How many people have Medicare Part D?
In 2019, 47 million beneficiaries were enrolled in Part D, which represents three-quarters of Medicare beneficiaries. Part D benefits are provided through private plans approved by the federal government. The number of offered plans varies geographically, but a typical enrollee will have dozens of options to choose from.
What does Medicare Part D cover for medications?
Part D covers medications you get at your local pharmacy, mail order, or other pharmacies. You must be enrolled in either Medicare Part A or Part B to join a Part D plan, and individual Part D plans offer different levels of coverage. The plan you choose will determine how much you pay.
Are there individual Part D plans available to me?
Individual Part D plans available to you are based on where you live, and costs vary by plan. Different plans are offered in different locations, and costs can vary greatly.

Is Medicare Part D for everyone?
Medicare Cost Plan Medicare offers prescription drug coverage for everyone with Medicare. This coverage is called “Part D.” There are 2 ways to get Medicare prescription drug coverage: 1.
What is Part D initial coverage limit?
$4,660CMS has released the following 2023 parameters for the defined standard Medicare Part D prescription drug benefit: Deductible: $505 (up from $480 in 2022); Initial coverage limit: $4,660 (up from $4,430 in 2022);
How many patients does Medicare cover?
64 million AmericansHow many Americans are covered by Medicare? Nearly 64 million Americans are currently covered by Medicare, and funding for the program accounted for more than 4% of the U.S. gross domestic product in 2020. Total Medicare spending stood at about $917 billion that year, and is expected to grow to $1.78 trillion in 2031.
Does Medicare Part D plans have maximum out-of-pocket?
Medicare Part D plans do not have an out-of-pocket maximum in the same way that Medicare Advantage plans do. However, Medicare Part D plans have what's called a “catastrophic coverage” phase, which works similar to an out-of-pocket maximum.
What are the 4 phases of Part D coverage?
Throughout the year, your prescription drug plan costs may change depending on the coverage stage you are in. If you have a Part D plan, you move through the CMS coverage stages in this order: deductible (if applicable), initial coverage, coverage gap, and catastrophic coverage.
How Does Part D coverage work?
You pay a monthly premium to an insurance carrier for your Part D plan. In return, you use the insurance carrier's network of pharmacies to purchase your prescription medications. Instead of paying full price, you will pay a copay or percentage of the drug's cost. The insurance company will pay the rest.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
What is the largest Medicare Advantage plan?
Best for size of network: UnitedHealthcare UnitedHealthcare is the largest provider of Medicare Advantage plans and offers plans in nearly three-quarters of U.S. counties. UnitedHealthcare also partners with AARP, insuring the Medicare products that carry the AARP name.
What percentage of the population is on Medicare?
Currently, 44 million beneficiaries—some 15 percent of the U.S. population—are enrolled in the Medicare program. Enrollment is expected to rise to 79 million by 2030. Only one in 10 beneficiaries relies solely on the Medicare program for health care coverage.
How Much Does Part D cover?
The national base beneficiary premium for Part D plans is $33.37 per month in 2022, according to the Centers for Medicare & Medicaid Services, which calculates this number in part by using the national average monthly bid amount submitted by private insurers.
Is Medicare Part D worth getting?
Most people will need Medicare Part D prescription drug coverage. Even if you're fortunate enough to be in good health now, you may need significant prescription drugs in the future. A relatively small Part D payment entitles you to outsized benefits once you need them, just like with a car or home insurance.
Why is Medicare Part D so expensive?
Another reason some prescriptions may cost more than others under Medicare Part D is that brand-name drugs typically cost more than generic drugs. And specialty drugs used to treat certain health conditions may be especially expensive. Read more about generic vs. brand-name medications.
What does Medicare Part D cover?
All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes,” like drugs to treat cancer or HIV/AIDS. A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary.
How many drugs does Medicare cover?
All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug. However, in most cases, a similar drug should be available.
What happens if you don't use a drug on Medicare?
If you use a drug that isn’t on your plan’s drug list, you’ll have to pay full price instead of a copayment or coinsurance, unless you qualify for a formulary exception. All Medicare drug plans have negotiated to get lower prices for the drugs on their drug lists, so using those drugs will generally save you money.
How many prescription drugs are covered by Medicare?
Plans include both brand-name prescription drugs and generic drug coverage. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes. This helps make sure that people with different medical conditions can get the prescription drugs they need. All Medicare drug plans generally must cover at least 2 drugs per ...
Why does Medicare change its drug list?
Your plan may change its drug list during the year because drug therapies change, new drugs are released, or new medical information becomes available.
What is a drug plan's list of covered drugs called?
A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary. Many plans place drugs into different levels, called “tiers,” on their formularies. Drugs in each tier have a different cost. For example, a drug in a lower tier will generally cost you less than a drug in a higher tier.
What are the tiers of Medicare?
Here's an example of a Medicare drug plan's tiers (your plan’s tiers may be different): Tier 1—lowest. copayment. An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug.
What percentage of Medicare Part D plans are standalone?
A majority of those enrolled in Part D plans, 58 percent , choose standalone plans. In 2020, just five plans provided coverage to 88 percent of Part D enrollees. Every private plan offering Part D must be approved by Medicare. Read on to discover what Medicare Part D is, what it covers, and how to know what you will pay in 2021.
What are the requirements for Medicare Part D?
Part D eligibility requirements are the same as those for original Medicare and include those who: 1 are age 65 or older 2 have received Social Security disability payments for at least 24 months 3 have a diagnosis of amyotrophic lateral sclerosis (ALS) 4 have a diagnosis of end stage renal disease (ESRD) or kidney failure 5 have received Social Security disability for at least 24 months
What is Part D insurance?
Part D provides the most comprehensive prescription medication coverage for outpatient needs. Part D covers medications you get at your local pharmacy, mail order, or other pharmacies.
How much is the deductible for Part D 2021?
Deductible. In 2021, guidelines say the deductible can’t be more than $445 for any Part D plan. You can choose plans that have $0 deductible based on the medications you take. For example, some Part D plans offer tier 1 and 2 medications with no deductible.
How many tiers are there in Part D?
The medications at the bottom of the pyramid are less expensive and the ones at the very top are the most expensive. Most plans have four to six tiers.
What to do if your medication isn't covered by Medicare?
In some cases, if your medication isn’t covered or if coverage is dropped for your medication, you can appeal to the plan for an exception. You can either call the number on your card for your plan or use Medicare’s list of contacts who may help you.
What is tier 3 in Medicare?
Tier 3: non-preferred brand medications. Tier 4 and higher: specialty, select, high-cost medications. Medications on the tiers can be different for each plan, so it’s good to know where your medications fall within the tier system of the specific plan you are considering.
What is Medicare Part D?
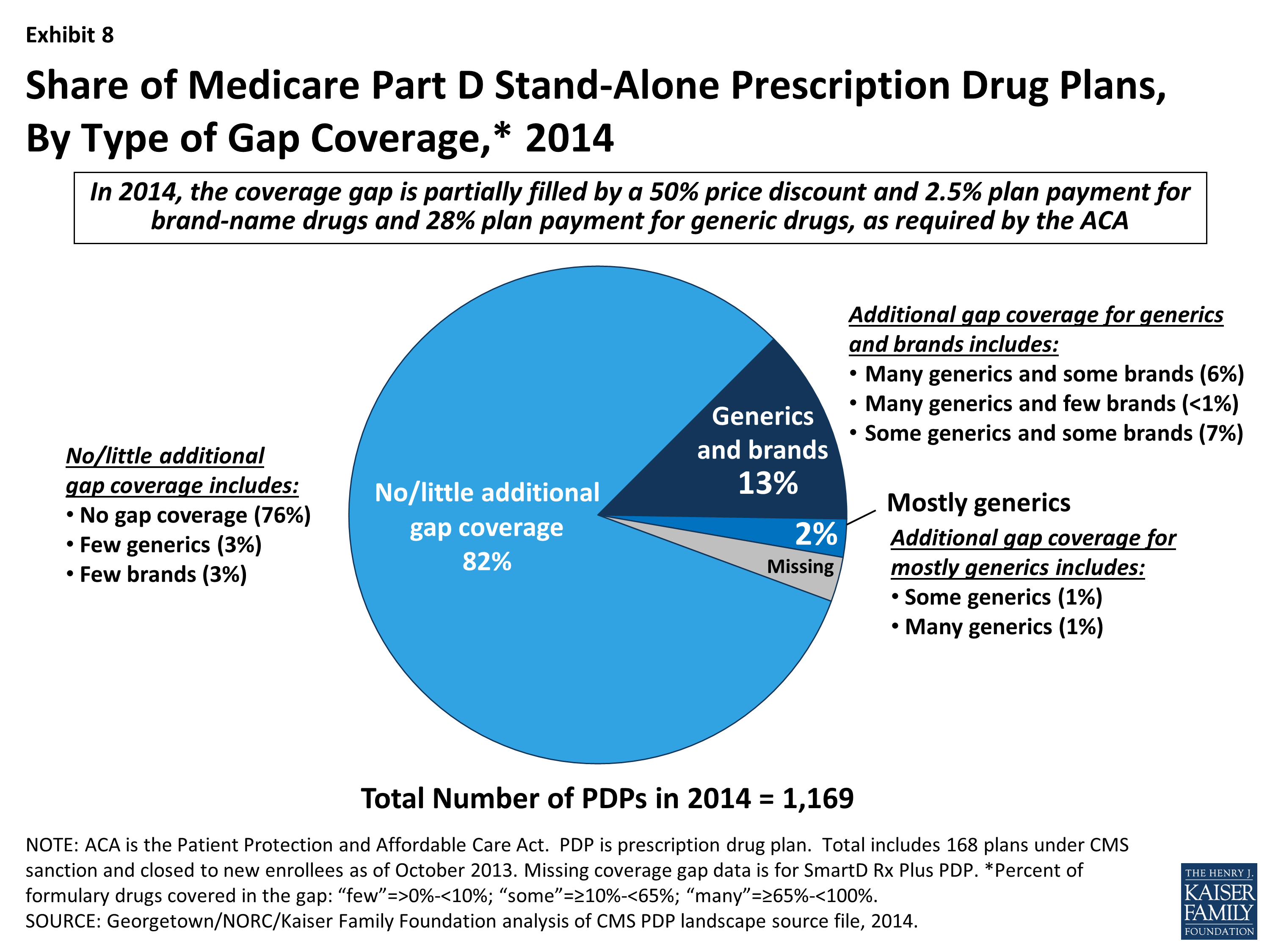
Medicare Part D is a voluntary outpatient prescription drug benefit for people with Medicare, provided through private plans approved by the federal government. Beneficiaries can choose to enroll in either a stand-alone prescription drug plan (PDP) to supplement traditional Medicare or a Medicare Advantage prescription drug plan (MA-PD), mainly HMOs and PPOs, that cover all Medicare benefits including drugs. In 2020, 46 million of the more than 60 million people covered by Medicare are enrolled in Part D plans. This fact sheet provides an overview of the Medicare Part D program, plan availability, enrollment, and spending and financing, based on data from the Centers for Medicare & Medicaid Services (CMS), the Congressional Budget Office (CBO), and other sources.
What are the requirements for a Part D plan?
Part D plans must offer either the defined standard benefit or an alternative equal in value (“actuarially equivalent”) and can also provide enhanced benefits. Both basic and enhanced benefit plans vary in terms of their specific benefit design, coverage, and costs, including deductibles, cost-sharing amounts, utilization management tools (i.e., prior authorization, quantity limits, and step therapy), and formularies (i.e., covered drugs). Plan formularies must include drug classes covering all disease states, and a minimum of two chemically distinct drugs in each class. Part D plans are required to cover all drugs in six so-called “protected” classes: immunosuppressants, antidepressants, antipsychotics, anticonvulsants, antiretrovirals, and antineoplastics.
What is the LIS for Part D?
Beneficiaries with low incomes and modest assets are eligible for assistance with Part D plan premiums and cost sharing. Through the Part D Low-Income Subsidy (LIS) program, additional premium and cost-sharing assistance is available for Part D enrollees with low incomes (less than 150% of poverty, or $19,320 for individuals/$26,130 for married couples in 2021) and modest assets (less than $14,790 for individuals/$29,520 for couples in 2021).
How many Medicare beneficiaries will be in 2021?
In 2021, 48 million Medicare beneficiaries are enrolled in Medicare Part D plans, including employer-only group plans; of the total, half (50%) are enrolled in stand-alone PDPs and the other half (50%) are enrolled in Medicare Advantage drug plans (Figure 7). Another 1.1 million beneficiaries are estimated to have drug coverage through employer-sponsored retiree plans where the employer receives a subsidy from the federal government equal to 28% of drug expenses between $480 and $9,850 per retiree (in 2022). Several million beneficiaries are estimated to have other sources of drug coverage, including employer plans for active workers, FEHBP, TRICARE, and Veterans Affairs (VA). Another 12% of people with Medicare are estimated to lack creditable drug coverage.
What is the Part D plan for 2022?
In 2022, beneficiaries in each state will have the option to enroll in a Part D plan participating in an Innovation Center model in which enhanced drug plans cover insulin products at a monthly copayment of $35 in the deductible, initial coverage, and coverage gap phases of the Part D benefit. Participating plans do not have to cover all insulin products at the $35 monthly copayment amount, just one of each dosage form (vial, pen) and insulin type (rapid-acting, short-acting, intermediate-acting, and long-acting). In 2022, a total of 2,159 Part D plans will participate in this model, a 32% increase in participating plans since 2021. This total includes 33% of all PDPs (258 plans) and 38% of MA-PDs (1,901 plans, including segmented plans) available in 2022, including plans in the territories. Between 7 and 10 PDPs in each region are participating in the model, in addition to multiple MA-PDs (Figure 3).
How many PDPs will be available in 2022?
In 2022, 766 PDPs will be offered across the 34 PDP regions nationwide (excluding the territories), a substantial reduction of 230 PDPs (23%) from 2021 and the first drop in PDP availability since 2017 (Figure 1).
How much does Medicare pay for generic drugs?
For total drug costs above the catastrophic threshold, Medicare pays 80%, plans pay 15%, and enrollees pay either 5% of total drug costs or $3.95/$9.85 for each generic and brand-name drug, respectively.
How many parts does Medicare have?
Medicare is broken out into four parts.
What isn’t covered by Medicare?
Original Medicare covers the essentials, but there are a lot of services that aren’t covered such as:
How long does it take for Medicare to cover colonoscopy?
If you had a different screening for colorectal cancer called a flexible sigmoidoscopy, Medicare covers a screening colonoscopy if it is 48 months or longer after that test.
What is Medicare Part C?
Medicare Part C. Part C is also known as Medicare Advantage. Private health insurance companies offer these plans. When you join a Medicare Advantage plan, you still have Medicare. The difference is the plan covers and pays for your services instead of Original Medicare.
How often do you have to have a colonoscopy for Medicare?
Colonoscopies. Medicare covers screening colonoscopies. Test frequency depends on your risk for colorectal cancer: Once every 24 months if you have a high risk. Once every 10 years if you aren’t at high risk.
Does Medicare cover chiropractic care?
Medicare has some coverage for chiropractic care if it’s medically necessary. Part B covers a chiropractor’s manual alignment of the spine when one or more bones are out of position. Medicare doesn’t cover other chiropractic tests or services like X-rays, massage therapy or acupuncture.
Does Medicare cover hearing aids?
Hearing aids. Medicare doesn’t cover hearing aids or pay for exams to fit hearing aids. Some Medicare Advantage plans have benefits that help pay for hearing aids and fitting exams.
What is a copayment for Medicare?
A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug. for each drug. If you don't join a drug plan, Medicare will enroll you in one to make sure you don't miss a day of coverage.
What is Medicare program?
A Medicare program to help people with limited income and resources pay Medicare prescription drug program costs , like premiums, deductibles, and coinsurance. with your prescription drug costs. If you don't join a plan, Medicare will enroll you in one to make sure you don't miss a day of coverage.
Can you keep a Medigap policy?
Medigap policies can no longer be sold with prescription drug coverage, but if you have drug coverage under a current Medigap policy, you can keep it . If you join a Medicare drug plan, your Medigap insurance company must remove the prescription drug coverage under your Medigap policy and adjust your premiums. Call your Medigap insurance company for more information.
Is Medicare a creditable drug?
It may be to your advantage to join a Medicare drug plan because most Medigap drug coverage isn't creditable. You may pay more if you join a drug plan later.
Can you join Medicare with meds by mail?
This is a comprehensive health care program in which the Department of Veterans Affairs shares the cost of covered health care services and supplies with eligible beneficiaries. You may join a Medicare drug plan, but if you do, you won’t be able to use the Meds by Mail program which can give your maintenance drugs to you at no charge (no premiums, deductibles, and copayments). For more information, visit va.gov/communitycare/programs/dependents/champva/ or call CHAMPVA at 800-733-8387.
Does Medicare help with housing?
, you won't lose your housing assistance. However, your housing assistance may be reduced as your prescription drug spending decreases.
Does Medicare cover drug costs?
Your drug costs are covered by Medicare. You'll need to join a Medicare drug plan for Medicare to pay for your drugs.
How much of Medicare is covered by Part D?
In 2019, about three-quarters of Medicare enrollees obtained drug coverage through Part D. Program expenditures were $102 billion, which accounted for 12% of Medicare spending. Through the Part D program, Medicare finances more than one-third of retail prescription drug spending in the United States.
How many Medicare beneficiaries are enrolled in Part D?
Medicare beneficiaries who delay enrollment into Part D may be required to pay a late-enrollment penalty. In 2019, 47 million beneficiaries were enrolled in Part D, which represents three-quarters of Medicare beneficiaries.
What is Medicare Part D?
Medicare Part D, also called the Medicare prescription drug benefit, is an optional United States federal-government program to help Medicare beneficiaries pay for self-administered prescription drugs.
What is Medicare online tool?
Medicare offers an interactive online tool that allows for comparison of coverage and costs for all plans in a geographic area. The tool lets users input their own list of medications and then calculates personalized projections of the enrollee's annual costs under each plan option. Plans are required to submit biweekly data updates that Medicare uses to keep this tool updated throughout the year.
Why did Medicare repeal the Catastrophic Coverage Act?
However, this legislation was repealed just one year later, partially due to concerns regarding premium increases. The 1993 Clinton Health Reform Plan also included an outpatient drug benefit, but that reform effort ultimately failed due to a lack of public support.
How does Part D cover drug costs?
Part D enrollees cover a portion of their own drug expenses by paying cost-sharing. The amount of cost-sharing an enrollee pays depends on the retail cost of the filled drug, the rules of their plan, and whether they are eligible for additional Federal income-based subsidies. Prior to 2010, enrollees were required to pay 100% of their retail drug costs during the coverage gap phase, commonly referred to as the "doughnut hole.” Subsequent legislation, including the Affordable Care Act, “closed” the doughnut hole from the perspective of beneficiaries, largely through the creation of a manufacturer discount program.
When did Medicare start covering prescription drugs?
Upon enactment in 1965 , Medicare included coverage for physician-administered drugs, but not self-administered prescription drugs. While some earlier drafts of the Medicare legislation included an outpatient drug benefit, those provisions were dropped due to budgetary concerns. In response to criticism regarding this omission, President Lyndon Johnson ordered the formation of the Task Force on Prescription Drugs. The Task Force conducted a comprehensive review of the American prescription drug market and reported that many elderly Americans struggled to afford their medications.

Medicare Prescription Drug Plan Availability in 2022
Low-Income Subsidy Plan Availability in 2022
Part D Plan Premiums and Benefits in 2022
Part D and Low-Income Subsidy Enrollment
Part D Spending and Financing
- Part D Spending
The Congressional Budget Office (CBO) estimates that spending on Part D benefits will total $111 billion in 2022, representing 15% of net Medicare outlays (net of offsetting receipts from premiums and state transfers). Part D spending depends on several factors, including the total number of Part D enrollees, their health status and drug … - Part D Financing
Financing for Part Dcomes from general revenues (73%), beneficiary premiums (15%), and state contributions (11%). The monthly premium paid by enrollees is set to cover 25.5% of the cost of standard drug coverage. Medicare subsidizes the remaining 74.5%, based on bids submitted by plans for their expected benefit payments…
Issues For The Future