This may be done up to two (2) days prior to the patient's anticipated discharge to their home. The supplier should bill the date of service on the claim as the date of discharge and shall use the place of service (POS) as 12 (patient's home). The item must be for subsequent use in the patient's home.
Full Answer
Can I get DME with Medicare?
Anyone who has Medicare Part B (Medical Insurance) can get DME as long as the equipment is medically necessary. When does Original Medicare cover DME?
Do I have any questions about billing for DME?
Generally speaking, this information applies to all payer types. However, it's always a good idea to check with the payer directly if you have any questions or concerns about billing for DME, prosthetics, or orthotic devices.
What is a Medicare DME agreement?
DME that Medicare covers includes, but isn't limited to: An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
What does Medicare Part B cover for DME?
Medicare Part B (Medical Insurance) covers Medically necessary durable medical equipment (DME) if your doctor prescribes it for use in your home. DME that Medicare covers includes, but isn't limited to: If your supplier accepts Assignment you pay 20% of the Medicare-approved amount, and the Part B Deductible applies.
What is a Medicare DME claim?
covers. medically necessary. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine. DME if your doctor prescribes it for use in your home.
What are the documentation guidelines for DME?
Documentation, including pertinent portions of the beneficiary's medical records (e.g., history, physical examination, diagnostic tests, summary of findings, diagnoses, treatment plans), supporting the medical necessity of the prescribed PMD must be furnished to the supplier within 45 days of the examination.
What is required when billing Medicare for repair of previously purchased equipment?
With respect to Medicare reimbursement for the repair, there are two documentation requirements: Treating physician/practitioner must document that the item being repaired continues to be reasonable and necessary. Treating physician or supplier must document that the repair itself is reasonable and necessary.
What does DME reimbursement mean?
Expenses incurred by a beneficiary are reimbursable by Medicare if the equipment meets the definition of DME; the equipment is necessary and reasonable for the treatment of the beneficiary's illness or injury; and the equipment is used in the beneficiary's home.
How do you write a DME prescription?
Your prescription can be handwritten on a standard prescription pad. It must include the physician's name, contact information and signature of the care provider; your name; and a statement about the equipment needed, for example "Oxygen at LPM" “CPAP” , “BiPAP”, “CPAP Mask”, “CPAP Humidifier” or “CPAP Supplies”.
What is the criteria for documentation of medical necessity?
Well, as we explain in this post, to be considered medically necessary, a service must: “Be safe and effective; Have a duration and frequency that are appropriate based on standard practices for the diagnosis or treatment; Meet the medical needs of the patient; and.
What is the POS for DME?
DME Suppliers The following POS codes would qualify as the patient's home: 01, 04, 09, 12, 13, 14, 16, 31, 32, 33, 54, 55, 56, and 65. DME suppliers should report the POS code where the device is intended to be used. DME dispensed for use in a POS other than the patient's home are not reimbursable.
Does DME need a modifier?
In addition to an appropriate HCPCS code for the DME item, many HCPCS codes require a modifier. The modifiers are used to provide more information about the item.
What is the purchase modifier for DME?
UEUE — USED DURABLE MEDICAL EQUIPMENT PURCHASE. This modifier is used for used DME items that are purchased. When using the UE modifier, you are indicating you have furnished the beneficiary with a used piece of equipment.
Which of the following is excluded from Medicare coverage?
Non-medical services, including a private hospital room, hospital television and telephone, canceled or missed appointments, and copies of x-rays. Most non-emergency transportation, including ambulette services. Certain preventive services, including routine foot care.
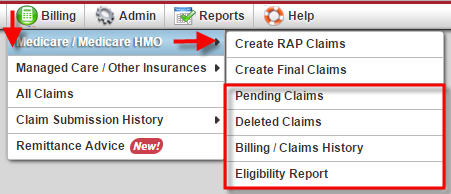
Where are Dmepos claims submitted to?
supply patients with durable medical equipment (DME) (e.g., canes, crutches); DMEPOS claims are submitted to DME Medicare administrative contractors (MACs) who are awarded contracts by CMS; each DME MAC covers a specific geographic region of the country and is responsible for processing DMEPOS claims for its specific ...
When will CMS reprocess claims?
Claims for these accessories submitted prior to July 1, 2020, with dates of service from January 1, 2020 through June 30, 2020, will need to be reprocessed to ensure that CMS pays the unadjusted fee schedule amounts, as required by section 106 of the Further Consolidated Appropriations Act, 2020.
When will Medicare change the KU modifier?
As aforementioned, these system changes will be implemented on July 1, 2020.
What is Medicare Accessibility Act?
CMS is implementing the Patient Access and Medicare Protection Act to ensure that beneficiaries have access to wheelchair accessories and seat and back cushions when furnished with Group 3 complex rehabilitative power wheelchairs. To ensure beneficiary access to these accessories particularly for these vulnerable populations, advance payment may be available for suppliers. Prior to July 1, suppliers will be paid the adjusted fee schedule rates. The average reduction during this period for these items is approximately 10%. During this time, CMS has announced that suppliers are able to submit a single advance payment request for multiple claims if the conditions described in CMS regulations at 42 CFR Section 421.214 are met. Additional information is below.
What is gap filling in Medicare?
For newly covered items of DMEPOS paid on a fee schedule basis where a Medicare fee does not exist , the Centers for Medicare & Medicaid Services (CMS) uses a process to establish fees called gap-filling. This allows Medicare to establish a price that aligns with the statutory requirements for the DMEPOS fee schedule.
What is a DMEPOS file?
The DMEPOS public use file contains fee schedules for certain items that were adjusted based on information from the DMEPOS Competitive Bidding Program in accordance with Section 1834 (a) (1) (F) of the Act.
What is TTFT in Medicare?
TTFT is a system consisting of an electromagnetic field generator and transducer arrays and will be covered under the Medicare Part B benefit for durable medical equipment (DME) for items and services furnished on or after September 1, 2019.
When does the Cares Act end?
Section 3712 (a) of the CARES Act extends the current adjusted fee schedule methodology that pays for certain items furnished in rural and non-contiguous non-CBAs based on a 50/50 blend of adjusted and unadjusted fee schedule amounts through December 31, 2020 or through the duration of the PHE, whichever is later.
What is assignment in Medicare?
Assignment —An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
Does Medicare pay for DME repairs?
Medicare will pay 80% of the Medicare-approved amount (up to the cost of replacing the item) for repairs. You pay the other 20%. Your costs may be higher if the supplier doesn’t accept assignment.
What is the CPM code for DME?
The CPM devices (HCPCS code E0935) are classified as items requiring frequent and substantial servicing and are covered as DME as follows (see the Medicare National Coverage Determinations Manual.):
How long do DME MACs pay rental fees?
For these items of DME, A/B MACs (HHH) and DME MACs pay the fee schedule amounts on a monthly rental basis not to exceed a period of continuous use of 15 months. In the tenth month of rental, the beneficiary is given a purchase option (see §30.5.2). If the purchase option is exercised, A/B MACs (HHH) and DME MACs continue to pay rental fees not to exceed a period of continuous use of 13 months and ownership of the equipment passes to the beneficiary. If the purchase option is not exercised, A/B MACs (HHH) and DME MACs continue to pay rental fees until the 15 month cap is reached and ownership of the equipment remains with the supplier (see §30.5.4). In the case of electric wheelchairs only, the beneficiary must be given a purchase option at the time the equipment is first provided (see §30.5.3).
How to determine liability to a provider other than an HHA?
To determine patient liability to a provider other than an HHA (including nominal charge providers other than a HHA), A/B MACs (A) subtract any unmet deductible from the actual charge and multiply the remainder by 20 percent. The result, plus the unmet deductible is the patient's liability. Coinsurance is applied as applicable.
How to determine Part B payment to nominal charge?
To determine the Part B payment to a nominal charge HHA , A/B MACs (HHH) subtract any unmet Part B deductible from the fee schedule amount and multiply the remainder by
How to determine Part B payment?
To determine the Part B payment to a provider other than nominal charge provider, A/B MACs (A) and (HHH) subtract any unmet Part B deductible from the lower of the actual charge or the fee schedule amount for the item or service and multiply the remainder by
What is an enteral care kit?
Enteral care kits contain all the necessary supplies for the enteral patient using the syringe, gravity, or pump method of nutrient administration. Parenteral nutrition care kits and their components are considered all-inclusive items necessary to administer therapy during a monthly period.
What is PIM in Medicare?
Chapter 5, section 5.2.1 of the Medicare Program Integrity Manual (PIM) states that, in order for Medicare to make payment for an item of Durable Medical Equipment Prosthetic, and Orthotic Supplies (DMEPOS), the DMEPOS supplier must obtain a prescription from the
Where to submit CMS-855S?
To do so, you’ll need to fill out and submit a CMS-855S form (along with all of your supporting documents) to Palmetto GBA, the national supplier clearinghouse for Medicare. If you have questions, you can contact the clearinghouse at 866-238-9652 or visit the Palmetto GBA website.
Is DME cut and dried?
Unfortunately, purchasing things such as splints, prosthetics, and durable medical equipment (DME) isn’t so cut and dried. In fact, when it comes to orthotics and prosthetics billing, there’s a lot of room for error. Prev.
When do hospitals report Medicare beneficiaries?
If the beneficiary is a dependent under his/her spouse's group health insurance and the spouse retired prior to the beneficiary's Medicare Part A entitlement date, hospitals report the beneficiary's Medicare entitlement date as his/her retirement date.
What is secondary payer?
Medicare is the Secondary Payer when Beneficiaries are: 1 Treated for a work-related injury or illness. Medicare may pay conditionally for services received for a work-related illness or injury in cases where payment from the state workers’ compensation (WC) insurance is not expected within 120 days. This conditional payment is subject to recovery by Medicare after a WC settlement has been reached. If WC denies a claim or a portion of a claim, the claim can be filed with Medicare for consideration of payment. 2 Treated for an illness or injury caused by an accident, and liability and/or no-fault insurance will cover the medical expenses as the primary payer. 3 Covered under their own employer’s or a spouse’s employer’s group health plan (GHP). 4 Disabled with coverage under a large group health plan (LGHP). 5 Afflicted with permanent kidney failure (End-Stage Renal Disease) and are within the 30-month coordination period. See ESRD link in the Related Links section below for more information. Note: For more information on when Medicare is the Secondary Payer, click the Medicare Secondary Payer link in the Related Links section below.
Does Medicare pay for black lung?
Federal Black Lung Benefits - Medicare does not pay for services covered under the Federal Black Lung Program. However, if a Medicare-eligible patient has an illness or injury not related to black lung, the patient may submit a claim to Medicare. For further information, contact the Federal Black Lung Program at 1-800-638-7072.
Does Medicare pay for the same services as the VA?
Veteran’s Administration (VA) Benefits - Medicare does not pay for the same services covered by VA benefits.
Is Medicare a primary or secondary payer?
Providers must determine if Medicare is the primary or secondary payer; therefore, the beneficiary must be queried about other possible coverage that may be primary to Medicare. Failure to maintain a system of identifying other payers is viewed as a violation of the provider agreement with Medicare.