Medicare Part A is also known as hospital insurance. This part of Original Medicare typically helps cover inpatient services, such as hospital stays and care at a Skilled Nursing Facility (SNF Welcome sports fans, to a new era in televised football. Contracts are up, NBC is trying to replace the legendary MNF with a sharp-looking new SNF and things will not be the way they were before. NBC will be fielding a bus of an analyst (Jerome Bettis), the insightful ex-wide receiver Cris Collin…NBC Sunday Night Football
Full Answer
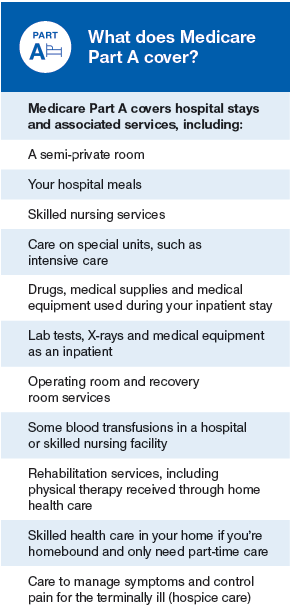
What does Medicare Part a cover for inpatient care?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. You’re admitted to the hospital as an inpatient after an official doctor’s order, which says you need inpatient hospital care to treat your illness or injury.
What does Medicare Part a cover for the elderly?
Part A covers inpatient care, skilled nursing services, some home health and rehabilitation costs, and hospice care. However, it does not cover doctor fees during a hospital stay, as Part B covers those costs.
What's not covered by part a&part B Medicare Part A?
What's not covered by Part A & Part B Medicare Part A coverage–hospital care Inpatient hospital care Skilled nursing facility care Long-term care hospitals Related Resources Find hospitals
How much does Medicare Part a cover long-term care?
Medicare Part A (Hospital Insurance) covers the cost of long-term care in a Long-term care hospital (LTCH). Days 1-60: $1,364 deductible.* D ays 61-90: $341 coinsurance each day. Days 91 and beyond: $682 coinsurance per each “lifetime reserve day” after day 90 for each benefit period (up to 60 days over your lifetime).

Which care and services are covered by Medicare Part A?
Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
Does Medicare Part A cover hospital stay?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
Which part of Medicare covers both inpatient and outpatient?
Part BPart A provides inpatient/hospital coverage. Part B provides outpatient/medical coverage. Part C offers an alternate way to receive your Medicare benefits (see below for more information). Part D provides prescription drug coverage.
What is the benefit period for Medicare Part A?
What Is A Benefit Period? In Medicare Part A, which is hospital insurance, a benefit period begins the day you go into a hospital or skilled nursing facility and ends when you have been out for 60 days in a row.
What does Medicare Part A cover quizlet?
Medicare Part A. Medicare Part A includes inpatient hospital coverage, skilled nursing care, nursing home care, and hospice care. It is the plan in which you're automatically enrolled when you apply for Medicare. The Part A plan is your hospital insurance plan.
What is not covered under Medicare Part A?
Medicare Part A will not cover long-term care, non-skilled, daily living, or custodial activities. Certain hospitals and critical access hospitals have agreements with the Department of Health & Human Services that lets the hospital “swing” its beds into (and out of) SNF care as needed.
What is Medicare Part A and Part B?
Part A (Hospital Insurance): Helps cover inpatient care in hospitals, skilled nursing facility care, hospice care, and home health care. Part B (Medical Insurance): Helps cover: Services from doctors and other health care providers. Outpatient care. Home health care.
What is Medicare Part B?
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services. Part B also covers some preventive services. Look at your Medicare card to find out if you have Part B.
What's the difference between Medicare Part A and Part B?
If you're wondering what Medicare Part A covers and what Part B covers: Medicare Part A generally helps pay your costs as a hospital inpatient. Medicare Part B may help pay for doctor visits, preventive services, lab tests, medical equipment and supplies, and more.
Does Medicare Part A pay 100 of hospitalization?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
What is the Medicare Part A deductible?
Part A Deductible: The deductible is an amount paid before Medicare begins to pay its share. The Part A deductible for an inpatient hospital stay is $1,556 in 2022. The Part A deductible is not an annual deductible; it applies for each benefit period.
What is meant by benefit period?
What Is a Benefit Period? A benefit period is the length of time during which an insurance policyholder or their dependents may file and receive payment for a covered event. All insurance plans will include a benefit period, which can vary based on policy type, insurance provider, and policy premium.
What are Medicare covered services?
Medicare-covered hospital services include: Semi-private rooms. Meals. General nursing. Drugs as part of your inpatient treatment (including methadone to treat an opioid use disorder) Other hospital services and supplies as part of your inpatient treatment.
How many days of inpatient care is in a psychiatric hospital?
Inpatient mental health care in a psychiatric hospital is limited to 190 days in a lifetime.
What is an inpatient hospital?
Inpatient hospital care. You’re admitted to the hospital as an inpatient after an official doctor’s order, which says you need inpatient hospital care to treat your illness or injury. The hospital accepts Medicare.
How many days in a lifetime is mental health care?
Things to know. Inpatient mental health care in a psychiatric hospital is limited to 190 days in a lifetime.
Who approves your stay in the hospital?
In certain cases, the Utilization Review Committee of the hospital approves your stay while you’re in the hospital.
Why are hospitals required to make public charges?
Hospitals are required to make public the standard charges for all of their items and services (including charges negotiated by Medicare Advantage Plans) to help you make more informed decisions about your care.
How to know if Medicare will cover you?
Talk to your doctor or other health care provider about why you need certain services or supplies. Ask if Medicare will cover them. You may need something that's usually covered but your provider thinks that Medicare won't cover it in your situation. If so, you'll have to read and sign a notice. The notice says that you may have to pay for the item, service, or supply.
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
Is Medicare Advantage the same as Original Medicare?
What's covered? Note. If you're in a Medicare Advantage Plan or other Medicare plan, your plan may have different rules. But, your plan must give you at least the same coverage as Original Medicare. Some services may only be covered in certain settings or for patients with certain conditions.
What is covered by Medicare Part A?
2021 Medicare Part A coverage for an inpatient hospital typically includes: 1 semi-private rooms 2 meals 3 nursing care 4 drugs 5 medical equipment that a doctor uses during the inpatient stay 6 rehabilitation services, such as physical therapy
How many quarters does Medicare cover?
Medicare Part A plans are free for people who have worked for 40 quarters and paid Medicare tax. According to the United States Census Bureau, Medicare plans provided coverage to approximately 17.9% of the population in 2018. In this article, we define what Medicare Part A covers and its cost.
What is the Medicare deductible for inpatient hospital stays in 2021?
People who use their Medicare Part A coverage for inpatient hospital stays still have to meet their deductible before Medicare funds any treatment. In 2021, this deductible is $1,484.
How much does Medicare pay for a skilled nursing home stay?
If an inpatient stay extends beyond 90 days, Medicare provides 60 reserve days that will cost a person $742 a day. Medicare Part A also covers skilled nursing home stays. However, the rules are different. There is no copayment for the first 20 days of the stay. Between days 21 and 100, the copayment is $185.50 per day.
How much does Medicare pay for an additional day?
For example, Medicare Part A covers the first 60 days of an inpatient stay. However, an individual will have to pay $371 for each additional day between 61 and 90 days.
What is Medicare 2021?
2021 coverage. Summary. Medicare is federal health insurance for people aged 65 years or older and for younger people with disabilities. There are four parts of Medicare: A, B, C, and D. Part A covers inpatient care, skilled nursing services, some home health and rehabilitation costs, and hospice care. Medicare Part A plans are free ...
How much does Medicare pay for a quarter?
Individuals who paid Medicare taxes for 30–39 quarters pay $259 a month for Medicare Part A. People who paid Medicare taxes for fewer than 30 quarters and those with certain disabilities who have reached their current benefit limits will need to pay $471 a month for Part A.
What is part A in hospital?
Long-term care hospital services. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Acute care hospitals that provide treatment for patients who stay, on average, more than 25 days. Most patients are transferred from an intensive or critical care unit.
How long does an acute care hospital stay?
Acute care hospitals that provide treatment for patients who stay, on average, more than 25 days. Most patients are transferred from an intensive or critical care unit. Services provided include comprehensive rehabilitation, respiratory therapy, head trauma treatment, and pain management. .
When does the benefit period end?
The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins. ...
How long does it take to get discharged from a long term care hospital?
You’re transferred to a long-term care hospital directly from an acute care hospital. You’re admitted to a long-term care hospital within 60 days of being discharged from a hospital.
Can long term care hospitals accept patients?
During the COVID-19 pandemic, long-term acute-care hospitals can now accept any a cute-care hospital patients.
Do you have to pay a deductible for long term care?
Each day after the lifetime reserve days: All costs. *You don’t have to pay a deductible for care you get in the long-term care hospital if you were already charged a deductible for care you got in a prior hospitalization within the same benefit period.