Yes, you can have both Medicare and employer-provided health insurance. In most cases, you will become eligible for Medicare coverage when you turn 65, even if you are still working and enrolled in your employer’s health plan. You are welcome to drop the employer coverage and have only Medicare if you so choose, but you are not required to do so.
Full Answer
Should you stay on your employer health insurance or get Medicare?
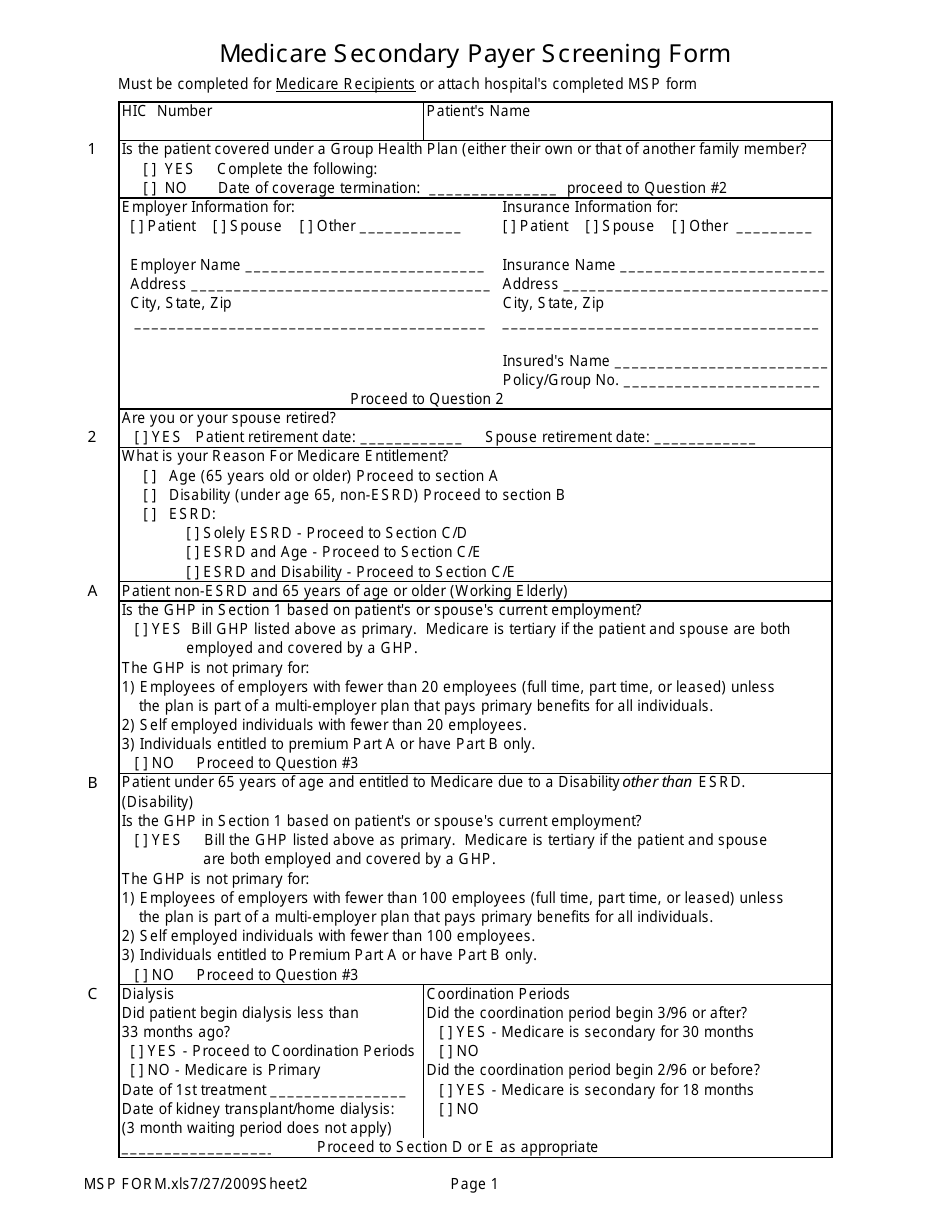
Depending on your employer’s size, Medicare will work with your employer’s health insurance coverage in different ways. If your company has 20 employees or less and you’re over 65, Medicare will pay primary. Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage a small group health plan.
How does Medicare work with employer insurance?
Nov 24, 2021 · Yes, you can have both Medicare and employer-provided health insurance. In most cases, you will become eligible for Medicare coverage when you turn 65, even if you are still working and enrolled in your employer’s health plan. You are welcome to drop the employer coverage and have only Medicare if you so choose, but you are not required to do so.
Can you get Medicare if you are still working?
Aug 14, 2021 · If your employer has fewer than 20 employees, Medicare becomes primary. Thus, your employer coverage pays second when you have both Medicare and coverage through an employer with fewer than 20 employees. If your employer has more than 20 employees, Medicare will pay secondary to your group coverage.
Does Medicare coverage change if you return to work?
May 07, 2021 · Although retirement age usually ranges from 66 to 67 years old, Medicare eligibility for most individuals begins at age 65. Some people who continue to work past age 65 may also have group health...
Can you have employer coverage and Medicare at the same time?
Do employers have to contribute to Medicare?
Is Medicare primary or secondary to group insurance?
Is Medicare financed by employer/employee contributions?
What is a Medicare eligible employee?
If an employer has fewer than 20 employees, an employee turning 65 and covered by the employer-based health insurance plan may be required to enroll in Medicare Part A and Part B. Medicare then becomes the primary payer of the employee's coverage.Jul 14, 2021
What happens when an employee turns 65?
How do you know if Medicare is primary or secondary?
How do you determine which insurance is primary and which is secondary?
Who is Medicare through?
Who pays for Medicare and who benefits?
What does Medicare employee mean on my paystub?
Who pays for Medicare Part A?
Can you keep Medicare and Cobra?
If you are first enrolled in Medicare and then become eligible for COBRA, you may keep both types of coverage . Medicare will serve as the primary payer, and COBRA will act as the secondary payer.
How long do you have to enroll in Medicare?
When your employer coverage does finally end, you will be given eight months to enroll in Medicare Part A and Part B, and you’ll have 63 days to enroll in a Medicare Advantage plan before facing any late enrollment penalties.
Is Medicare a primary or secondary payer?
Medicare acts as the secondary payer. Medicare categorizes a company of fewer than 20 employees as “small.”. If you are an active employee at a small company, Medicare will be the primary payer. Any employer coverage you receive will be the secondary payer.
How old do you have to be to be on Medicare?
Being under 65 years old with a disability. If you are under 65 but are enrolled in Medicare because of a disability and are also covered by an employer health plan, the employer will serve as the primary payer if it has more than 100 employees. With fewer than 100 employees, Medicare becomes the primary payer.
What is a large company?
Large companies (20 or more employees) A company is classified as “large” by Medicare if it has 20 or more employees. If you receive your employer health coverage from a large company and are still an active (not retired) employee, that coverage serves as the primary payer. Medicare acts as the secondary payer.
Is tricare a primary payer?
TRICARE. For active military members with TRICARE, TRICARE works as the primary payer, and Medicare is the secondary payer. Retired members of the military who receive TRICARE for Life are required to enroll in Medicare Part B if eligible, and Medicare will serve as their primary payer. Veterans Affairs (VA)
Who is Christian Worstell?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. .. Read full bio
Can employers contribute to Medicare premiums?
Medicare Premiums and Employer Contributions. Per CMS, it’s illegal for employers to contribute to Medica re premiums. The exception is employers who set up a 105 Reimbursement Plan for all employees. The reimbursement plan deducts money from the employees’ salaries to buy individual insurance policies.
Is Medicare billed first or second?
If your employer has fewer than 20 employees, then Medicare becomes primary. This means Medicare is billed first, and your employer plan will be billed second. If you have small group insurance, it’s HIGHLY recommended that you enroll in both Parts A and B as soon as you’re eligible. If you don’t, your employer’s group plan can refuse ...
What happens if you don't have Part B insurance?
If you don’t, your employer’s group plan can refuse to pay your claims. Your insurance might cover claims even if you don’t have Part B, but we always recommend enrolling in Part B. Your carrier can change that at any time, with no warning, leaving you responsible for outpatient costs.
Is Part B premium free?
Since Part B is not premium-free like Part A is for most, you may wish to delay enrollment if you have group insurance. As stated above, the size of your employer determines whether your coverage will be considered creditable once you retire and are ready to enroll. Group coverage for employers with 20 or more employees is deemed creditable ...
What is CMS L564?
You will need your employer to fill out the CMS-L564 form. This form is a request for employment information form. Once the employer completes section B of the form, you can send in the document with your application to enroll in Medicare.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare.
Does Medicare cover dependents?
Medicare is individual health insurance coverage, which means that it doesn’t include coverage for spouses or dependents. Most group health plans, on the other hand, do include some sort of coverage option for dependents and spouses.
How long do you have to enroll in Medicare after you retire?
Once you retire and give up your employer health benefits, you will have a special enrollment period of 8 months to enroll in Part A and Part B, if you haven’t enrolled already. This special enrollment period begins the month after your employment or group health plan ends. There is no late enrollment penalty for enrolling in original Medicare ...
How to determine if Medicare is primary or secondary?
Here’s how to know who the primary and secondary payers are in your situation: 1 Medicare is generally the primary payer if the company you work for has fewer than 20 employees. But Medicare becomes the secondary payer if your employer is part of a group health plan with other employers who have more than 20 employees. 2 Medicare is typically the secondary payer if the company you work for has 20 or more employees. In this case, your group health plan is the primary payer and Medicare pays out only after your employer’s plan has paid their portion.
How old do you have to be to get Medicare?
Although retirement age usually ranges from 66 to 67 years old, Medicare eligibility for most individuals begins at age 65. Some people who continue to work past age 65 may also have group health plan benefits through their employer. Because of this, it’s possible to have both Medicare and a group health plan after age 65.
Is Medicare the primary or secondary payer?
Medicare is typically the secondary payer if the company you work for has 20 or more employees.
What is the number to call Medicare?
If you’re not sure whether Medicare will be the primary or secondary payer in your situation, you can call 855-798-2627 to speak to someone at Medicare’s Benefits Coordination & Recovery Center.
What is the primary payer?
When you receive medical services, your primary insurance pays out first. This insurance is known as the primary payer. If there’s anything that your primary insurance didn’t cover, your secondary insurance pays out next. This insurance is known as the secondary payer.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is a health care provider?
Tell your doctor and other. health care provider. A person or organization that's licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers. about any changes in your insurance or coverage when you get care.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How many employees does a multi-employer plan have?
At least one or more of the other employers has 20 or more employees.
Does Medicare pay for Part A?
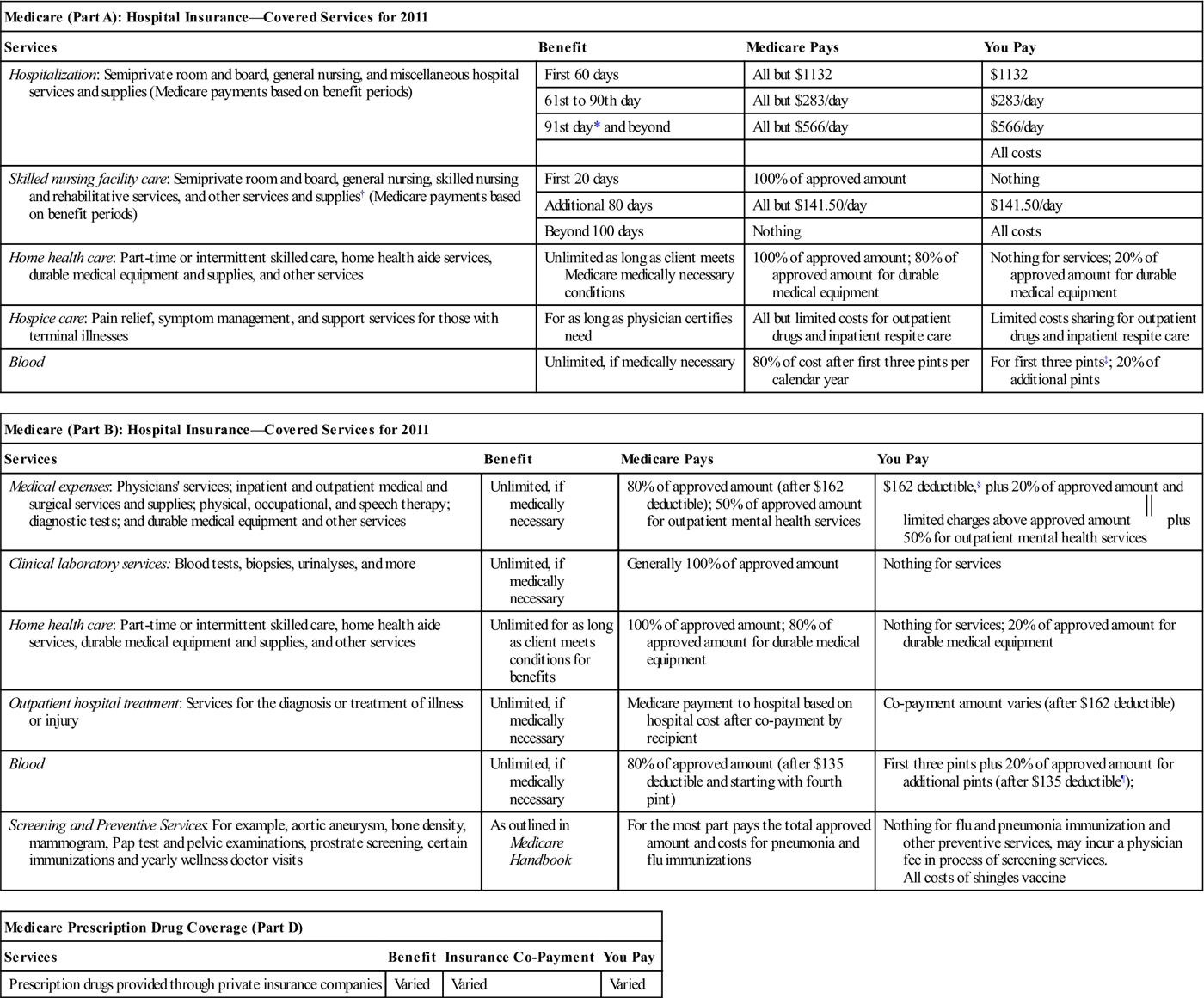
Medicare pays the rest of any Part A services. It doesn’t necessarily work the same way with Part B, and Part B costs money (see next section), so that’s why most people choose Part A only when working for a large employer. One exception would be if you are contributing to an HSA and plan to continue doing so.
When does Medicare change?
If that former employer DOES offer coverage, your benefits will likely change when you turn 65. This is because when you are age 65 and have retiree coverage, Medicare becomes your primary insurance, and your group coverage now pays secondary. Prices and benefits from your employer coverage may be different once you turn 65.
Do you have to have Medicare if you are 65?
Medicare and Employer Coverage. If you are 65+ (or turning 65 soon) and will have both Medicare and Employer Coverage because you are still actively working, you will have a number of things to think through. Medicare coordinates benefits with your employer coverage. You likely have options to keep your employer insurance ...
Is Medicare a secondary plan?
Medicare is secondary if you are age 65 or older and your employer has more than 20 employees and you are still ACTIVELY working (not a retiree or on COBRA). This is called Medicare Secondary Payer. In this scenario, your group plan pays first, and then Medicare pays second.
How much is Medicare Part A deductible in 2021?
The Medicare Part A hospital deductible is $1,484 in 2021. So if you have both your employer insurance and Part A, and you incur a bill for a hospital stay, you will only be out $1,484 for your inpatient hospital services. Medicare pays the rest of any Part A services.
Is Medicare Part B premium free?
Now Part B is not premium-free. You will pay a monthly premium for Part B based on your income. Some people who are eligible for Medicare and employer group health coverage choose to delay enrolling in Medicare Part B and Part D while still covered on their group health coverage (or their spouse’s group health coverage).
Is Medicare primary or secondary?
You will need both Part A & B for sure because Medicare will pay first, and then your group insurance will pay secondary. Occasionally we see some insurance companies who will cover claims even if you don’t have Part B. Don’t buy it. You run the risk of that insurance company changing that at any time without warning, and leaving you stuck with all the expenses that Part B would normally cover. It’s not worth the risk – we advise always enrolling in Parts A & B if your employer has fewer than 20 employees and Medicare will be primary.
When do you have to enroll in Medicare Part B?
If you work for a business with less than 20 people, your employer may require you to enroll in Medicare Part B at age 65. Talk to your employer to learn more about your options.
What can't an employer do?
What Your Employer Cannot Do 1 Your employer cannot require you to get on Medicare once you turn 65. 2 Your employer cannot require you to get on a different kind of insurance (like by offering to pay for you Medicare Supplement Insurance or Medicare Advantage Premiums, for example). 3 Your employer cannot offer you a different kind of insurance than people younger than you.
Do I need to sign up for Medicare when I turn 65?
It depends on how you get your health insurance now and the number of employees that are in the company where you (or your spouse) work.
How does Medicare work with my job-based health insurance?
Most people qualify to get Part A without paying a monthly premium. If you qualify, you can sign up for Part A coverage starting 3 months before you turn 65 and any time after you turn 65 — Part A coverage starts up to 6 months back from when you sign up or apply to get benefits from Social Security (or the Railroad Retirement Board).
Do I need to get Medicare drug coverage (Part D)?
You can get Medicare drug coverage once you sign up for either Part A or Part B. You can join a Medicare drug plan or Medicare Advantage Plan with drug coverage anytime while you have job-based health insurance, and up to 2 months after you lose that insurance.
How does Medicare reimbursement work?
A Medicare premium reimbursement is a fantastic way for active employees to get refunds of their premiums. Often, premiums may cost less than group insurance at your workplace. If you prefer Medicare to your group coverage, you may be eligible to get premium reimbursements.
What is a health reimbursement arrangement?
A Health Reimbursement Arrangement is a system covered by Section 105. This arrangement allows your employer to reimburse you for your premiums. Some HRAs at employers that provide group coverage require that your employer’s payment plan ties in with the group health plan. Contact a human resources representative at your organization ...
What is Section 105?
Although there are several different plan options, the most popular Section 105 program is a Health Reimbursement Arrangement plan.
What is a Section 105 health plan?
The type of Section 105 plans employers offers will depend on the employer’s size and whether they provide a group health plan. A Health Reimbursement Arrangement is a system covered by Section 105. This arrangement allows your employer to reimburse you for your premiums. Some HRAs at employers that provide group coverage require ...
What is ICHRA insurance?
Individual Coverage Health Reimbursement Arrangement (ICHRA) To be eligible for an Individual Coverage Health Reimbursement Arrangement, you’ll need Part A and Part B, or Part C. You can use the ICHRA to reimburse premiums for Medicare and Medigap as well as other costs. Employers have more choice in which medical costs are eligible ...
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare.
