What is the Medicare initial enrollment period?
You have an Initial Enrollment Period of seven months (3 months before and after you become eligible) to add additional Medicare health care coverage with an Advantage plan, or Supplemental Insurance (Medigap policies) and/or a Prescription Drug plan. Medicare enrollment or changes to plans you are already enrolled in are limited to specific times.
How many people are enrolling in Medicare cost plan plans?
But there were far fewer Medicare cost plan enrollees as of 2019, due to the implementation of the Medicare Advantage competition clause. According to a Kaiser Family Foundation analysis, the total number of cost plan enrollees dropped to about 200,000 people as of 2019.
What is a Medicare cost plan?
A Medicare cost plan is similar to a Medicare Advantage plan in that enrollees have access to a network of doctors and hospitals, and may have additional benefits beyond what’s provided by Original Medicare. But unlike Medicare Advantage plans, a cost plan offers policyholders the option...
How do I enroll in a Medicare cost plan?
Companies that offer Medicare cost plans must provide Medicare beneficiaries with an open enrollment period of at least 30 days. During this time, you’ll submit an application to the plan’s provider to enroll. Enrollment details may be different depending on the company that’s offering the cost plan.
What is Medicare cost plan?
What is a Medicare cost plan? A Medicare cost plan is similar to a Medicare Advantage plan in that enrollees have access to a network of doctors and hospitals, and may have additional benefits beyond what’s provided by Original Medicare.
How many Medicare plans are there in Minnesota?
There wee 27 cost plans available in Minnesota as of 2018, and although that dropped in 2019, there are still 21 plans available in Minnesota in 2020. People who still have Medicare cost plans available in their area can still enroll, and there are cost plans available in 2020 in Colorado, Iowa, Illinois, Maryland, Minnesota, Nebraska, ...
What is the competition clause in Medicare?
The Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (which rebranded Medicare+Choice as Medicare Advantage) created a competition clause that banned Medicare Cost plans from operating in areas where they faced substantial competition from Medicare Advantage plans.
How many people are on Medicare in 2019?
According to a Kaiser Family Foundation analysis, the total number of cost plan enrollees dropped to about 200,000 people as of 2019.
Which states do not have Medicare?
The rest were spread across Colorado, District of Columbia, Iowa, Illinois, Maryland, North Dakota, South Dakota, Texas, Virginia, and Wisconsin; most states do not have Medicare cost plans available. But there were far fewer Medicare cost plan enrollees as of 2019, due to the implementation of the Medicare Advantage competition clause.
Who can join Medicare?
Who can join a Medicare cost plan? Eligible enrollees who live within a Medicare cost plan’s service area can join the plan when it’s accepting new members. A cost plan that is accepting new enrollees must have an annual open enrollment window of at least 30 days, although they can set an enrollment cap and close enrollment once it’s reached.
Does a cost plan have supplemental Part D?
If the cost plan offers optional supplemental Part D prescription coverage, enrollment in (or disenrollment from) the Part D coverage is limited to the normal annual open enrollment period for Part D plans. If the cost plan does not have a supplemental Part D plan available — or if it does and the enrollee would prefer a different Part D plan — ...
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
How much is coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). Beyond Lifetime reserve days : All costs. Note. You pay for private-duty nursing, a television, or a phone in your room.
How much is coinsurance for 61-90?
Days 61-90: $371 coinsurance per day of each benefit period. Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime) Beyond lifetime reserve days: all costs. Part B premium.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
Do you pay more for outpatient services in a hospital?
For services that can also be provided in a doctor’s office, you may pay more for outpatient services you get in a hospital than you’ll pay for the same care in a doctor’s office . However, the hospital outpatient Copayment for the service is capped at the inpatient deductible amount.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.
When is the best time to join Medicare?
The best time to join a Medicare health or drug plan is when you first get Medicare. Signing up when you’re first eligible can help you avoid paying a lifetime Part D late enrollment penalty. If you miss your first chance, generally you have to wait until fall for Medicare’s annual Open Enrollment Period (October 15–December 7) to join a plan.
How to get Medicare if you are not collecting Social Security?
If you’re not already collecting Social Security benefits before your Initial Enrollment Period starts, you’ll need to sign up for Medicare online or contact Social Security. To get the most from your Medicare and avoid the Part B late enrollment penalty, complete your Medicare enrollment application during your Initial Enrollment Period.
What is Medicare cost plan?
A Medicare cost plan blends parts of both original Medicare and Medicare Advantage. These plans work together with your original Medicare coverage while providing additional benefits and flexibility. Medicare cost plans are very similar to Medicare Advantage plans. However, there are some key differences between the two.
How long does it take to enroll in Medicare?
Companies that offer Medicare cost plans must provide Medicare beneficiaries with an open enrollment period of at least 30 days. During this time, you’ll submit an application to the plan’s provider to enroll. Enrollment details may be different depending on the company that’s offering the cost plan.
What are the benefits of Medicare Advantage?
These plans offer many of the extra benefits that come with Medicare Advantage plans, such as dental, vision, and hearing care . However, unlike Medicare Advantage plans, people with Medicare cost plans have more flexibility to use out-of-network doctors and to choose a separate Part D plan.
How to enroll in Medicare Part B?
To enroll in a Medicare cost plan, you must meet the following eligibility requirements: 1 be enrolled in Medicare Part B 2 live in an area where Medicare cost plans are offered 3 find a Medicare cost plan that’s accepting new members 4 complete an application during the plan’s enrollment period 5 agree to all cost plan rules that are disclosed during the enrollment process
What happens when you enroll in Medicare?
When you enroll in a Medicare cost plan, you gain access to the plan’s network of healthcare providers. You can either choose a provider within this network or an out-of-network provider. When you go out of network, it’s covered by original Medicare.
How old do you have to be to get Medicare?
To enroll in a Medicare cost plan, you must first be enrolled in Medicare Part B. To be eligible for Part B, you must meet one of the following criteria: be age 65 or older. have a disability and receive Social Security Disability Insurance.
Does Medicare have a Part D plan?
Additionally, some Medicare cost plans come bundled with Part D prescription drug coverage . If your plan doesn’t include Part D, you can enroll in a separate Part D plan that best suits your needs. There’s also additional flexibility in switching plans.
When does Medicare change plans?
Medicare health and drug plans can make changes each year—things like cost, coverage, and what providers and pharmacies are in their networks. October 15 to December 7 is when all people with Medicare can change their Medicare health plans and prescription drug coverage for the following year to better meet their needs.
What is an ANOC in Medicare?
People in a Medicare health or prescription drug plan should always review the materials their plans send them, like the “Evidence of Coverage” (EOC) and “Annual Notice of Change” (ANOC). If their plans are changing, they should make sure their plans will still meet their needs for the following year.
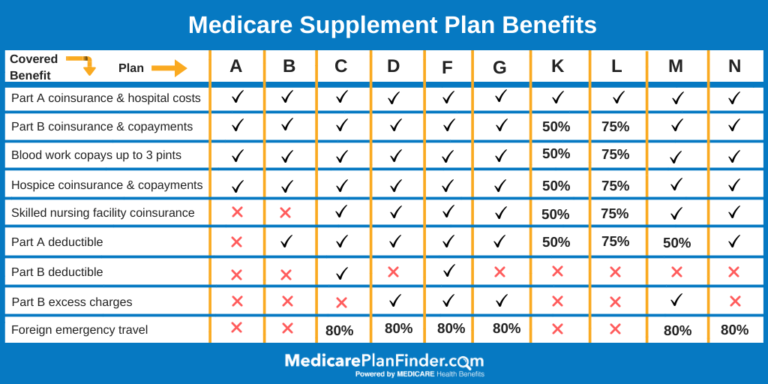
What is a Medigap plan?
These plans, also known as “ Medigap ,” provide coverage for some of Medicare’s out-of-pocket costs, such as deductibles, coinsurance and copayments. Some Medigap plans even include annual out-of-pocket spending limits. Sign up for a Medicare Advantage plan.
How much is Medicare Part B?
Part B. The standard Medicare Part B premium is $148.50 per month. However, the Part B premium is based on your reported taxable income from two years prior. The table below shows what Part B beneficiaries will pay for their premiums in 2021, based off their 2019 reported income. Medicare Part B IRMAA.
How much is the deductible for Part D in 2021?
Part D. Deductibles vary according to plan. However, Part D deductibles are not allowed to exceed $455 in 2021, and many Part D plans do not have a deductible at all. The average Part D deductible in 2021 is $342.97. 1.
How much coinsurance is required for hospice?
A 5 percent coinsurance payment is also required for inpatient respite care. For durable medical equipment used for home health care, a 20 percent coinsurance payment is required.
What is Medicare Part D based on?
Part D premiums also come with an income-based tier system that uses your reported income from two years prior, similar to how Medicare Part B premiums are calculated. Part D premiums for 2021 will be based on reported taxable income from 2019, and the breakdown is as follows: Medicare Part D IRMAA. 2019 Individual tax return.
How much is a copayment for a mental health facility?
For an extended stay in a hospital or mental health facility, a copayment of $371 per day is required for days 61-90 of your stay, and $742 per “lifetime reserve day” thereafter.
How much can you save if you don't accept Medicare?
If you are enrolled in Original Medicare, avoiding health care providers who do not accept Medicare assignment can help you save up to 15 percent on excess charges. Read additional medicare costs guides to learn more about Medicare costs and how they will affect you.