How much does Medicare Part a cover long-term care?
Medicare Part A (Hospital Insurance) covers the cost of long-term care in a Long-term care hospital (LTCH). Days 1-60: $1,364 deductible.* D ays 61-90: $341 coinsurance each day. Days 91 and beyond: $682 coinsurance per each “lifetime reserve day” after day 90 for each benefit period (up to 60 days over your lifetime).
How much does it cost to get Medicare benefits every day?
Days 61–90: $389 coinsurance per day. Days 91 and beyond: $778 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to a maximum of 60 reserve days over your lifetime). Each day after the lifetime reserve days: All costs.
How much does Medicare pay for mental health care?
Mental health care (inpatient) provides coverage for mental health care services you get in a hospital that require you to be admitted as an inpatient. $1,364 Deductible [glossary] for each Benefit period . Days 1–60: $0 Coinsurance per day of each benefit period.
Do you have to pay a deductible for long-term care?
*You don’t have to pay a deductible for care you get in the long-term care hospital if you were already charged a deductible for care you got in a prior hospitalization within the same benefit period. This is because your benefit period starts on day one of your prior hospital stay, and that stay counts towards your deductible. For example:
Does Medicare cover ICU?
(Medicare will pay for a private room only if it is "medically necessary.") all meals. regular nursing services. operating room, intensive care unit, or coronary care unit charges.
How many days of hospitalization will Medicare pay for?
90 daysIn Original Medicare, these are additional days that Medicare will pay for when you're in a hospital for more than 90 days. You have a total of 60 reserve days that can be used during your lifetime. For each lifetime reserve day, Medicare pays all covered costs except for a daily coinsurance.
How much does Medicare reimburse for?
Medicare pays for 80 percent of your covered expenses. If you have original Medicare you are responsible for the remaining 20 percent by paying deductibles, copayments, and coinsurance. Some people buy supplementary insurance or Medigap through private insurance to help pay for some of the 20 percent.
How many days will Medicare pay 100% of the covered costs of care in a skilled nursing care facility?
20 daysSkilled Nursing Facility (SNF) Care Medicare pays 100% of the first 20 days of a covered SNF stay. A copayment of $194.50 per day (in 2022) is required for days 21-100 if Medicare approves your stay.
Is there a maximum amount Medicare will pay?
In general, there's no upper dollar limit on Medicare benefits. As long as you're using medical services that Medicare covers—and provided that they're medically necessary—you can continue to use as many as you need, regardless of how much they cost, in any given year or over the rest of your lifetime.
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
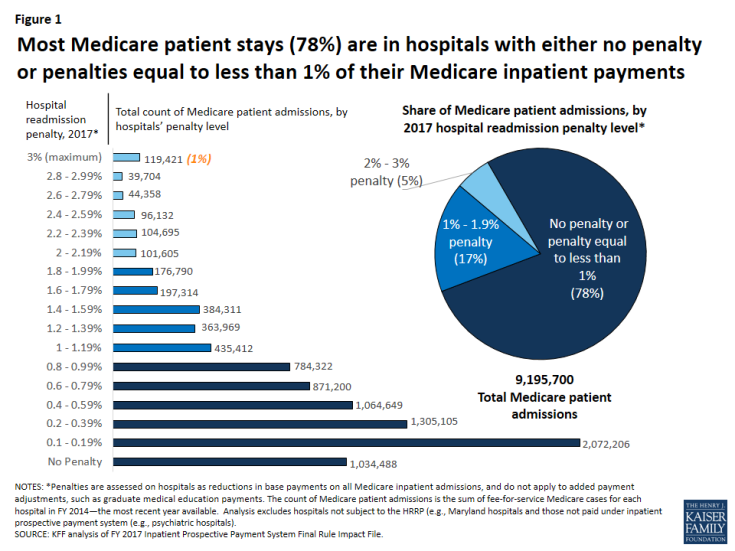
Do hospitals lose money on Medicare patients?
Privately insured patients and others often make up the difference. Payments relative to costs vary greatly among hospitals depending on the mix of payers. In 2015, two-thirds of hospitals lost money providing care to Medicare and Medicaid patients and nearly one-fourth lost money overall (see chart above).
Do doctors lose money on Medicare patients?
Summarizing, we do find corroborative evidence (admittedly based on physician self-reports) that both Medicare and Medicaid pay significantly less (e.g., 30-50 percent) than the physician's usual fee for office and inpatient visits as well as for surgical and diagnostic procedures.
How do you qualify for Medicare reimbursement?
A person must be age 65 or older; and. Be eligible for monthly Social Security or Railroad Retirement Board (RRB) cash benefits....Medicare Part A (Hospital Insurance) and Medicare Part B (Medical Insurance) are available to the individuals below:Age 65 or older.Disabled.End-Stage Renal Disease (ESRD)
What is the 21 day rule for Medicare?
For days 21–100, Medicare pays all but a daily coinsurance for covered services. You pay a daily coinsurance. For days beyond 100, Medicare pays nothing. You pay the full cost for covered services.
What is the 3 day rule for Medicare?
The 3-day rule requires the patient have a medically necessary 3-consecutive-day inpatient hospital stay. The 3-consecutive-day count doesn't include the discharge day or pre-admission time spent in the Emergency Room (ER) or outpatient observation.
What is the 100 day rule for Medicare?
Medicare pays for post care for 100 days per hospital case (stay). You must be ADMITTED into the hospital and stay for three midnights to qualify for the 100 days of paid insurance. Medicare pays 100% of the bill for the first 20 days.
What are Medicare covered services?
Medicare-covered hospital services include: Semi-private rooms. Meals. General nursing. Drugs as part of your inpatient treatment (including methadone to treat an opioid use disorder) Other hospital services and supplies as part of your inpatient treatment.
What does Medicare Part B cover?
If you also have Part B, it generally covers 80% of the Medicare-approved amount for doctor’s services you get while you’re in a hospital. This doesn't include: Private-duty nursing. Private room (unless Medically necessary ) Television and phone in your room (if there's a separate charge for these items)
What is an inpatient hospital?
Inpatient hospital care. You’re admitted to the hospital as an inpatient after an official doctor’s order, which says you need inpatient hospital care to treat your illness or injury. The hospital accepts Medicare.
How much does Medicare pay for a doctor's visit?
For example, you might pay $10 or $20 for a doctor's visit or prescription drug. for each emergency department visit and a copayment for each hospital service. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid.
What does Medicare Part B cover?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. usually covers emergency department services when you have an injury, a sudden illness, or an illness that quickly gets much worse.
Why don't you pay copays for emergency department visits?
If your doctor admits you to the same hospital for a related condition within 3 days of your emergency department visit, you don't pay the copayment because your visit is considered part of your inpatient stay.
What is an ICU nurse?
The ICU Nurse performs various diagnostic tests, administers medications, and develops patient care plans in conjunction with other medical professionals. Provides professional nursing care to assigned patients in the intensive care unit.
What is required to become an ICU nurse?
In addition, ICU Nurse requires of graduation from an approved nursing program. Typically reports to a manager or head of a unit/department. Requires a state license to practice. ICU Nurse 's years of experience requirement may be unspecified. Certification and/or licensing in the position's specialty is the main requirement.
What is the North Carolina region?
About North Carolina. North Carolina (/ˌkærəˈlaɪnə/ (listen)) is a state in the southeastern region of the United States. It borders South Carolina and Georgia to the south, Tennessee to the west, Virginia to the north, and the Atlantic Ocean to the east. North Carolina is the 28th-most extensive and the 9th-most populous of the U.S. states.
How many counties are there in North Carolina?
The state is divided into 100 counties. The capital is Raleigh, which along with Durham and Chapel Hill is home to the largest research park in the United States (Research Triangle Park). The most populous municipality is Charlotte, which is the second-largest banking center in... Source: Wikipedia (as of 04/11/2019).
How long does it take to get into an inpatient rehab facility?
You’re admitted to an inpatient rehabilitation facility within 60 days of being discharged from a hospital.
What is the benefit period for Medicare?
benefit period. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services. A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row.
Does Medicare cover private duty nursing?
Medicare doesn’t cover: Private duty nursing. A phone or television in your room. Personal items, like toothpaste, socks, or razors (except when a hospital provides them as part of your hospital admission pack). A private room, unless medically necessary.
Does Medicare cover outpatient care?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
How long does it take to get discharged from a long term care hospital?
You’re transferred to a long-term care hospital directly from an acute care hospital. You’re admitted to a long-term care hospital within 60 days of being discharged from a hospital.
How long does an acute care hospital stay?
Acute care hospitals that provide treatment for patients who stay, on average, more than 25 days. Most patients are transferred from an intensive or critical care unit. Services provided include comprehensive rehabilitation, respiratory therapy, head trauma treatment, and pain management. .
What is Medicare Part A?
Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. covers the cost of long-term care in a. long-term care hospital. Acute care hospitals that provide treatment for patients who stay, on average, more than 25 days.
Do you have to pay a deductible for long term care?
Each day after the lifetime reserve days: All costs. *You don’t have to pay a deductible for care you get in the long-term care hospital if you were already charged a deductible for care you got in a prior hospitalization within the same benefit period.
How long does a trauma team need to be on Medicare?
According to the Centers for Medicare & Medicaid Services (CMS), a trauma team must provide at least 30 minutes of critical care in order to bill for a trauma team activation. Many billers think this means 30 minutes of physician time. In fact, CMS regulations state that critical care time can include care delivered by either physicians ...
How long does a trauma team have to be in the hospital?
A trauma team must provide at least 30 minutes of critical care before the hospital can bill for a trauma activation, so failure to capture critical care charges will reduce trauma program revenue dramatically.
Can a trauma surgeon charge for critical care?
If a trauma surgeon spends only 20 minutes with a patient during an activation but the trauma team as a whole spends 45 minutes providing care: The surgeon cannot submit a professional charge for critical care . However, the hospital can submit a facility charge for critical care.
Does the hospital charge for trauma activation?
Since the patient received less than 30 minutes of critical care, the hospital cannot charge for a trauma activation. The same principles apply to patients who are DOA or who die in the ED soon after arrival.
Can a hospital report 68x revenue code without 99291?
However, the hospital can still report a 68x revenue code without G0390.
How long does a patient have to be in critical care for a trauma activation?
In order to bill the Center for Medicare & Medicaid Services (CMS) for a trauma activation, a patient must have received at least 30 minutes of critical care (CPT 99291). In some trauma centers, coders interpret this to mean 30 minutes of physician critical care.
Why are trauma centers important?
Trauma centers are known to improve patient outcomes and quality of care , so there is no reason that the care you provide should not positively impact reimbursement. When coding and billing are optimized, most trauma programs can become a key driver of hospital financial performance.
Is trauma activation reimbursable?
Here’s why: While the trauma activation is not reimbursable by CMS, it can still be captured in your Hospital Cost Report, which will help increase your hospital’s Medicare reimbursement overall by ensuring a higher case mix index (CMI).
Can hospitals reimburse beyond DRG?
Often hospitals don’t even pursue reimbursement beyond the DRG payment. As a result, the trauma program misses out on legitimate reimbursement opportunities. While trauma center coding and billing are unique, they can be mastered with some attention from management.
Do hospitals have to follow CMS guidelines?
Hospitals must follow CMS guidelines when seeking CMS reimbursement for trauma care. However, many hospitals lose sight of the fact that private payers may have very different policies on trauma reimbursement. If you follow CMS guidelines when billing third-party payers, your center may be missing out on additional payment.
