Part A ($195.4 billion gross fee‑for‑service spending in 2016): Medicare Part A pays for inpatient hospital, skilled nursing facility, home health related to a hospital stay, and hospice care. Part A financing comes primarily from a 2.9 percent payroll tax paid by both employees and employers.
Full Answer
How much does Medicare Part a cost in 2016?
About 99 percent of Medicare beneficiaries do not pay a Part A premium since they have at least 40 quarters of Medicare-covered employment. The Medicare Part A annual deductible that beneficiaries pay when admitted to the hospital will be $1,288.00 in 2016, a small increase from $1,260.00 in 2015.
Will Medicare premiums and deductibles increase in 2016?
Today, the Centers for Medicare & Medicaid Services (CMS) announced the 2016 premiums and deductibles for the Medicare inpatient hospital (Part A) and physician and outpatient hospital services (Part B) programs. As the Social Security Administration previously announced, there will no Social Security cost of living increase for 2016.
How many Americans are enrolled in Medicare Part B in 2016?
These groups account for about 30 percent of the 52 million Americans expected to be enrolled in Medicare Part B in 2016. “Our goal is to keep Medicare Part B premiums affordable.
Is Medicare a primary or secondary payer?
Mostly, Medicare is primary. The primary insurer is the one that pays the claim first, whereas the secondary insurer pays second. With a Medigap policy, the supplement is secondary. Medicare pays claims first, and then Medigap pays. But, depending on the other policy, you have Medicare could be a secondary payer.

Who pays the 20% of a Medicare B claim?
After the beneficiary meets the annual deductible, Part B will pay 80% of the “reasonable charge” for covered services, the reimbursement rate determined by Medicare; the beneficiary is responsible for the remaining 20% as “co-insurance.” Unfortunately, the “reasonable charge” is often less than the provider's actual ...
What is the percentage of beneficiaries that are in the original Medicare plan?
Currently, 44 million beneficiaries—some 15 percent of the U.S. population—are enrolled in the Medicare program. Enrollment is expected to rise to 79 million by 2030. Only one in 10 beneficiaries relies solely on the Medicare program for health care coverage.
What covers the 20% on Medicare?
For Part B-covered services, you usually pay 20% of the Medicare-approved amount after you meet your deductible. This is called your coinsurance. You pay a premium (monthly payment) for Part B. If you choose to join a Medicare drug plan, you'll pay a separate premium for your Medicare drug coverage (Part D).
How much did Medicare go up in 2016?
Some people already signed up for Part B could see a hike in premiums.How Much You'll Pay for Medicare Part B in 2016Single Filer IncomeJoint Filer Income2016 Monthly PremiumUp to $85,000Up to $170,000$121.80 or $104.90*$85,001 - $107,000$170,001 - $214,000$170.50$107,001 - $160,000$214,001 - $320,000$243.602 more rows
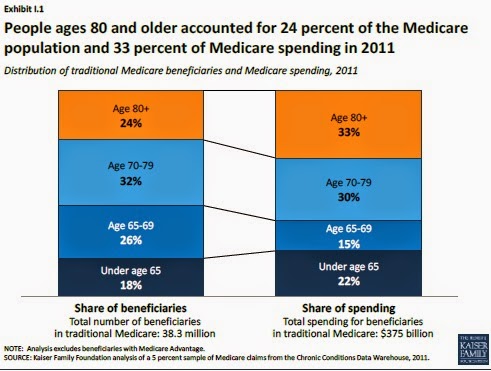
Who uses the most Medicare?
The majority (83%) of Medicare beneficiaries are ages 65 and older, while 17 percent are under age 65 and qualify for Medicare because of a permanent disability. However, a much larger share of black (31%) and Hispanic beneficiaries (23%) than white beneficiaries (14%) are under age 65 and living with disabilities.
What percent of Medicare is Medicare Advantage?
In 2021, more than 26 million people are enrolled in a Medicare Advantage plan, accounting for 42 percent of the total Medicare population, and $343 billion (or 46%) of total federal Medicare spending (net of premiums).
Does everyone pay the same for Medicare Part B?
Medicare premiums are calculated based on your modified adjusted gross income from two years prior. Thus, your premium can change if you receive a change in income. Does everyone pay the same for Medicare Part B? No, each beneficiary will pay a Medicare Part B premium that is based on their income.
Who pays for Medicare Part A?
Most people receive Medicare Part A automatically when they turn age 65 and pay no monthly premiums. If you or your spouse haven't worked at least 40 quarters, you'll pay a monthly premium for Part A.
Why is my first Medicare bill so high?
If you're late signing up for Original Medicare (Medicare Parts A and B) and/or Medicare Part D, you may owe late enrollment penalties. This amount is added to your Medicare Premium Bill and may be why your first Medicare bill was higher than you expected.
When did Medicare start charging a premium?
July 30, 1965July 30, 1965: With former President Harry S. Truman at his side, President Lyndon B. Johnson signs the Medicare bill into law.
What were Medicare Part B premiums in 2016?
If you were enrolled in Medicare Part B prior to 2016, your 2016 monthly premium is generally $104.90.
Are Medicare premiums adjusted for inflation?
Medicare Part B premiums are indexed for inflation. They're adjusted periodically to keep pace with the falling value of the dollar. What you pay this year may not be what you'll pay next year.
What is the number to call for Medicare?
If you have questions about who pays first, or if your coverage changes, call the Benefits Coordination & Recovery Center (BCRC) toll-free at 1-855-798-2627. TTY users should call 1-855-797-2627. To better serve you, have your Medicare number ready when you call.
What is Medicare and other health insurance called?
If you have Medicare and other health coverage, each type of coverage is called a “payer.”. When there’s more than one payer, “coordination of benefits” rules decide who pays first. The “primary payer” pays what it owes on your bills first, and then your provider sends the rest to the “secondary payer” to pay. ...
Is there a third payer for Medicare?
In some cases, there may also be a “third payer.”. Whether Medicare pays first depends on a number of things. Be sure to tell your doctor and other health care providers if you have health coverage in addition to Medicare. This will help them send your bills to the correct payer to avoid delays.
How much did PDP premiums increase in 2016?
After several years of relatively low growth, average monthly PDP premiums increased by 6 percent in 2016 to $39.21 per month. However, monthly premiums for two of the most popular PDPs (AARP Rx Preferred and Humana Enhanced) increased by more than 20 percent in 2016.
What is Medicare Part D?
The law that established Part D defined a standard drug benefit , but nearly all Part D plan sponsors offer plans with alternative designs ...
How many cost sharing tiers are there in Part D?
Almost all Part D enrollees are in plans with five cost-sharing tiers: two generic tiers, two brand tiers, and a specialty tier. PDPs typically charge coinsurance rather than copayments for brand-name drugs, and the use of tiered pharmacy networks is now the norm in PDPs.
How many people are in enhanced plans for Part D?
More than half of Part D enrollees are in enhanced plans. Nearly three in 10 Part D enrollees (29 percent, or about 12 million enrollees) are receiving extra help through the Part D Low-Income Subsidy (LIS) program that pays their drug plan premiums (if they enroll in a benchmark plan) and reduces their cost sharing.
Does Medicare have a drug plan?
Since 2006, Medicare beneficiaries have had access to prescription drug coverage offered by private plans, either stand-alone prescription drug plans (PDPs) or Medicare Advantage drug plans (MA-PD plans). Medicare drug plans (also referred to as Part D plans) receive payments from the government to provide Medicare-subsidized drug coverage to enrolled beneficiaries, who pay a monthly premium that varies by plan. The law that established Part D defined a standard drug benefit, but nearly all Part D plan sponsors offer plans with alternative designs that are equal in value, and plans may also offer an enhanced benefit. Part D plans also must meet certain other requirements, but vary in terms of premiums, benefit design, gap coverage, formularies, and pharmacy networks.
How much money did Medicare spend in 2016?
In FY 2016, the Office of the Actuary has estimated that gross current law spending on Medicare benefits will total $672.6 billion. Medicare will provide health insurance to 57 million individuals who are 65 or older, disabled, or have end-stage renal disease.
What is the Medicare budget for 2016?
The FY 2016 Budget includes a package of Medicare legislative proposals that will save a net $423.1 billion over 10 years. The proposals are scored off the President’s Budget adjusted baseline, which assumes a zero percent update to Medicare physician payments. These reforms will strengthen Medicare by more closely aligning payments with the costs of providing care, encouraging health care providers to deliver better care and better outcomes for their patients, and improving access to care for beneficiaries. The Budget includes investments to reform Medicare physician payments and accelerate physician participation in high-quality and efficient healthcare delivery systems. Finally, it makes structural changes in program financing that will reduce Federal subsidies to high income beneficiaries and create incentives for beneficiaries to seek high value services. Together, these measures will extend the Hospital Insurance Trust Fund solvency by approximately five years.
What is a Part D beneficiary?
2/ In Part D only, some beneficiary premiums are paid directly to plans and are netted out here because those payments are not paid out of the Trust Funds. 3/ Includes related benefit payments, including refundable payments made to providers and plans, transfers to Medicaid, and additional Medicare Advantage benefits.
What is the authority for a program to prevent prescription drug abuse in Medicare Part D?
Establish Authority for a Program to Prevent Prescription Drug Abuse in Medicare Part D: HHS requires Part D sponsors to conduct drug utilization review, which assesses the prescriptions filled by a particular enrollee.
How many people are in Medicare Part D in 2016?
In 2016, the number of beneficiaries enrolled in Medicare Part D is expected to increase by about 3.5 percent to 43.7 million , including about 12.6 million beneficiaries who receive the low‑income subsidy.
How much has Medicare saved?
Cumulatively since enactment of the Affordable Care Act, 9.4 million beneficiaries have saved a total of $15 billion on prescription drugs. The FY 2016 Budget includes a package of Medicare legislative proposals that will save a net $423.1 billion over 10 years.
What are the goals of CMS for FY 2016?
Clinical Quality Improvement: The key goals for FY 2016 are improving the health status of communities; delivering patient-centered, reliable, accessible, and safe care; and better care at lower costs. Through improving cardiac health, reducing disparities in diabetic care, using immunization information systems and meaningful use of health IT to improve prevention coordination, CMS aims to improve the health status ofbeneficiaries. These goals will also be achieved by efforts to reduce healthcare‑associated infections, healthcare‑associated conditions in nursing homes, and hospital readmissions and adverse drug events.
How many people did Medicare cover in 2017?
programs offered by each state. In 2017, Medicare covered over 58 million people. Total expenditures in 2017 were $705.9 billion. This money comes from the Medicare Trust Funds.
What is Medicare Part B?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. and. Medicare Drug Coverage (Part D) Optional benefits for prescription drugs available to all people with Medicare for an additional charge.
What is the CMS?
The Centers for Medicare & Medicaid Services ( CMS) is the federal agency that runs the Medicare Program. CMS is a branch of the. Department Of Health And Human Services (Hhs) The federal agency that oversees CMS, which administers programs for protecting the health of all Americans, including Medicare, the Marketplace, Medicaid, ...
Who pays payroll taxes?
Payroll taxes paid by most employees, employers, and people who are self-employed. Other sources, like these: Income taxes paid on Social Security benefits. Interest earned on the trust fund investments. Medicare Part A premiums from people who aren't eligible for premium-free Part A.
Does Medicare cover home health?
Medicare only covers home health care on a limited basis as ordered by your doctor. , and. hospice. A special way of caring for people who are terminally ill. Hospice care involves a team-oriented approach that addresses the medical, physical, social, emotional, and spiritual needs of the patient.
How to learn more about Medicare?
How to Learn More About Your Medicare Options. Primary insurance isn't too hard to understand; it's just knowing which insurance pays the claim first. Medical billing personnel can always help you figure it out if you're having trouble. While it's not hard to understand primary insurance, Medicare is its own beast.
Is Medicare primary insurance in 2021?
Updated on July 13, 2021. Many beneficiaries wonder if Medicare is primary insurance. But, the answer depends on several factors. While there are times when Medicare becomes secondary insurance, for the most part, it’s primary. Let’s go into further detail about what “primary” means, and when it applies.
Is Medicare a primary or secondary insurance?
Mostly, Medicare is primary. The primary insurer is the one that pays the claim first, whereas the secondary insurer pays second. With a Medigap policy, the supplement is secondary. Medicare pays claims first, and then Medigap pays. But, depending on the other policy, you have Medicare could be a secondary payer.
Does Medicare pay your claims?
Since the Advantage company pays the claims, that plan is primary. Please note that Medicare WON’T pay your claims when you have an Advantage plan. Medicare doesn’t become secondary to an Advantage plan. So, you’ll rely on the Advantage plan for claim approvals.
Can you use Medicare at a VA hospital?
Medicare and Veterans benefits don’t work together; both are primary. When you go to a VA hospital, Veteran benefits are primary. Then, if you go to a civilian doctor or hospital, Medicare is primary. But, you CAN’T use Veterans benefits at a civilian doctor. Also, you can’t use Medicare benefits at the VA.
Is Medicare a part of tricare?
Medicare is primary to TRICARE. If you have Part A, you need Part B to remain eligible for TRICARE. But, Part D isn’t a requirement. Also, TRICARE covers your prescriptions. Your TRICARE will be similar to a Medigap plan; it covers deductibles and coinsurances.