If your or your spouse's employer has less than 20 employees and isn't part of a multi-employer or multiple employer group health plan, then Medicare pays first, and the group health plan pays second. Medicare pays first. Medicare may pay second if both of these apply: At least one or more of the other employers has 20 or more employees.
Full Answer
Is Medicare better than employer insurance?
Their spouse can stay on their employer’s plan until they become eligible for Medicare, and though there are some exceptions, 65-year-old employees can benefit from both their employer’s plan and their Medicare plan. Contrary to popular belief, Medicare could actually provide better coverage at a lower cost than an employer plan.
Do you need Medicare if you have employer coverage?
Individuals age 65 and over who currently receive group health plan coverage from their employers are also eligible for Medicare. Depending on the size of the company, these individuals may choose to enroll into Medicare immediately or delay enrollment until a later date.
Can I still work and get Medicare coverage?
You can join a Medicare drug plan or Medicare Advantage Plan with drug coverage anytime while you have job-based health insurance, and up to 2 months after you lose that insurance. A period of time when you can join or leave a Medicare-approved plan.
Can I get Medicare through my spouse?
You’re generally eligible for Original Medicare (Part A and Part B) when you turn 65 or receive disability benefits, whether or not you’re married. If you’re married and haven’t worked in a paying job or didn’t work enough quarters, you may still qualify for premium-free Medicare Part A benefits through your spouse.

Can my spouse get Medicare if I am still working?
Generally, if you have job-based health insurance through your (or your spouse's) current job, you don't have to sign up for Medicare while you (or your spouse) are still working. You can wait to sign up until you (or your spouse) stop working or you lose your health insurance (whichever comes first).
Can one spouse be on Medicare and the other not?
The answer is no. Medicare is individual insurance, so spouses cannot be on the same Medicare plan together. Now, if your spouse is eligible for Medicare, then he or she can get their own Medicare plan.
Is my spouse eligible for Medicare when I turn 65?
Your spouse is eligible for Medicare when he or she turns 65. Your eligibility for Medicare has no impact on the date that your spouse is eligible for Medicare. Continue reading for more answers to your questions about Medicare, individual health insurance, and coverage options for your spouse after you enroll.
Can you have Medicare and employer insurance at the same time?
Yes, you can have both Medicare and employer-provided health insurance. In most cases, you will become eligible for Medicare coverage when you turn 65, even if you are still working and enrolled in your employer's health plan.
How does Medicare work for married couples?
Medicare has no family plans, meaning that you and your spouse must enroll for Medicare benefits separately. This also means husbands, wives, spouses and partners pay separate Medicare premiums.
When can my wife get Medicare?
age 65 or olderTo qualify for Medicare, your spouse must be age 65 or older. If your spouse is age 62 (or any age under 65), he or she could only qualify for Medicare by disability.
Can my wife get Medicare when I retire?
Your Medicare insurance doesn't cover your spouse – no matter whether your spouse is 62, 65, or any age. But in some cases, a younger spouse can help you get Medicare Part A with no monthly premium.
Can I drop my employer health insurance and go on Medicare?
You can keep your employer plan and sign up for Medicare Part A. You can keep your employer plan and sign up for Medicare Part A, and decide if you want to pick up B, D, and/or a Medigap Plan. Most people don't sign up for Parts B and D, because they have a monthly premium.
Does my spouse have to pay for Medicare?
Most people pay the standard premium, which is $148 per month in 2021. The more you make each year, the more you'll pay each month for Medicare. For Part C (Medicare Advantage), you and your spouse will have your own premium, deductible, and copays. This is true even if you have the same plan.
Do I automatically get Medicare when I turn 65?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
Is Medicare always the primary payer?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
How do you determine which insurance is primary and which is secondary?
The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" to pay. The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer.
When do spouses have to enroll in Medicare?
Check whether your spouse’s employer plan requires you, as a covered dependent, to enroll in Medicare when you turn 65. Some plans — notably the military’s TriCare-for-Life coverage and health benefits provided by an employer with fewer than 20 employees — automatically become secondary to Medicare when an enrollee becomes entitled to Medicare.
How long does a spouse have to sign up for a new employer?
This period lasts for up to eight months after employer coverage comes to an end.
How long after Medicare Part B enrollment can I buy a Medigap policy?
In addition, during the six months following Part B enrollment, you have a guaranteed right to buy a Medigap policy, also known as Medicare Supplement Insurance. After six months , Medigap providers can deny to sell you a plan, or can alter your premiums, based on preexisting conditions.
What happens if you don't have Medicare?
In this case, if you’re not enrolled in Medicare, you would receive almost no coverage from the employer plan. If you are not married but living in a domestic partnership and you are covered by your partner's health insurance at work, you should enroll in Part A and Part B during your initial enrollment period at age 65 to avoid late penalties. ...
When can I enroll in Medicare Part A?
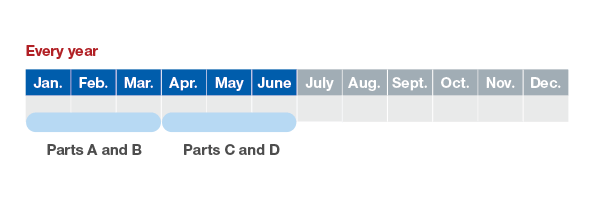
You can enroll in Part A (hospital insurance) during your seven-month initial enrollment period around your 65th birthday. It won’t cost you anything — there are no premiums for Part A if you’re entitled to Medicare — but it provides an opportunity to tell the Social Security Administration (SSA), which handles Medicare enrollment, ...
Do I have to sign up for Medicare if I'm 65?
No, as long as you follow Medicare’s rules. Almost anybody who is retired but has group health coverage from the employer of a spouse who is still working does not need to sign up for Medicare Part B on reaching 65.
Do I need to sign up for Part D if my spouse is still working?
As long as you continue to receive “creditable” drug coverage under the employer plan — whether your spouse is still working or retired — you do not need to sign up for a Part D plan. Creditable coverage means that Medicare considers it to be as good as Part D.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What happens when there is more than one payer?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) to pay. In some rare cases, there may also be a third payer.
Delaying Medicare Coverage
You do have the option to delay your enrollment for Medicare if another health insurance plan already covers you.
Enrolling in Medicare
If you do not want to delay your Medicare enrollment process, you can still enroll in Original Medicare, a Medicare Advantage Plan, or a Medicare Part D prescription drug plan. You will need to enroll during your Initial Enrollment Period, which begins three months before your 65th birthday and ends three months after your 65th birthday.
Should I enroll in Medicare?
Enrolling in Medicare when you already have health coverage is not necessary, but if you don’t want to delay your enrollment, then you should familiarize yourself with the enrollment periods to avoid possible penalties.
How long do you have to work to qualify for Medicare?
In the United States, as soon as you turn 65 you are eligible for Medicare benefits if you are citizen or have been a legal resident for five years or more and have worked for at least 40 quarters (10 years) paying federal taxes.
How old do you have to be to get Medicare?
In a case such as this, you must be at least 62 years old.
Can you get Medicare at different ages?
If you and your spouse are different ages, you will likely become eligible at different times. Primary Medicare recipients and their non-insured spouses are entitled to the same benefits under Medicare if both have reached the age of 65.
Do you have to enroll in Medicare Part B or D?
If you wish to sign up for Medicare Part B (Medical Insurance), and/or Part D (prescription drug insurance), you must enroll separately during your initial enrollment period, Open Enrollment or during Special Enrollment Period to avoid paying late enrollment penalties.
How long does Medicare coverage last?
This special period lasts for eight months after the first month you go without your employer’s health insurance. Many people avoid having a coverage gap by signing up for Medicare the month before your employer’s health insurance coverage ends.
What is a small group health plan?
Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage a small group health plan. If your employer’s insurance covers more than 20 employees, Medicare will pay secondary and call your work-related coverage a Group Health Plan (GHP).
Does Medicare pay second to employer?
Your health insurance through your employer will pay second and cover either some or all of the costs left over. If Medicare pays secondary to your insurance through your employer, your employer’s insurance pays first. Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance ...
Does Medicare cover health insurance?
Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance coverage in different ways. If your company has 20 employees or less and you’re over 65, Medicare will pay primary. Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage ...
Can an employer refuse to pay Medicare?
The first problem is that your employer can legally refuse to make any health-related medical payments until Medicare pays first. If you delay coverage and your employer’s health insurance pays primary when it was supposed to be secondary and pick up any leftover costs, it could recoup payments.
How long do you have to work to get Medicare?
Generally, you qualify for premium-free Part A when you’ve worked at least 10 years (40 quarters) paying Medicare taxes. Beneficiaries typically pay a Part B premium.
How old do you have to be to get Medicare?
If your spouse is at least 62 years old, and has worked at least 10 years paying Medicare taxes, you can enroll in Medicare when you turn 65, including premium-free Part A. If your spouse is younger than 62 when you turn 65, you won’t qualify for premium-free Part A until your spouse turns 62 ...
Do you have to pay Medicare premiums if you haven't worked?
Beneficiaries typically pay a Part B premium. If you haven’t worked and paid taxes for that long, you may have to pay a monthly premium for Medicare Part A, depending on your spouse’s age and how long he or she has worked and paid taxes. If you’re married and haven’t worked in a paying job:
How to choose between Medicare and employer coverage?
Choosing between Medicare and employer coverage. If you are eligible for both Medicare and employer coverage, you will generally have three options: Keep both types of coverage. Drop your employer coverage and just have Medicare. Delay Medicare enrollment and just have employer coverage.
How long do you have to enroll in Medicare?
When your employer coverage does finally end, you will be given eight months to enroll in Medicare Part A and Part B, and you’ll have 63 days to enroll in a Medicare Advantage plan before facing any late enrollment penalties.
How old do you have to be to be on Medicare?
Being under 65 years old with a disability. If you are under 65 but are enrolled in Medicare because of a disability and are also covered by an employer health plan, the employer will serve as the primary payer if it has more than 100 employees. With fewer than 100 employees, Medicare becomes the primary payer.
What is Medicare payer?
When enrolled in both Medicare and employer insurance, each type of coverage is called a “ payer .”. Which type of coverage pays first depends largely on the size of your employer.
Is Medicare a primary or secondary payer?
Medicare acts as the secondary payer. Medicare categorizes a company of fewer than 20 employees as “small.”. If you are an active employee at a small company, Medicare will be the primary payer. Any employer coverage you receive will be the secondary payer.
Can you keep Medicare and Cobra?
If you are first enrolled in Medicare and then become eligible for COBRA, you may keep both types of coverage . Medicare will serve as the primary payer, and COBRA will act as the secondary payer.
Do I need to sign up for Medicare when I turn 65?
It depends on how you get your health insurance now and the number of employees that are in the company where you (or your spouse) work.
How does Medicare work with my job-based health insurance?
Most people qualify to get Part A without paying a monthly premium. If you qualify, you can sign up for Part A coverage starting 3 months before you turn 65 and any time after you turn 65 — Part A coverage starts up to 6 months back from when you sign up or apply to get benefits from Social Security (or the Railroad Retirement Board).
Do I need to get Medicare drug coverage (Part D)?
You can get Medicare drug coverage once you sign up for either Part A or Part B. You can join a Medicare drug plan or Medicare Advantage Plan with drug coverage anytime while you have job-based health insurance, and up to 2 months after you lose that insurance.