What does the Medicare permission to contact rule cover?
What Does it Cover? Specifically, the Medicare Permission to Contact (PTC) rule outlines when it is okay to contact a current or potential Medicare beneficiary, the specific products they are giving you permission to contact them for, how you can approach them, and when you can contact them.
How long does it take to get prior authorization for Medicare?
Once approved, your plan pays without prior authorization. How Long Does it Take to Get Prior Authorization? It can take days to get prior authorization. Although, if you’re waiting for a drug, you should call your local pharmacy within a week.
Can I contact Medicare enrollees via email?
Due to a change reflected in the 2019 MCMG and now in the Medicare Advantage & Part D Communication Requirements, agents are permitted to make unsolicited direct contact with potential enrollees via email. However, the email must have an opt-out option in order to remain compliant.
Can a client contact Medicare supplements or Medicare Advantage?
A client should indicate whether they want information on Medicare Supplements, Medicare Advantage, or both. Once a beneficiary gives permission for an agent to contact them, the agent still has to be careful. The permission only covers a very small window of service.
What is the permission to contact form?
The Medicare Permission to contact form (goes by acronym PTC) is different than a scope of appointment. A PTC form allows you to contact the prospect via phone or in person. Cold calling prospects for Medicare Advantage and Medicare part D plans is a violation of CMS rules.
Can you email a Medicare beneficiary?
Due to a change reflected in the 2019 MCMG and now in the Medicare Advantage & Part D Communication Requirements, agents are permitted to make unsolicited direct contact with potential enrollees via email. However, the email must have an opt-out option in order to remain compliant.
What are the unsolicited contact rules for Medicare?
CMS has strict guidelines around contacting Medicare beneficiaries. In general, you can't market through unsolicited direct contact. (Often referred to as cold calling and includes going door-to-door.) Referred beneficiaries must contact you or the plan directly.
Can I speak to Medicare on behalf of someone else?
You can either give verbal permission over the phone for the customer service representative to speak with someone else on your behalf, or fill out an authorization form in advance.
When can telephonic contact with a Medicare eligible consumer be made quizlet?
Once contact is made or 9 months from the date the consumer provided permission (e.g. consumer signature date on BRC) or 90 days if on federal do not call list, whichever comes first. Agent Brenda is presenting Medicare Advantage plan options to her consumer, Melanie.
Which of the following describes permission to contact guidelines quizlet?
Which of the following describes Permission to Contact guidelines? It allows the agent to discuss the products identified during the marketing appointment. It does not have to be provided by the consumer, but can be provided by the consumer's spouse or adult child.
When can telephonic contact with a Medicare consumer be made?
Once contact is made or 9 months from the date the consumer provided permission (e.g. consumer signature date on BRC) or 90 days if on federal do not call list, whichever comes first.
What is Medicare solicitation?
People representing Medicare plans aren't allowed to: Come to your home uninvited to sell or endorse anything. Call you unless you're already a member of the plan. If you're a member, the agent who helped you join can call you.
What are CMS guidelines for referrals?
In a CMS compliant situation, you would 1) ask for referrals without mentioning any benefit to the enrollee and then 2) present a thank-you gift for the referrals he or she has provided. Second, the gifts you provide must be of a nominal value.
How does Medicare Helpline work?
The Medicare Coverage Hotline is a private for-profit lead generation campaign and does not offer insurance and is not an insurance agency or broker. Your call is sold to a licensed insurance agent to give you information about your Medicare Advantage Plans.
Who is the best person to talk to about Medicare?
You can make an appointment with a Social Security representative at your local office by calling 1-800-772-1213. You can also call Medicare directly at 1-800-633-4227. Finally, your State Health Insurance Assistance Program (SHIP) provides free counseling and education to help you choose coverage.
Can you call Medicare 24 hours a day?
Medicare offers a toll-free number that's staffed 24 hours a day, seven days a week. Beneficiaries can call for Medicare information or to enroll in a plan or make an appeal. Callers can choose from a handful of menu options. Beneficiaries can also mail or fax Medicare or request information in an accessible format.
Why would I get a letter from CMS?
In general, CMS issues the demand letter directly to: The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment.
Why do I keep getting emails about Medicare?
Ads or mailings from Medicare health plans typically start on or just after October 1 each year. These marketing campaigns are designed to prompt you to call a phone number, enter an email address, or register for an event to learn more about an advertised plan and ultimately sign up for that plan.
Why do I get Medicare mail?
It's sent to all people who automatically get Medicare because they're getting Social Security benefits before they're eligible for Medicare. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
Why am I getting a letter from Medicare?
If Medicare enrolls you in a plan, you'll get a yellow or green letter letting you know when your coverage begins, and you'll have a Special Enrollment Period to change plans if you want to enroll in a different plan than the one Medicare enrolled you in.
Phone
For specific billing questions and questions about your claims, medical records, or expenses, log into your secure Medicare account, or call us at 1-800-MEDICARE.
1-800-MEDICARE (1-800-633-4227)
For specific billing questions and questions about your claims, medical records, or expenses, log into your secure Medicare account, or call us at 1-800-MEDICARE.
What happens if your client requests Medicare information outside of the scope during your meeting?
What happens if your client requests Medicare information outside of the Scope during your meeting? You must fill out a second Scope covering the new information before continuing the meeting. If they’re interested in non-health related products, you must schedule a future appointment to discuss them.
How long do you have to keep SOA for Medicare?
Per CMS, agents must keep SOA forms on file for at least 10 years, even if the appointment didn’t end in a sale.
How to mention star rating in Medicare?
When mentioning Star Ratings, you must include that the rating is out of five stars and clearly identify the star ratings’ contract year. You may not reference the Star Rating based on prior contract year data when the marketing materials are for the upcoming year. Agents must also let potential enrollees know when a plan has been assigned an LPI or Low Performing Icon by CMS. You may not showcase the overall Star Rating and fail to disclose that the plan has previously suffered from performance issues. Additionally, Star Ratings may not be published until CMS releases them on the Medicare Plan Finder.
What does CMS regulate?
CMS also regulates marketing and plan presentations, including when you’re allowed to market, and how you market.
What is life as an agent before Medicare?
Life as an agent before Medicare’s Annual Enrollment Period is a flurry of contracting and certifying. But there’s another C that’s even more important: Compliance.
Is permission to contact the same as scope of appointment?
Permission to Contact is not the same as Scope of Appointment. Mostly, PTC comes first, then SOA next.
Can an agent contact potential clients via email?
Due to a change reflected in the 2019 Medicare Communications and Marketing Guidelines (MCMG) and now updated in CFR 42, agents are permitted to make unsolicited direct contact with potential enrollees via email. However, the email must have an opt-out option in order to remain compliant. Additionally, the content of any unsolicited email cannot intend to steer a recipient into choosing or retaining a plan. A compliant email would promote your services rather than any specific plans.
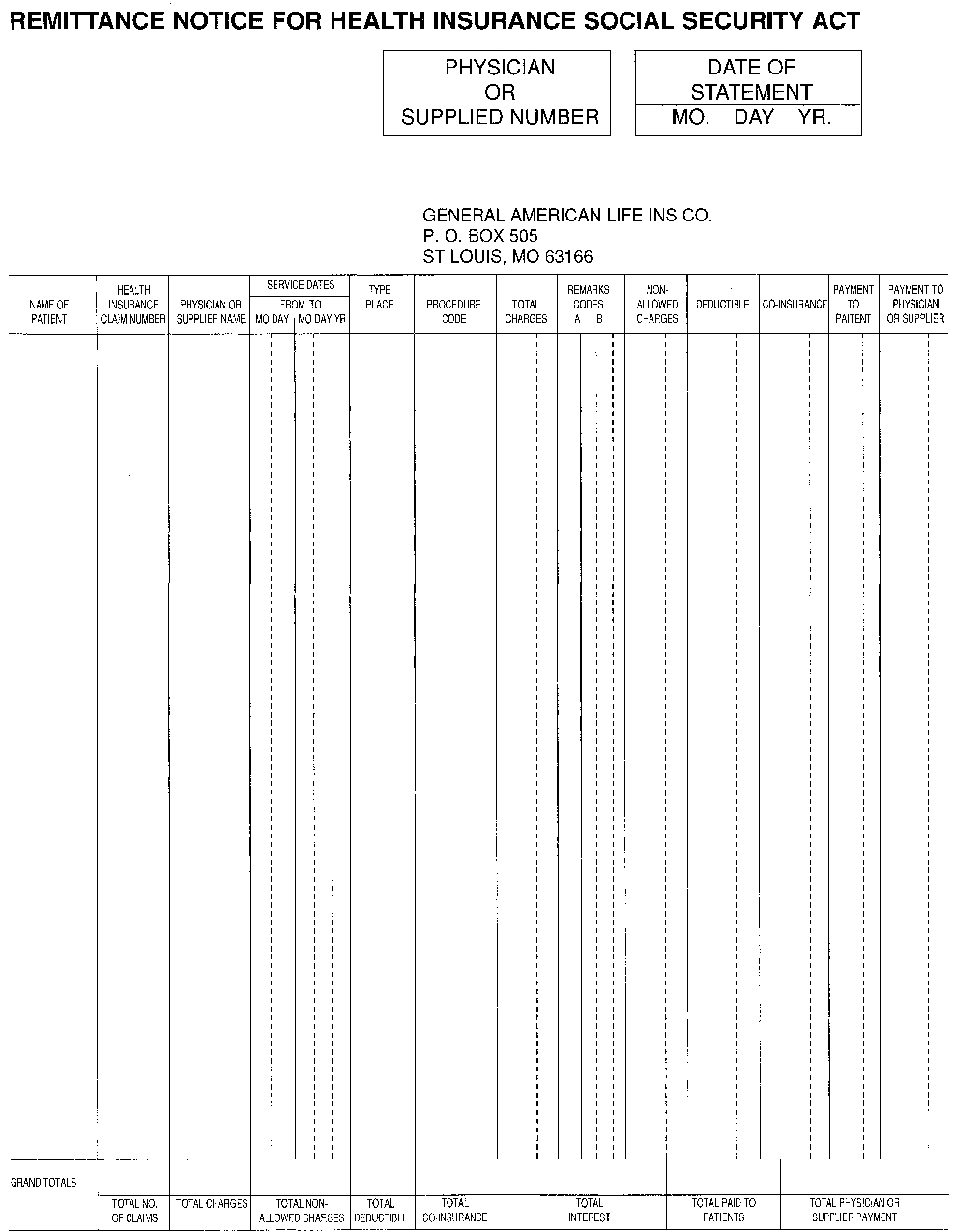
How to release information from Medicare?
Medicare does not release information from a beneficiary’s records without appropriate authorization. If you have an attorney or other representative , he or she must send the BCRC documentation that authorizes them to release information. Your attorney or other representative will receive a copy of the RAR letter and other letters from the BCRC as long as he or she has submitted a Consent to Release form. A Consent to Release (CTR) authorizes an individual or entity to receive certain information from the BCRC for a limited period of time. With that form on file, your attorney or other representative will also be sent a copy of the Conditional Payment Letter (CPL) and demand letter. If your attorney or other representative wants to enter into additional discussions with any of Medicare’s entities, you will need to submit a Proof of Representation document. A Proof of Representation (POR) authorizes an individual or entity (including an attorney) to act on your behalf. Note: In some special circumstances, the potential third-party payer can submit Proof of Representation giving the third-party payer permission to enter into discussions with Medicare’s entities. If potential third-party payers submit a Consent to Release form, executed by the beneficiary, they too will receive CPLs and the demand letter. It is in the best interest of both sides to have the most accurate information available regarding the amount owed to the BCRC. Please see the following documents in the Downloads section at the bottom of this page for additional information: POR vs. CTR, Proof of Representation Model Language and Consent to Release Model Language.
Why is Medicare conditional?
Medicare makes this conditional payment so you will not have to use your own money to pay the bill. The payment is "conditional" because it must be repaid to Medicare when a settlement, judgment, award, or other payment is made.
How to remove CPL from Medicare?
If you or your attorney or other representative believe that any claims included on CPL/PSF or CPN should be removed from Medicare's interim conditional payment amount, documentation supporting that position must be sent to the BCRC. This process can be handled via mail, fax, or the MSPRP. Click the MSPRP link for details on how to access the MSPRP. The BCRC will adjust the conditional payment amount to account for any claims it agrees are not related to the case.
How long does it take for a BCRC to send a CPL?
Within 65 days of the issuance of the RAR Letter, the BCRC will send the CPL and Payment Summary Form (PSF). The PSF lists all items or services that Medicare has paid conditionally which the BCRC has identified as being related to the pending case.
What happens if a BCRC determines that another insurance is primary to Medicare?
If the BCRC determines that the other insurance is primary to Medicare, they will create an MSP occurrence and post it to Medicare’s records. If the MSP occurrence is related to an NGHP, the BCRC uses that information as well as information from CMS’ systems to identify and recover Medicare payments that should have been paid by another entity as primary payer.
What is conditional payment in Medicare?
A conditional payment is a payment Medicare makes for services another payer may be responsible for.
What is a POR in Medicare?
A Proof of Representation (POR) authorizes an individual or entity (including an attorney) to act on your behalf. Note: In some special circumstances, the potential third-party payer can submit Proof of Representation giving the third-party payer permission to enter into discussions with Medicare’s entities.
What is a provider in healthcare?
The term “provider” is a broad term that includes, but is not limited to physicians, staff, hospitals, nursing homes, pharmacies, and vendors, contracted with the plan to provide services to plan members, and sub-contractors.
Can you give a gift card to a member?
You are not permitted to provide any gift (e.g., cash, gift card) to a consumer/member in exchange for a referral (i.e. contact information including name and telephone number/email).
How to know if your treatment requires approval?
Refer to your plan documents, including the drug formulary, to see if your treatment requires approval. This information should be on your plan’s website. The Medicare & You handbook also contains more information.
What services do you need prior authorization for?
The services most often requiring prior approval are durable medical equipment, skilled nursing facility stays, and Part B drugs.
What does prior authorization mean?
Prior authorization means your doctor must get approval before providing a service or prescribing a medication. Now, when it comes to Advantage and Part D, coverage is often plan-specific. Meaning, you should contact your plan directly to confirm coverage.
Do you need prior authorization for Medicare Part B?
Part B covers the administration of certain drugs when given in an outpatient setting. As part of Medicare, you’ll rarely need to obtain prior authorization. Although, some meds may require your doctor to submit a Part B Drug Prior Authorization Request Form. Your doctor will provide this form.
Does Medicare Advantage cover out of network care?
Unfortunately, if Medicare doesn’t approve the request, the Advantage plan typically doesn’t cover any costs, leaving the full cost to you.
Do you need a Part B prior authorization form?
Although, some meds may require your doctor to submit a Part B Drug Prior Authorization Request Form. Your doctor will provide this form. Once the request gets approval, coverage begins.
Does Medicare require prior authorization?
Medicare Part A Prior Authorization. Medicare, including Part A, rarely requires prior authorization. If it does, you can obtain the forms to send to Medicare from your hospital or doctor. The list mostly includes durable hospital equipment and prosthetics.
What is proof of representation for Medicare?
Proof of Representation is required for the Benefits Coordination & Recovery Center (BCRC) to communicate with and provide information to an attorney that represents a Medicare beneficiary. Once the BCRC has the appropriate documentation, it can communicate with the attorney and act upon requests made by the attorney on behalf of the beneficiary. This includes furnishing conditional payment information and/or a recovery demand letter as well as addressing questions regarding the specific claims included in the conditional payment information, appeal requests, or waiver of recovery of overpayment requests. Note: A Subpoena Duces Tecum is not needed to obtain these documents when a valid Proof of Representation and or a Consent to Release is on file.
What happens if Medicare Secondary Payer is not reached?
If a resolution of the Medicare Secondary Payer recovery claim is not reached before the death of a beneficiary, new Proof of Representation on behalf of the beneficiary’s estate must be submitted. If there is no will or formal estate, the document or documents must be signed by an individual who is entitled under state law to pursue the applicable claim. For additional details, please refer to the Proof of Representation vs. Consent to Release ( POR vs. CTR) presentation which can be accessed by clicking the Medicare’s Recovery Process link.
Important Medicare Guidelines Update
Permission to Contact
- Every interaction with a potential client has a starting point. Due to a change reflected in the 2019 MCMG and now in the Medicare Advantage & Part D Communication Requirements, agents are permitted to make unsolicited direct contact with potential enrollees via email. However, the email must have an opt-out option in order to remain compliant. Add...
Scope of Appointment
- Scope of Appointment means just what it says. It’s a form outlining exactly what you’ll be presenting to a client during a meeting. The SOA ensures that potential enrollees will not be pitched plans other than those they originally requested. In 2018, the Centers for Medicare and Medicaid Services (CMS) removed the requirement for SOAs to be recorded 48 hours in advanc…
Marketing Rules
- CMS also regulates marketing and plan presentations, including when you’re allowed to market, and how you market. Agents must wait until October 1 to begin marketing next year’s plans to potential beneficiaries and cannot enroll members until October 15. In the CMS MA & Part D Communication Requirements, CMS differentiates between materials that are considered “non-…
Events & Appointments
- The types of presentations you host throughout the year typically fall under one of three categories; educational events, sales events, and individual appointments. Educational events must be advertised as such and be designed to inform Medicare beneficiaries about the parts of Medicare in general. When holding an educational event, you: MAY: 1. Distribute educational ma…
Secret Shoppers
- Staying compliant should be a year-long objective for every agent. Annual Enrollment is the culmination of revised CMS Medicare Advantage & Part D Communication Requirements, new 2022 plans, and all kinds of potential enrollees, some of which could be secret shoppers. CMS secret shoppers measure quality of service and compliance with Medicare regulations as a way …
Websites
- Consumer-facing websites that promote a specific carrier or a group of carriers’ Medicare Advantage or Part D products must be submitted to CMS for approval. This is typically accomplished through the carriers. You may refer to the specific carrier’s policy regarding website review. CMS has increasingly cracked down on websites in recent years, so it’s important to be s…