Key Takeaways:
- Medicare benefits are available to individuals under age 65 if they meet certain disability requirements.
- Medicare benefits for individuals under age 65 with a disability are the same as those for seniors over age 65.
- In many cases, if you are eligible for Medicare due to a disability, you will be automatically enrolled—you don't have to sign up.
What qualifies you for Medicare disability benefits?
Who qualifies for SSDI?
- People who have worked for a number of years and had enough money taken out of their paychecks for Social Security (FICA)
- Self-employed people who paid self-employment taxes
- You must meet Social Security’s very strict definition of disability to qualify for SSDI.
- Having a low income or financial needs do not affect whether you can get SSDI.
What does disability qualify for Medicare?
The takeaway
- Medicare coverage is available for people with a disability who receive SSDI.
- You’ll automatically be enrolled in parts A and B after your 24th month of SSDI benefits.
- You can choose to decline Medicare Part B coverage if you have other options that work better for your budget.
Does a disabled person qualify for Medicare?
To become eligible for Medicare based on disability, you must first qualify for Social Security Disability Insurance. SSDI pays monthly benefits to people with disabilities who might be limited in their ability to work. If you are injured or have a medical condition that limits your ability to work, you may be eligible for SSDI.
Do I have to take Medicare on disability?
You can get Medicare coverage as long as you have a disability and have been approved for SSDI. There are two exceptions to the 2-year waiting period. If you have amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s Disease, you’ll be enrolled in coverage in the first month you receive SSDI.
What Is Medicare a disability program?
Medicare is a health insurance program for people 65 years of age and older, some disabled people under 65 years of age, and people with end-Stage Renal Disease (permanent kidney failure treated with dialysis or a transplant).
What is the difference between Medicare and Social Security disability?
Both programs help those in retirement or on disability. Medicare provides health insurance, while Social Security provides a monthly income.
What happens to my Medicare disability when I turn 65?
What Happens When You Turn 65? When you turn 65, you essentially lose your entitlement to Medicare based on disability and become entitled based on age. In short, you get another chance to enroll, a second Initial Enrollment Period if you will.
Does Medicare automatically come with disability?
You will typically be automatically enrolled in Original Medicare, Part A and B, after you've received Social Security disability benefits (or certain Railroad Retirement Board disability benefits) for two straight years. Your Medicare coverage will start 24 months from the month you qualified for disability benefits.
What is the monthly amount for Social Security disability?
SSDI payments range on average between $800 and $1,800 per month. The maximum benefit you could receive in 2020 is $3,011 per month. The SSA has an online benefits calculator that you can use to obtain an estimate of your monthly benefits.
What kind of insurance do you get with disability?
Social Security Disability Insurance (SSDI)
Does disability pay more than Social Security?
However, if you're wondering if disability would pay more, just ask yourself where you are relative to your full retirement age. If you're under it, disability will be higher. If you're above it, Social Security will be higher.
At what age does disability convert to Social Security?
When you reach the age of 65, your Social Security disability benefits stop and you automatically begin receiving Social Security retirement benefits instead. The specific amount of money you receive each month generally remains the same.
Can you collect disability and Social Security at the same time?
Yes, you can receive Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI) at the same time. Social Security uses the term “concurrent” when you qualify for both disability benefits it administers.
Will my disability benefits change when I turn 65?
The Benefits Do Convert Nothing will change. You will continue to receive a monthly check and you do not need to do anything in order to receive your benefits. The SSA will simply change your disability benefit to a retirement benefit once you have reached full retirement age.
What other benefits can I get with Social Security disability?
If you get SSI, you also may be able to get other benefits, such as Medicaid and the Supplemental Nutrition Assistance Program (SNAP). For more information about SSI, read Supplemental Security Income (SSI) (Publication No. 05-11000). After you receive disability benefits for 24 months, you'll be eligible for Medicare.
Does Medicare cover 100 percent of hospital bills?
Medicare generally covers 100% of your medical expenses if you are admitted as a public patient in a public hospital. As a public patient, you generally won't be able to choose your own doctor or choose the day that you are admitted to hospital.
How long can you get Medicare after you have been disabled?
Indefinite Access to Medicare. Even after the eight-and-one-half year period of extended Medicare coverage has ended, working individuals with disabilities can continue to receive benefits as long as the individual remains medically disabled.
What is covered by Medicare?
Coverage includes certain hospital, nursing home, home health, physician, and community-based services. The health care services do not have to be related to the individual’s disability in order to be covered.
What are the requirements for Medicare for ESRD?
The requirements for Medicare eligibility for people with ESRD and ALS are: ALS – Immediately upon collecting Social Security Disability benefits. People who meet all the criteria for Social Security Disability are generally automatically enrolled in Parts A and B.
How long do you have to wait to get Medicare?
There is a five month waiting period after a beneficiary is ...
How long does Medicare coverage last?
Medicare eligibility for working people with disabilities falls into three distinct time frames. The first is the trial work period, which extends for 9 months after a disabled individual obtains a job.
Why should beneficiaries not be denied coverage?
Beneficiaries should not be denied coverage simply because their underlying condition will not improve.
How long does a disabled person have to work to get a job?
The first is the trial work period, which extends for 9 months after a disabled individual obtains a job. The second is the seven-and-three-quarter years (93 months) after the end of the trial work period. Finally, there is an indefinite period following those 93 months.
How long does a disability last?
Generally, this means you are unable to work and that your condition is expected to last for at least a year. Medicare doesn’t determine who is eligible for disability coverage.
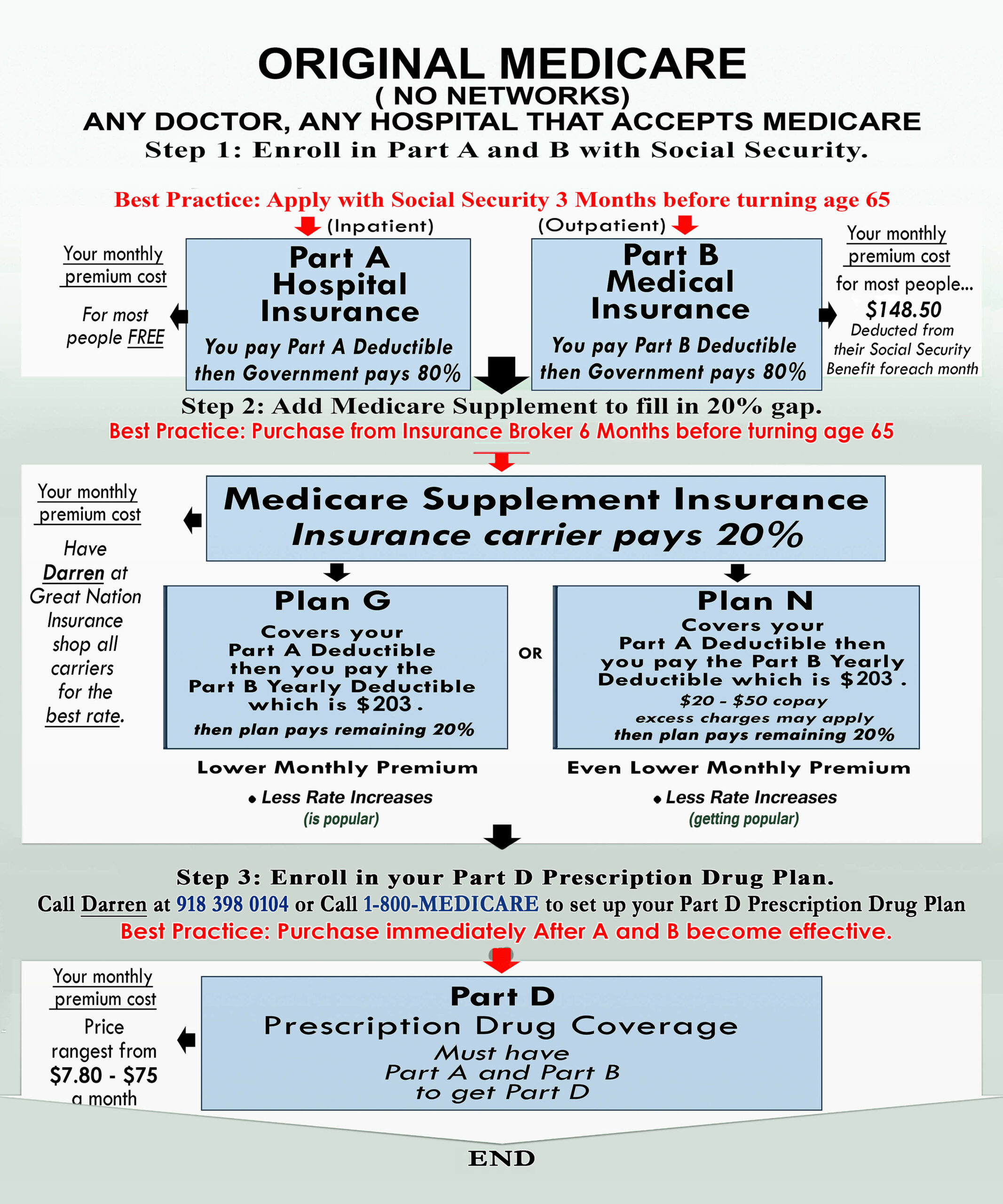
How much is Medicare Part B 2021?
The standard Part B premium for 2021 is $148.50 per month. The deductible for Medicare Part B in 2021 is $203. After you meet the deductible, some services are covered in full. You’ll pay 20 percent of the Medicare-approved amount for other services.
How long do you have to wait to get Medicare?
In most cases, you’ll need to wait 24 months before your Medicare coverage begins. There is a 2-year waiting period that begins the first month you receive a Social Security benefit check.
How much is hospitalization for Medicare Part A 2021?
In 2021, hospitalization costs with Medicare Part A include: Deductible: $1,484 for each benefit period. Days 1–60: after the deductible has been met, inpatient stays will be completely covered until the 60th day the benefit period. Days 61–90: $371 per day coinsurance.
What is Part B insurance?
Part B is used to pay for a wide range of medical services, including doctor and specialist appointments, emergency room visits, ambulance services, medical equipment, preventive care, and some medications. You’ll normally pay a monthly premium for Part B coverage.
When does Medicare start covering ALS?
If you have amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s Disease, you’ll be enrolled in coverage in the first month you receive SSDI. If you have end stage renal disease (ESRD), your Medicare coverage normally begins after you’ve received 3 months of dialysis treatment.
Can I get Medicare Part B after 24 months?
The takeaway. Medicare coverage is available for people with a disability who receive SSDI. You’ll automatically be enrolled in parts A and B after your 24th month of SSDI benefits. You can choose to decline Medicare Part B coverage if you have other options that work better for your budget.
What is SSI disability?
Supplemental Security Income (SSI) Disability & Medicaid coverage. Waiting for a disability status decision and don’t have health insurance. No disability benefits, no health coverage. The Marketplace application and disabilities. More information about health care for people with disabilities.
How long do you have to wait to get Medicare if you have Social Security Disability?
Social Security Disability Insurance (SSDI) & Medicare coverage. If you get Social Security Disability Income (SSDI), you probably have Medicare or are in a 24-month waiting period before it starts. You have options in either case.
Can I enroll in a Medicare Marketplace plan if I have Social Security Disability?
You’re considered covered under the health care law and don’t have to pay the penalty that people without coverage must pay. You can’t enroll in a Marketplace plan to replace or supplement your Medicare coverage.
Can I keep my Medicare Marketplace plan?
One exception: If you enrolled in a Marketplace plan before getting Medicare, you can keep your Marketplace plan as supplemental insurance when you enroll in Medicare. But if you do this, you’ll lose any premium tax credits and other savings for your Marketplace plan. Learn about other Medicare supplement options.
Can I get medicaid if I have SSDI?
You may be able to get Medicaid coverage while you wait. You can apply 2 ways: Create an account or log in to complete an application. Answer “ yes” when asked if you have a disability.
Can I get medicaid if I'm turned down?
If you’re turned down for Medicaid, you may be able to enroll in a private health plan through the Marketplace while waiting for your Medicare coverage to start.
How many people are covered by Medicare?
Medicare provides coverage for about 10 million disabled Americans under the age of 65 . Medicare isn't available to most people until age 65, but if you have a long-term disability or have been diagnosed with certain diseases, Medicare is available at any age.
When do you get Medicare cards?
You'll get Medicare cards in the mail three months before your 25th month of disability.
How to apply for SSDI?
Your application for SSDI is likely to move more quickly if you select one doctor as the lead contact for your case. It's best to go with one who: 1 Has experience with disability cases 2 Responds promptly to requests for information 3 Is familiar with your overall health situation
How long does it take to get approved for SSDI?
However, getting approved for SSDI can be a long process, and even after you're approved, you'll have to wait 24 months before your Medicare benefits begin (with exceptions for end-stage renal disease and amyotrophic lateral sclerosis).
How long does Medicare cover ESRD?
If you have employer-sponsored or union-sponsored insurance and you become eligible for Medicare due to ESRD, Medicare will coordinate with your existing coverage for 30 months. During that time, your private insurance will be your primary coverage, and Medicare will pick up a portion of the remaining costs.
What happens if you don't want Medicare Part B?
If you don't want Medicare Part B, you can send back the card. If you keep the card, you'll keep Part B and will pay Part B premiums. In 2021, the Part B premium is $148.50 per month for most enrollees. 6 . You'll also be eligible to join a Medicare Part D prescription drug plan.
How long does it take for SSDI to start?
According to the law, your SSDI payments cannot start until you have been disabled for at least five full months. 4 Your payment will usually start with your sixth month of disability.
How long does disability last on Social Security?
To qualify for either program, you must meet SSA’s definition of disability : You’re unable to do substantial gainful activity (work) Your disability is expected to last for at least one year or result in death. Your impairment is on Social Security’s list of disabling medical conditions.
How long does a disability policy last?
Types of Disability Policies. There are two types of disability policies. Short-term policies may pay for up to two years. Most last for a few months to a year. Long-term policies may pay benefits for a few years or until the disability ends. Employers who offer coverage may provide short-term coverage, long-term coverage, or both.
What is SSDI for spouse?
Social Security Disability Insurance (SSDI) Social Security Disability Insurance ( SSDI) is for people who have become disabled after earning enough Social Security work credits within a certain time. Your spouse or former spouse and your children may be eligible for benefits when you start getting SSDI. You can apply for SSDI benefits online, by ...
What age does Medicare cover?
Medicare provides medical health insurance to people under 65 with certain disabilities and any age with end-stage renal disease (permanent kidney failure requiring dialysis or a kidney transplant). Learn about eligibility, how to apply and coverage. Affordable Care Act Marketplace offers options to people who have a disability, ...
What is the Affordable Care Act Marketplace?
Affordable Care Act Marketplace offers options to people who have a disability, don’t qualify for disability benefits, and need health coverage. Learn about the Marketplace, how to enroll, and use your coverage.
How long does it take to get SSDI?
You can apply for SSDI benefits online, by phone, or in person . If your application is approved, you’ll have a five-month waiting period for benefits to start. If your application is denied, you can appeal the decision.
How do I apply for SSI?
How to Apply for Supplemental Security Income (SSI) Adults can apply for SSI by phone, in person at a local Social Security office, or in some cases online. To apply for SSI for a child, you can start the process online but will need to complete it either in person or by phone.
How long is a person eligible for Medicare?
Everyone eligible for Social Security Disability Insurance (SSDI) benefits is also eligible for Medicare after a 24-month qualifying period. The first 24 months of disability benefit entitlement is the waiting period for Medicare coverage. During this qualifying period for Medicare, the beneficiary may be eligible for health insurance ...
Why does Bill have Medicare?
Example: Bill has Medicare coverage because of permanent kidney failure. He also has group health plan coverage through the company he works for. His group health coverage will be his primary payer for the first 30 months after Bill becomes eligible for Medicare. After 30 months, Medicare becomes the primary payer.
How long can you keep Medicare after you return to work?
Answer: As long as your disabling condition still meets our rules, you can keep your Medicare coverage for at least 8 ½ years after you return to work. (The 8 ½ years includes your nine month trial work period.) Question: I have Medicare hospital Insurance (Part A) and medical insurance (Part B) coverage.
What is a large group health plan?
If the employer has 100 employees or more, the health plan is called a large group health plan. If you are covered by a large group health plan because of your current employment or the current employment of a family member, Medicare is the secondary payer (see example below).
How to order a publication from Medicare?
Answer: You can view, print, or order publications online or by calling 1-800-MEDICARE (1-800-633-4227). The fastest way to get a publication is to use our search tool and then view and print it. If you order online or through 1-800-MEDICARE, you will receive your order within 3 weeks. The link to search publications is at: http://www.medicare.gov/Publications/home.asp
Is Medicare a secondary payer?
Answer: Medicare may be the "secondary payer" when you have health care coverage through your work. See the information under "Coordination of Medicare and Other Coverage for Working Beneficiaries with Disabilities" about when Medicare is a "secondary payer or primary payer".
Does Medicare pay for non-VA hospital?
If the VA authorizes services in a non-VA hospital, but doesn't pay for all of the services you get during your hospital stay, then Medicare may pay for the Medicare-covered part of the services that the VA does not pay for. Example: John, a veteran, goes to a non-VA hospital for a service that is authorized by the VA.
What is Medicare Advantage?
Medicare Advantage Plans for Disabled Under 65. Most Social Security Disability Advantage plans combine Medicare coverage with other benefits like prescription drugs, vision, and dental coverage. Medicare Advantage can be either HMOs or PPOs. You may have to pay a monthly premium, an annual deductible, and copays or coinsurance for each healthcare ...
How long do you have to be on Medicare if you are 65?
When you’re under 65, you become eligible for Medicare if: You’ve received Social Security Disability Insurance (SSDI) checks for at least 24 months. At the end of the 24 months, you’ll automatically enroll in Parts A and B. You have End-Stage Renal Disease (ESRD) and need dialysis or a kidney transplant. You can get benefits with no waiting period ...
What is a special needs plan?
A Special Needs Plan fits the healthcare needs of the people in the policy.
Can a disabled child get medicare?
Medicare for Disabled Youth. Children under the age of 20 with ESRD can qualify for Medicare if they need regular dialysis treatment and at least one of their parents is eligible for or receives Social Security retirement benefits. If your child is over the age of 20, they qualify for Medicare after receiving SSDI benefits for at least 24 months.
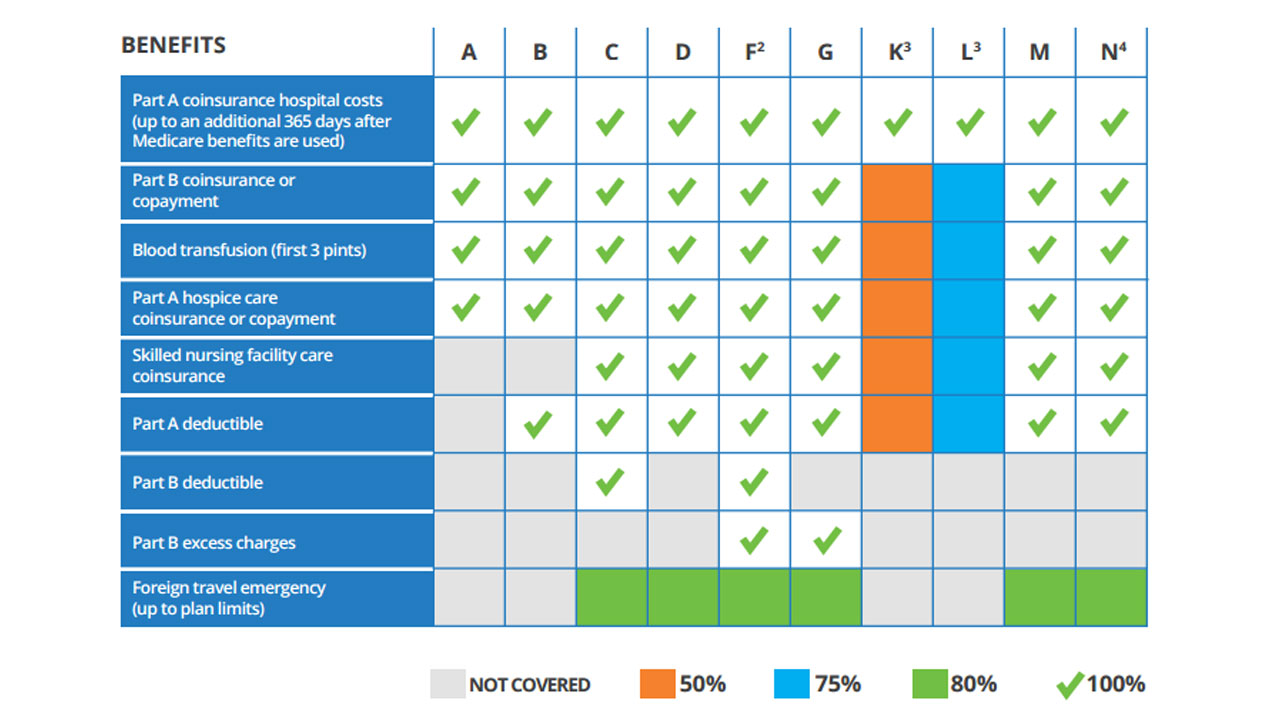
Does Medicare cover Medigap?
Medicare pays a large portion of the cost, but not all of it. Medigap can help cover what Medicare doesn’t cover. But if you’re under 65, it can be hard to find an affordable Medigap plan. While some states require companies to offer at least one Medigap plan to people under age 65, others do not.
Is Medigap premium higher at 65?
Additionally, premiums for this plan are lower since it includes fewer benefits. As Medigap premiums are much higher when you’re under 65, it can be beneficial to enroll in a Plan such as A to control costs and switch to a plan with more benefits after you turn 65.
Can you sign up for Medicare and Medicaid?
Many people on Social Security Disability also qualify for their state’s Medicaid program. If you’re on Medicare and Medicaid, you can still sign up for an Advantage plan. The two programs together will usually cover almost all your healthcare costs.