting in permanently higher monthly premiums (unless you qualify for a Special Enrollment Period).
When do you have to enroll in Medicare Part B?
If you work for a company with fewer than 20 people, your employer may require you to enroll in Medicare Part B at the age of 65. We recommend speaking with your employer directly to learn more about your health insurance options when working past age 65.
How much is Medicare Part B in 2021?
Unlike premium-free Part A, Medicare Part B requires you to pay a monthly premium for your Part B benefits ($148.50 per month in 2021, though it could potentially be higher based on your income).
How Does Medicare Work with Retiree Insurance?
In general, if you have Medicare and retiree insurance, Medicare will pay your health care bills first. In this case, your group coverage is your secondary insurance. Thus, it acts similar to a Medicare Supplement policy. To get full benefits from your retiree insurance, you’ll want to enroll in Part A and Part B when you become eligible.
What type of insurance do you get when you retire?
Sometimes after you retire, your employer will offer group insurance. This type of insurance is called retiree insurance, but how does it work with Medicare? While you might have retired early, you should be informed about the answer to this and other questions before you’re eligible.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
When is Medicare paid first?
When you’re eligible for or entitled to Medicare because you have End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, the group health plan or retiree coverage pays first and Medicare pays second. You can have group health plan coverage or retiree coverage based on your employment or through a family member.
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
Which pays first, Medicare or group health insurance?
If you have group health plan coverage through an employer who has 20 or more employees, the group health plan pays first, and Medicare pays second.
What happens when you retire from Medicare?
Understanding Your Medicare Benefits. When retirement finally comes, it may bring changes into your life. While you may enjoy some time to travel or spend time with family, you may find changes when it comes to your health insurance as well.
How old do you have to be to get Medicare?
People can qualify for Medicare at the age of 65 . This insurance is available for individuals under the age of 65, but only for those who have a permanent disability or who suffer from amyotrophic lateral sclerosis (ALS) or end-stage renal disease. If you do have a permanent disability, you will also need to have received social security benefits for more than two years to become eligible.
What is Medicare Part A?
Medicare Part A is responsible for covering inpatient expenses, including overnight stays in in a hospital if you are formally admitted after surgery, during long-term hospital admissions, hospice care, skilled nursing facilities, and other similar services. Part A is standard for all Medicare recipients, and the premium payment is determined by the amount of time you have paid Medicare taxes. If you have worked and paid Medicare taxes for at least 10 years, you will not have a Part A premium payment. However, if you have worked less than 10 years, you will be required to pay a monthly premium.
What is original Medicare?
Original Medicare is the federal program available to all individuals eligible for Medicare. It includes Part A and Part B. Medicare Part A and Part B can both be selected upon enrollment, or Part B can be declined if a person so chooses.
When do you have to sign up for Medicare?
It is important to sign up for Medicare as soon as the eligibility period opens, which occurs three months prior to your 65th birthday. It will apply during the month of your 65 th birthday, and three months after your birthday.
What is Part B insurance?
Part B covers outpatient expenses and preventive care, such as annual checkups, diagnostic testing, ambulance services, and studies. Part B requires a monthly premium payment and can be declined upon eligibility.
When do you sign up for Medicare Part A?
Despite the fact that a person has adequate healthcare coverage through their employer or their spouse’s employer when they turn 65 years old , people often sign up for Medicare Part A anyhow.
How does a Medicare policy work?
For those people who do opt to get a Medicare plan and keep their insurance policy through their employer or their spouse’s employer, the two policies will work together to determine which policy will pay a claim first. This situation is a called a “coordination of benefits” and requires the primary payer (oftentimes the private insurance policy) to pay a claim first to their policy limits before passing the remaining amount due to the secondary payer (the Medicare plan) to pay the remaining amount. Of course, whether or not the private insurance policy is considered the primary or secondary payer depends on the circumstances. When you sign up for a Medicare policy, the application will ask several specific questions regarding your employer and the insurance policy through your employer to determine the ranking.
How long does the special enrollment period last?
The Special Enrollment Period will last for eight months starting on the month after the event occurs. Therefore, if a person’s employment ends in March, they will have eight months starting in April to sign up for Medicare without being penalized. Under these circumstances, a person is not confined by the general enrollment period in order to sign up for a Medicare plan.
How long do you have to sign up for Medicare?
The mandatory enrollment period also includes your birthday month and the three months after your birthday month. In total, you have a seven-month window to sign up for a Medicare policy. This period of time to enroll applies to any Medicare program.
What happens if you don't sign up for Medicare?
If a person does not sign up for insurance through Medicare, either through the Social Security Office for a Medicare Part A and/or Part B plan or through a private insurance company for a Medicare Advantage, which is also known as a Medicare Part C plan, there may be a penalty imposed for waiting. The question is, if a person has health insurance ...
When is Medicare Part D enrollment?
The enrollment period for Medicare Part D and Medicare Part C, which is also known as Medicare Advantage, runs from October 15 th to December 7 th of each year. Of course, if you miss the mandatory enrollment period and do not get to sign up for a Medicare policy during the general enrollment period, you will likely be penalized for late enrollment.
Is Medicare a primary or secondary payer?
Of course, whether or not the private insurance policy is considered the primary or secondary payer depends on the circumstances. When you sign up for a Medicare policy, the application will ask several specific questions regarding your employer and the insurance policy through your employer to determine the ranking.
