Medicare is federal health insurance for anyone age 65 and older, and some people under 65 with certain disabilities or conditions. Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
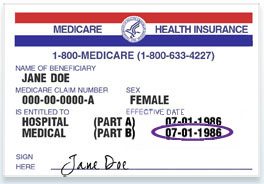
Does your patient have Medicare?
You're still in the Medicare Program. You still have Medicare rights and protections. You still get complete Part A and Part B coverage through the plan. Some plans offer extra benefits that Original Medicare doesn’t cover – like vision, hearing, or dental. Your out-of-pocket costs may be lower in a Medicare Advantage Plan. If so, this option may be more cost effective for you.
What is the cheapest Medicare plan?
- New York City: Plan G is $268 to $545 High-deductible Plan G: $69 to $91
- Tampa, Florida: Plan G is $176 to $263 High-deductible Plan G: $52 to $92
- Houston, Texas: Plan G is $128 to $434 High-deductible Plan G: $36 to $86
- Albuquerque, New Mexico: Plan G is $105 to $355 High-deductible Plan G: $30 to $59
Where can I find a doctor that accepts Medicare and Medicaid?
How to find a doctor who accepts Medicare There are a few simple ways to find a doctor who accepts your Medicare plan: Visit physician compare. The Centers for Medicare & Medicaid Services (CMS) has a tool that allows you to look up doctors near you and compare them side-by-side.
Can a patient have Medicare Part B only?
Yes, it's possible to enroll in Medicare Part B without also enrolling in Medicare Part A. You can do this if you're 65 or older, a U.S. resident (additional rules apply for non-U.S. citizens), and do not yet qualify for premium-free Part A (having met the requirement of 40 quarters (10 years) of working life and paying FICA taxes).If you qualify for premium-free Part A, you'll apply for both Part A & B together or apply for Part A first and Part B down the line.
What type of people get Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
What is Medicare in patient?
Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
What are the 3 types of Medicare?
Different types of Medicare health plansMedicare Advantage Plans. ... Medicare Medical Savings Account (MSA) Plans. ... Medicare health plans (other than MA & MSA) ... Rules for Medicare health plans.
Which type is not covered by Medicare?
does not cover: Routine dental exams, most dental care or dentures. Routine eye exams, eyeglasses or contacts. Hearing aids or related exams or services.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Who is Medicare through?
The Centers for Medicare & Medicaid Services (CMS) is the federal agency that runs Medicare. The program is funded in part by Social Security and Medicare taxes you pay on your income, in part through premiums that people with Medicare pay, and in part by the federal budget.
What is the difference between Medicare and Medicaid?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
What are the two types of Medicare?
There are 2 main ways to get Medicare: Original Medicare includes Medicare Part A (Hospital Insurance) and Part B (Medical Insurance). If you want drug coverage, you can join a separate Medicare drug plan (Part D).
Who paid for Medicare?
Medicare is funded by the Social Security Administration. Which means it's funded by taxpayers: We all pay 1.45% of our earnings into FICA - Federal Insurance Contributions Act - which go toward Medicare.
Does Medicare cover 100% of costs?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
Does Medicare cover hospital stays?
Medicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual's reserve days. Medicare provides 60 lifetime reserve days.
Do all hospitals accept Medicare?
Not all hospitals accept Medicare, but luckily, the vast majority of hospitals do. Generally, the hospitals that do not accept Medicare are Veterans Affairs and active military hospitals (they operate with VA and military benefits instead), though there are a few other exceptions nationwide.
What is Medicare Advantage?
Medicare Advantage is a Medicare-approved plan from a private company that offers an alternative to Original Medicare for your health and drug coverage. These “bundled” plans include Part A, Part B, and usually Part D.
What are the extra benefits that Medicare doesn't cover?
Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
What is Medicare Supplemental Insurance?
Medicare Supplemental Insurance (Medigap): Extra insurance you can buy from a private company that helps pay your share of costs in Original Medicare. Policies are standardized, and in most states named by letters, like Plan G or Plan K. The benefits in each lettered plan are the same, no matter which insurance company sells it.
Is Medicare a federal or state program?
Medicaid is a joint federal and state program that provides health coverage for some people with limited income and resources. Medicaid offers benefits, like nursing home care, personal care services, and assistance paying for Medicare premiums and other costs.
Is my test, item, or service covered?
Find out if your test, item or service is covered. Medicare coverage for many tests, items, and services depends on where you live. This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
Your Medicare coverage choices
Learn about the 2 main ways to get your Medicare coverage — Original Medicare or a Medicare Advantage Plan (Part C).
What Part A covers
Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
What Part B covers
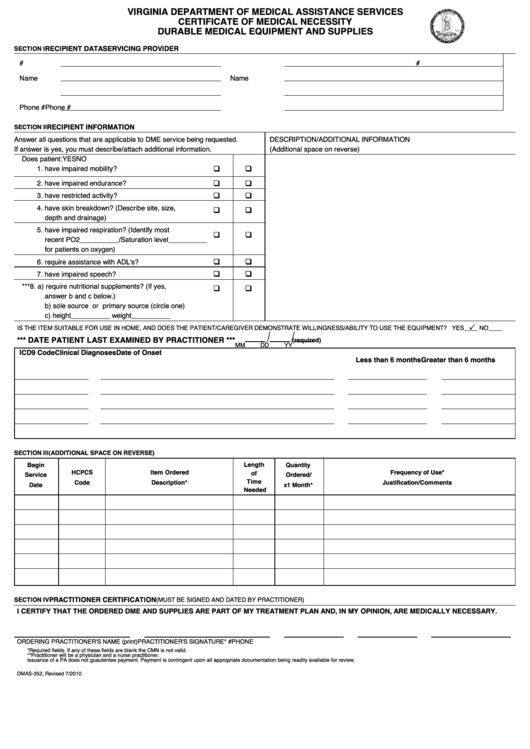
Learn about what Medicare Part B (Medical Insurance) covers, including doctor and other health care providers' services and outpatient care. Part B also covers durable medical equipment, home health care, and some preventive services.
What Medicare health plans cover
Medicare health plans include Medicare Advantage, Medical Savings Account (MSA), Medicare Cost plans, PACE, MTM
What's not covered by Part A & Part B
Learn about what items and services aren't covered by Medicare Part A or Part B. You'll have to pay for the items and services yourself unless you have other insurance. If you have a Medicare health plan, your plan may cover them.
What is hospital care?
Hospitals provide services like medical, surgical, and psychiatric care to people who are sick or injured. Services are ordered by a doctor. These types of hospitals can be found here using the "Hospital type" filter:
What is home health care?
Home health care provides skilled, short-term services in-home. These services are typically ordered by a doctor to help with recovery following an inpatient hospital stay, rehabilitation, or a stay at a facility providing skilled nursing care. In general, the goal of home health care is to help you get better, regain your independence, and be as self-sufficient as you can.
What is acute care?
Acute care: Give inpatient medical care and other related services for surgery, acute medical conditions or injuries (usually for a short-term illness or condition).
What is long term care?
Long-term care hospitals are acute care hospitals that provide extended medical and rehabilitative care to individuals who are clinically complex and have multiple acute or chronic conditions. Patients may improve with time and care and get discharged to home. Most patients are transferred to long-term care hospitals after they've been treated in an intensive or critical care unit. Long-term care hospital services include:
What is a doctor and a clinician?
Doctors and clinicians include doctors, clinicians and groups who are qualified to practice in many specialties. Each specialty focuses on certain parts of the body, periods of life, conditions, or primary care. The doctors, clinicians, and groups listed here typically work in an office or clinic setting. Only those who currently accept Medicare are included.
What is a nursing home?
Nursing homes are facilities for people who need 24-hour care. Most nursing homes provide both short-term and long-term care, including:
What is an inpatient rehabilitation facility?
Inpatient rehabilitation facilities are hospitals, or parts of hospitals, that offer an intensive rehabilitation to inpatients. Many patients with various conditions, like strokes or brain injuries, are transferred or admitted to an inpatient rehabilitation facility. Some inpatient rehabilitation facilities specialize in treating patients with certain medical conditions. Here, you'll get information on how many times a facility has treated Medicare patients with a specific condition in the last year, so you can find one that best fits your needs. The end goal of an inpatient rehabilitation facility is discharge to a patient's home or to another longer term facility as needed.
How to know if Medicare will cover you?
Talk to your doctor or other health care provider about why you need certain services or supplies. Ask if Medicare will cover them. You may need something that's usually covered but your provider thinks that Medicare won't cover it in your situation. If so, you'll have to read and sign a notice. The notice says that you may have to pay for the item, service, or supply.
What are the factors that determine Medicare coverage?
Medicare coverage is based on 3 main factors 1 Federal and state laws. 2 National coverage decisions made by Medicare about whether something is covered. 3 Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
What is Part B?
Part B covers 2 types of services. Medically necessary services: Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice. Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best.
What is Medicare Part A?
Part A coverage. Medicare Part A covers the care you receive when you’re admitted to a facility like a hospital or hospice center. Part A will pick up all the costs while you’re there, including costs normally covered by parts B or D. Part A coverage includes: hospital stays and procedures. hospice care.
What are the parts of Medicare?
Each part covers different healthcare services you might need. Currently, the four parts of Medicare are: Medicare Part A. Medicare Part A is hospital insurance. It covers you during short-term inpatient stays in hospitals and for services like hospice.
How long do you have to sign up for Medicare if you have delayed enrollment?
Special enrollment period. If you delayed Medicare enrollment for an approved reason, you can later enroll during a special enrollment period. You have 8 months from the end of your coverage or the end of your employment to sign up without penalty.
What is the maximum amount you can pay for Medicare in 2021?
In 2021, the out-of-pocket maximum for plans is $7,550. Note.
How many people are on medicare in 2018?
Medicare is a widely used program. In 2018, nearly 60,000 Americans were enrolled in Medicare. This number is projected to continue growing each year. Despite its popularity, Medicare can be a source of confusion for many people. Each part of Medicare covers different services and has different costs.
What age does Medicare cover?
Medicare is a health insurance program for people ages 65 and older , as well as those with certain health conditions and disabilities.
How old do you have to be to get Medicare?
You can enroll in Medicare when you meet one of these conditions: you’re turning 65 years old. you’ve been receiving Social Security Disability Insurance (SSDI) for 24 months at any age. you have a diagnosis of end-stage renal disease (ESRD) or amyotrophic lateral sclerosis (ALS) at any age.
What is covered by Medicare outpatient?
Covered outpatient hospital services may include: Emergency or observation services, which may include an overnight stay in the hospital or outpatient clinic services, including same-day surgery. Certain drugs and biologicals that you ...
How much does Medicare pay for outpatient care?
You usually pay 20% of the Medicare-approved amount for the doctor or other health care provider's services. You may pay more for outpatient services you get in a hospital than you’ll pay for the same care in a doctor’s office. However, the hospital outpatient Copayment for the service is capped at the inpatient deductible amount.
What is preventive care?
preventive services. Health care to prevent illness or detect illness at an early stage, when treatment is likely to work best (for example, preventive services include Pap tests, flu shots, and screening mammograms). . If you get hospital outpatient services in a critical access hospital, your copayment may be higher and may exceed ...
What is a copayment in a hospital?
An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug. A copayment is usually a set amount, rather than a percentage.
What is a deductible for Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. for each service. The Part B deductible applies, except for certain. preventive services.
Can you get a copayment for outpatient services in a critical access hospital?
If you get hospital outpatient services in a critical access hospital, your copayment may be higher and may exceed the Part A hospital stay deductible. If you get hospital outpatient services in a critical access hospital, your copayment may be higher and may exceed the Part A hospital stay deductible.
Does Part B cover prescription drugs?
Certain drugs and biologicals that you wouldn’t usually give yourself. Generally, Part B doesn't cover prescription and over-the-counter drugs you get in an outpatient setting, sometimes called “self-administered drugs.".
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
Which pays first, Medicare or group health insurance?
If you have group health plan coverage through an employer who has 20 or more employees, the group health plan pays first, and Medicare pays second.
What is Medicare Advantage?
Medicare Advantage is the private health insurance alternative to the federally run original Medicare. Think of Advantage as a kind of one-stop shopping choice that combines various parts of Medicare into one plan.
What part of Medicare pays for prescription drugs?
This is the part of Medicare that pays for some of your prescription drugs. You buy a Part D plan through a private insurer.
How much is Medicare deductible for 2021?
Medicare charges a hefty deductible each time you are admitted to the hospital. It changes every year, but for 2021 the deductible is $1,484. You can buy a supplemental or Medigap policy to cover that deductible and some out-of-pocket costs for the other parts of Medicare.
When will Medicare open enrollment start?
The next open enrollment will be from Oct. 15 to Dec. 7, 2021, and any changes you make will take effect in January 2022.
Does Medicare Advantage cover prescription drugs?
Most Medicare Advantage plans also fold in prescription drug coverage. Not all of these plans cover the same extra benefits, so make sure to read the plan descriptions carefully. Medicare Advantage plans generally are either health maintenance organizations (HMOs) or preferred provider organizations (PPOs).
Is Medicare complicated?
En español | Medicare is complicated and can be confusing to sort through. To make it easier, the program has been broken down into four basic parts that include coverage for everything from hospital care to doctor visits to prescription drugs.
Does Medicare cover vision?
The federal government requires these plans to cover everything that original Medicare covers, and some plans pay for services that original Medicare does not , including dental and vision care. In addition, in recent years the Centers for Medicare and Medicaid Services, which sets the rules for Medicare, has allowed Medicare Advantage plans to cover such extras as wheelchair ramps and shower grips for your home, meal delivery and transportation to and from doctors’ offices.