A prior or pre-existing condition is a condition or illness you were diagnosed with or were treated for before new health care coverage began. The wait time for your Medigap
Medigap
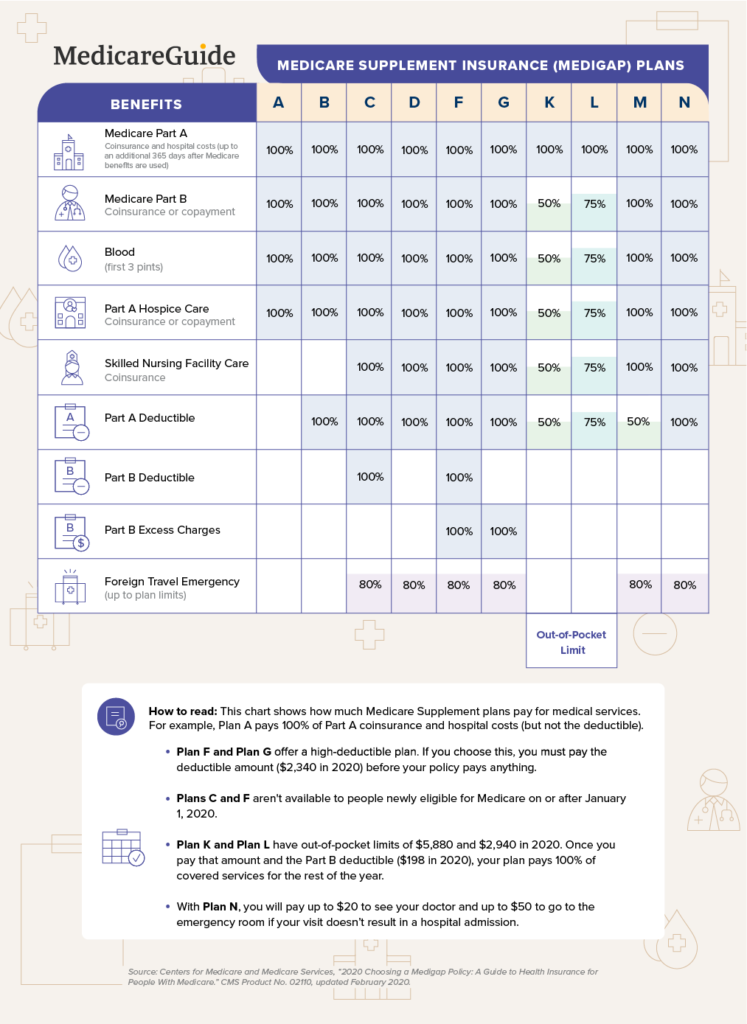
Medigap refers to various private health insurance plans sold to supplement Medicare in the United States. Medigap insurance provides coverage for many of the co-pays and some of the co-insurance related to Medicare-covered hospital, skilled nursing facility, home health care, ambulance, durable medical equipment, and doctor charges. Medigap's name is derived from the notion that it exists to …
What does health insurance pre-existing condition coverage mean for You?
What This Means for You. Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer. They cannot limit benefits for that condition either.
Can insurance companies refuse to cover pre-existing conditions?
Pre-Existing Conditions. Under current law, health insurance companies can’t refuse to cover you or charge you more just because you have a “pre-existing condition” — that is, a health problem you had before the date that new health coverage starts.
Does the ACA have a pre-existing condition exclusion period?
So in spite of pre-existing health conditions in his family, Greg’s health plan was not able to impose a pre-existing condition exclusion period. Now that the ACA has been implemented, Greg's employer cannot impose a pre-existing condition waiting periods on any new enrollees, regardless of their medical history or health insurance history.
What is the pre-existing Condition Insurance Plan (PCIP)?
The Pre-existing Condition Insurance Plan (PCIP) ended on April 30, 2014. The PCIP program provided health coverage options to individuals who were uninsured for at least six months, had a pre-existing condition, and had been denied coverage (or offered insurance without coverage of the pre-existing condition) by a private insurance company.

Can Medicare Supplement plans deny for pre-existing conditions?
A Medicare Supplement insurance plan may not deny coverage because of a pre-existing condition. However, a Medicare Supplement plan may deny you coverage for being under 65. A health problem you had diagnosed or treated before enrolling in a Medicare Supplement plan is a pre-existing condition.
What does Medicare consider a pre-existing condition?
See Plans. Medicare defines a pre-existing condition as any health problem that you had prior to the coverage start date for a new insurance plan. If you have Original Medicare or a Medicare Advantage plan, you are generally covered for all Medicare benefits even if you have a pre-existing condition.
How long can an insurer exclude coverage for a pre-existing condition on a Medicare Supplement?
within 6 monthsCoverage for the pre-existing condition can be excluded if the condition was treated or diagnosed within 6 months before the coverage starts under the Medigap policy. After this 6-month period, the Medigap policy will cover the condition that was excluded.
What classifies as a pre-existing condition?
As defined most simply, a pre-existing condition is any health condition that a person has prior to enrolling in health coverage. A pre-existing condition could be known to the person – for example, if she knows she is pregnant already.
What pre-existing conditions are not covered?
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy. They cannot limit benefits for that condition either.
Are pre-existing conditions covered?
You can still get health insurance cover if you have pre-existing medical conditions, but it is unlikely your policy will provide cover for them. The type of underwriting of your health plan determines whether your pre-existing conditions will be covered in the future.
Do Medicare Supplement policies have pre-existing conditions?
A Medicare Supplement insurance plan may not deny coverage because of a pre-existing condition. However, a Medicare Supplement plan may deny you coverage for being under 65. A health problem you had diagnosed or treated before enrolling in a Medicare Supplement plan is a pre-existing condition.
How long can an insurer exclude coverage for a pre-existing condition on a Medicare Supplement policy quizlet?
A Medicare Supplement policy can't deny or limit coverage for a preexisting condition more than 6 months after effective date of coverage.
How long is pre-existing condition?
The time period during which a health plan won't pay for care relating to a pre-existing condition. Under a job-based plan, this cannot exceed 12 months for a regular enrollee or 18 months for a late-enrollee.
What is a pre-existing condition quizlet?
Definition. HIPAA has defined pre-existing conditions to be health issues that have existed, treated of diagnosed within the last 6 months prior to employment.
Is high blood pressure considered pre-existing condition?
High blood pressure (also called hypertension) is a common pre-existing medical condition, and can be covered by your policy - but you need to meet the conditions below.
What is the difference between existing and pre-existing?
A. You can use pre- in ways that are redundant, but it's a valid prefix, and preexisting has its own meaning. For instance, if you want to describe dinosaurs in relation to humans, existing doesn't work, but preexisting does.
What is pre-ACA exclusion?
The Pre-ACA Pre-Existing Condition Exclusion. Pre-ACA, a pre-existing condition could affect your health insurance coverage. 1 If you were applying for insurance in the individual market, some health insurance companies would accept you conditionally by providing a pre-existing condition exclusion period, or a full exclusion on ...
What is creditable coverage?
Creditable coverage is health insurance coverage you had before you enrolled in your new health plan, as long as it was not interrupted by a period of 63 or more days.
What is HIPAA coverage?
In 1996, Congress passed the Health Insurance Portability and Accountability Act (HIPAA), a law that provides significant protection for you and your family members, particularly when you're enrolling in a plan offered by an employer. These protections include: 5 .
What are the protections of HIPAA?
In 1996, Congress passed the Health Insurance Portability and Accountability Act (HIPAA), a law that provides significant protection for you and your family members, particularly when you're enrolling in a plan offered by an employer. These protections include: 5 1 Limits on the use of pre-existing condition exclusions in employer-sponsored health plans. 2 Prevents employer-sponsored health plans from discriminating against you by denying you coverage or charging you more for coverage based on your or a family member's health problems. 3 Usually guarantees that if you purchase health insurance, you can renew your coverage regardless of any health conditions in your family.
How long was Greg's health insurance?
He had no coverage during the two weeks he was between jobs, and for the first month of his new job, but his uninsured duration was less than 63 days. So in spite of pre-existing health conditions in his family, Greg’s health plan was not able to impose a pre-existing condition exclusion period.
How long is a short term health plan?
Short-Term Health Plans: In addition, the new regulations for short-term health plans, which were finalized in August 2018 and took effect in October 2018, allow insurers to offer "short-term" plans with initial terms of up to 364 days, and total duration, including renewals, of up to three years. 9 .
When will the ACA be repealed?
Some of the ACA's taxes (the medical device tax, the Cadillac tax, and the health insurance tax) were repealed by Congress in 2019, with the repeals effective in 2020 and 2021.
What is a pre-existing condition?
A prior or pre-existing condition is a condition or illness you were diagnosed with or were treated for before new health care coverage began. The wait time for your Medigap coverage to start is called a pre-existing condition waiting period.
How long does Medigap cover medical conditions?
If you had six or more months of prior credit able coverage, Medigap insurers must cover your prior medical conditions immediately. Keep in mind that you cannot use creditable coverage to reduce your pre-existing waiting period if you had a break in coverage of more than 63 days.
Can you have a waiting period on a health insurance policy?
You can avoid such waiting periods if you buy your policy when you have a guaranteed issue right. If you buy your policy when you have a guaranteed issue right, the insurer cannot impose a waiting period for coverage of any prior medical condition.
Can you shorten your Medigap waiting period?
You can also avoid or shorten a pre-existing condition waiting period if you buy a policy during your open enrollment period. During this protected period, Medigap policies must shorten any pre-existing condition waiting period by the number of months you had prior creditable coverage.
What are pre-existing conditions?
What’s a pre-existing condition? 1 A pre-existing condition is a health problem you had before the date that your new health coverage starts. 2 Pre-existing conditions include epilepsy, cancer, diabetes, lupus, sleep apnea, and many more.
Can I get insurance for pregnancy?
Yes. If you were pregnant before you applied, your insurance plan can't reject you or charge you more because of your pregnancy. Once you're enrolled, your pregnancy and childbirth are covered from the day your plan starts. Get more information on coverage for pregnancy and childbirth. Previous Post. Next Post.
How long after birth can you change your health insurance?
Your coverage can start from the date of birth or adoption, even if you enroll up to 60 days afterward. Learn more about coverage for pregnancy and childbirth.
Can you refuse Medicaid coverage?
Medicaid and the Children's Health Insurance Program (CHIP) also can't refuse to cover you or charge you more because of your pre-existing condition.
Can Marketplace insurance reject you?
Getting Coverage. All Marketplace plans must cover treatment for pre-existing medical conditions. No insurance plan can reject you, charge you more, or refuse to pay for essential health benefits for any condition you had before your coverage started. Once you’re enrolled, the plan can’t deny you coverage or raise your rates based only on your ...
Is pregnancy covered by insurance?
Pregnancy is covered from the day your plan starts. If you’re pregnant when you apply, an insurance plan can’t reject you or charge you more because of your pregnancy . Once you’re enrolled, your pregnancy and childbirth are covered from the day your plan starts.
Do grandfathered plans cover pre-existing conditions?
Grandfathered plans don’t have to cover pre-existing conditions or preventive care. If you have a grandfathered plan and want pre-existing conditions covered, you have 2 options: You can switch to a Marketplace plan that will cover them during Open Enrollment. You can buy a Marketplace plan outside Open Enrollment when your grandfathered plan year ...
What is a pre-existing condition?
Under the “objective standard” definition, a pre-existing condition is any condition for which the patient has already received medical advice or treatment before enrollment in a new medical insurance plan. Under the broader, “prudent person” definition, a pre-existing condition is anything for which symptoms were present, ...
What does it mean when an insurance underwriter limits your pre-existing conditions?
In short, insurance underwriters are limiting their risks (and costs) by limiting the amount they will have to pay out for claims to cover known medical conditions. Some providers will grant coverage ...
What is acute onset?
The Acute Onset or Recurrence of a Pre-Existing Condition is the sudden and unexpected outbreak, or recurrence, of a Pre-Existing Condition which occurs without warning. It is typically of short duration, rapidly progressive, and requires immediate care. For coverage to be effective, the Acute Onset of a Pre-Existing Condition must occur after ...
What age does Patriot Medical pay?
A typical clause may read: For US citizens up to age 65 with a primary health plan, Patriot Travel Medical will pay the Usual, Reasonable and Customary charges of a sudden and unexpected recurrence of a Pre-existing Condition (defined on the Exclusions page) up to the plan maximum. For those without a primary health plan, ...
Is a medical condition considered pre-existing?
“Any medical condition that the insured has before contracting for insurance coverage can be considered a pre-existing condition.”
Is a preexisting condition considered acute?
Important: A Pre-Existing Condition that is chronic, a congenital condition, or that gradually becomes worse over time will not be considered Acute Onset. Further, plans would exclude coverage for known, scheduled, required, or expected medical care, drugs or Treatments existent or necessary before the Effective Date of coverage.
Can I get pre-existing conditions after a lesser period?
Some providers will grant coverage for pre-existing conditions after a lesser period. Often, if you have “prior creditable coverage”, meaning another insurance plan in place at the time you apply for your new international plan, coverage for pre-existing conditions may be granted in even less time.
