What is Medicare terminology?
Government dollars extended to healthcare facilities for the treatment of a patient or patients meeting certain criteria. Medicare Terminology _Group Health Plan (GHP) - Any health plan that is offered to employees and their families by an employer. Medicare Terminology _ Liability Insurance
What are the four parts of Medicare?
Medicare is divided into four Parts: A, B, C and D. Part A covers hospital (inpatient, formally admitted only), skilled nursing (only after being formally admitted to a hospital for three days and not for custodial care), and hospice services.
What is Medicare and how does it work?
Medicare is a social insurance program administered by the United States government, providing health insurance coverage to people who are aged 65 and over, or who meet other special criteria. Cahaba is the Medical Center's Medicare Administrative Contractor
What information is on a Medicare card?
Each Medicare enrollee receives a health insurance card. This card lists the beneficiary's name, sex, and Medicare number and the effective dates for Part A and Part B coverage.

Which organization can reference the Medicare Claims Processing Manual?
the National Uniform Claim Committee (NUCC)Providers sending professional and supplier claims to Medicare on paper must use Form CMS-1500 in a valid version. This form is maintained by the National Uniform Claim Committee (NUCC), an industry organization in which CMS participates.
Does Medicare require a referring provider?
Which Medicare plans require referrals? Original Medicare (parts A and B) doesn't require referrals for specialist care. However, if you have Part A or Part B coverage through a Medicare Advantage (Part C) plan, you may need a referral before seeing a specialist.
What is reference lab billing?
“Reference laboratory” - A Medicare-enrolled laboratory that receives a specimen from another, referring laboratory for testing and that actually performs the test. “Billing laboratory” - The laboratory that submits a bill or claim to Medicare. “Service” - A clinical diagnostic laboratory test.
Who adjudicates Medicare claims?
Administrative Law Judge (ALJ) – Adjudicator employed by the Department of Health and Human Services (HHS), Office of Medicare Hearings and Appeals (OMHA) that holds hearings and issues decisions related to level 3 of the appeals process.
Who is a referring provider?
The Referring Provider is the individual who directed the patient for care to the provider rendering the services being reported.
What are CMS guidelines for referrals?
In a CMS compliant situation, you would 1) ask for referrals without mentioning any benefit to the enrollee and then 2) present a thank-you gift for the referrals he or she has provided. Second, the gifts you provide must be of a nominal value.
What are the use of reference laboratories?
A national reference laboratory is required to implement quality assurance and, in many cases, is the main facility where testing for resistance to first and second-line drugs is done. The NRL also interacts with the Supranational Reference Laboratory Network (SNRL).
What are the functions of a reference laboratory?
Important functions of NRLs include the provision of guidance and support to clinical laboratories in the surveillance system for adopting national standards and protocols for microbiological analysis.
What is another name for a reference laboratory?
a laboratory that performs reference or calibration measurement procedures or assigns reference values to test objects, later potentially providing those associated reference values for references or sources of traceability of test results; alternate names include: reference measurement, reference testing, and ...
How do providers submit claims to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
What are the five steps in the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
What organization is responsible for claim content?
Organization that is responsible for claim content. The NUCC is led by the American Medical Association (AMA), and determines the content of both HIPAA and CMS-1500 claims.
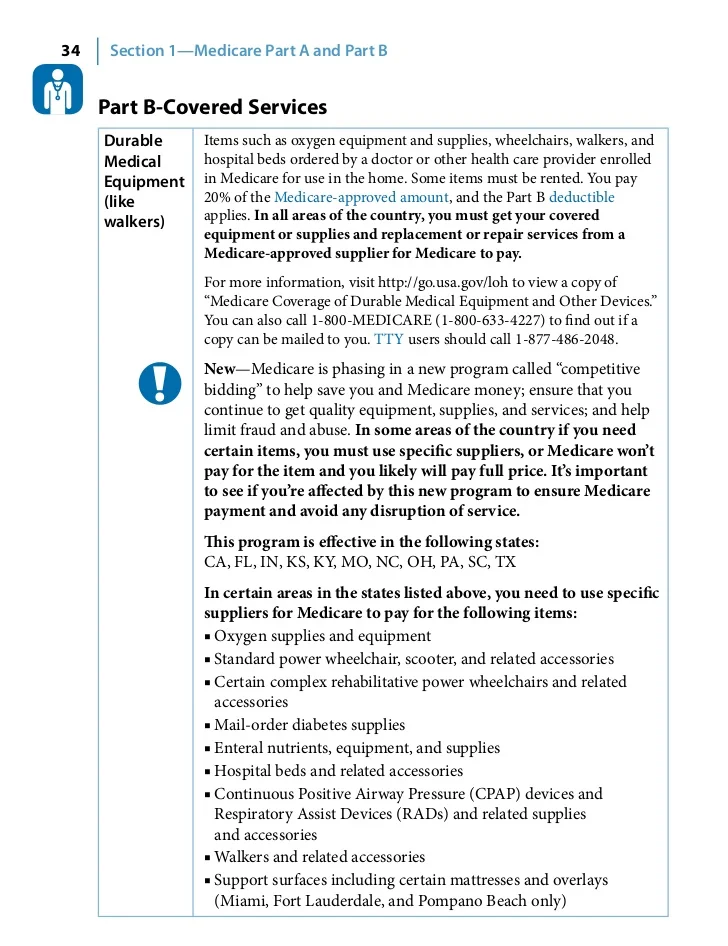
Lift Chairs
All of the following criteria must be met in order to consider coverage:
Support Surfaces
Group 1 (overlays) Group 2 (pressure reducing) Group 3 (air-fluidized bed)
Mobility Equipment
What are the rules? Remember you must rule out each lower level item. Medicare pays for the least costly alternative.
Non-invasive Ventilators
Non-invasive ventilator treatment is generally covered if treatment is needed for:
Oxygen and Oxygen Equipment
The key is to make sure there is documentation in the medical record indicating need for home oxygen therapy
Positive Airway Pressure Devices (PAP)
For Positive Airway Pressure or BiPAP without backup -- the only diagnosis that is covered is obstructive sleep apnea (OSA), G47.33
What is a Medicare reference number?
A Medicare Reference Number is a number that represents the position of a person on a Medicare card. For example, a person who is listed second on a Medicare Card has an IRN of 2.
Where is the Medicare card number?
While your Individual Reference Number is the number to the left of your name on your card, your Medicare Card Number is the 10 digit number that appears above your name, across the top section of the card.
What is Medicare for people over 65?
Medicare is a health insurance program for: people age 65 or older, . people under age 65 with certain disabilities, and . people of all ages with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a kidney transplant) Medicare has: Part A Hospital Insurance . Part B Medical Insurance.
What is Medicare Part B?
Medicare Part B (Medical Insurance) covers ambulance services to or from a hospital, critical access hospital, or a skilled nursing facility only when other transportation could endanger a patients health. RAC - Recovery Audit Contractor.
How long is a Medicare benefit period?
Medicare Part A 7. The benefit period ends with the close of a period of 60 consecutive days during which the patient was neither an inpatient of a hospital nor of a SNF. To determine the 60 consecutive day period, begin counting with the day the individual was discharged. Medicare Part A 8.
What is change in patient status from inpatient to outpatient?
The change in patient status from inpatient to outpatient is made prior to discharge or release, while the beneficiary is still a patient of the hospital; . The hospital has not submitted a claim to Medicare for the inpatient admission; . A physician concurs with the utilization review committee's decision; and .
What is the 72 hour rule for Medicare?
72 Hour Rule. Violation of the 72 Hour Rule could lead to exclusion from the Medicare Program, criminal fines and imprisonment, and civil liability.
What field is Y in Medicare?
Anytime a Medicare /Medicaid outpatient or emergency account is re-billed, Y must be entered in the APC Critical Bypass Field. If charges are entered after Medicare or Medicaid has paid on an outpatient account and intend to re-bill the account, enter Y in the APC Critical Bypass Field.
How long is a hospital stay deductible?
For any hospital stay that lasts longer than 150 days within a single benefit period, you will be required to pay the full cost for each day after the 150th day.
Who is responsible for Medicare eligibility?
The Social Security Administration (SSA) is responsible for determining Medicare eligibility, eligibility for and payment of Extra Help/Low Income Subsidy payments related to Parts C and D of Medicare, and collecting most premium payments for the Medicare program.
Who decides if a hospital is eligible for Medicare?
In most states the Joint Commission, a private, non-profit organization for ac crediting hospitals, decides whether or not a hospital is able to participate in Medicare, as currently there are no competitor organizations recognized by CMS.
What is CMS in healthcare?
The Centers for Medicare and Medicaid Services (CMS), a component of the U.S. Department of Health and Human Services (HHS), administers Medicare, Medicaid, the Children's Health Insurance Program (CHIP), the Clinical Laboratory Improvement Amendments (CLIA), and parts of the Affordable Care Act (ACA) ("Obamacare").
How much does Medicare cost in 2020?
In 2020, US federal government spending on Medicare was $776.2 billion.
What is Medicare and Medicaid?
Medicare is a national health insurance program in the United States, begun in 1965 under the Social Security Administration (SSA) and now administered by the Centers for Medicare and Medicaid Services (CMS). It primarily provides health insurance for Americans aged 65 and older, ...
How is Medicare funded?
Medicare is funded by a combination of a specific payroll tax, beneficiary premiums, and surtaxes from beneficiaries, co-pays and deductibles, and general U.S. Treasury revenue. Medicare is divided into four Parts: A, B, C and D.
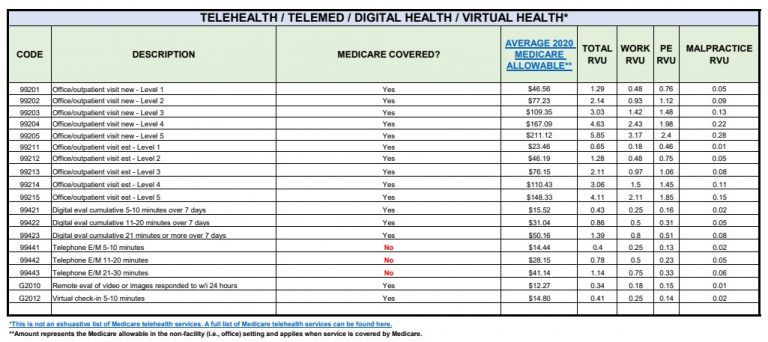
What is a RUC in medical?
The Specialty Society Relative Value Scale Update Committee (or Relative Value Update Committee; RUC), composed of physicians associated with the American Medical Association, advises the government about pay standards for Medicare patient procedures performed by doctors and other professionals under Medicare Part B.