Medicare part A modifiers full list
| Program | Category | Modifier Code | Description |
| PART – A | E/M | 25 | Significant, separately identifiable Eva ... |
| PART – A | Method II CAH | 26 | Professional component |
| PART – A | E/M | 27 | Multiple outpatient hospital Evaluation ... |
| PART – A | Anatomical | 50 | Bilateral procedure |
Which modifier goes first 25 or 95?
You put the modifier that affects payment the most first. Since AI is informational only and the 25 determine if the visit level should be paid ... put the 25 first then the AI You must log in or register to reply here.
What is Kx modifier with Medicare?
KX Modifier Thresholds (formerly known as Therapy Cap Process) Under Medicare Part B, the annual limitations on per beneficiary incurred expenses for outpatient therapy services are commonly referred to as “therapy caps” now known as KX modifier thresholds. The KX modifier thresholds are determined on a calendar year basis, which means that all beneficiaries begin a new threshold amount each year.
What is a Gy modifier for Medicare?
- Are proper and needed for the diagnosis or treatment of the patient’s medical condition
- Are furnished for the diagnosis, direct care, and treatment of the patient’s medical condition
- Meet the standards of good medical practice
- Are not mainly for the convenience of the patient, provider, or supplier Examples of services that are covered include:
When to use Medicare ABN claim modifiers?
You may also use the ABN as a voluntary notice to alert patients of their financial liability prior to providing care that Medicare never covers. An ABN is not required to bill a patient for an item or service that is not a Medicare benefit and is never covered. Medicare prohibits routine issuing of ABNs.
What is modifier is used for?
Modifiers indicate that a service or procedure performed has been altered by some specific circumstance, but not changed in its definition or code. They are used to add information or change the description of service to improve accuracy or specificity.
What are payment modifiers?
Modifier: Two digit numeric or alpha-number descriptor that is used by providers to indicate that a service or procedure has been altered by a specific circumstance, but the procedure code and definition is unchanged. 4.
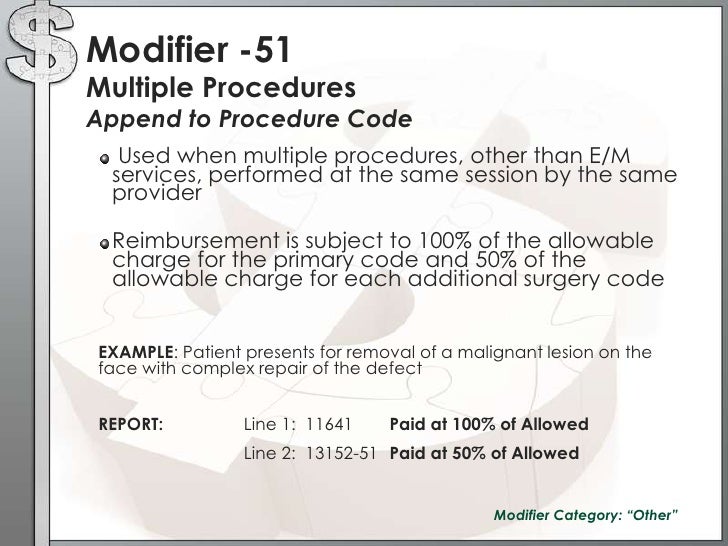
What is the use of the 51 and 59 modifiers?
Modifier 51 impacts the payment amount, and modifier 59 affects whether the service will be paid at all. Modifier 59 is typically used to override National Correct Coding Initiative (NCCI) Edits. NCCI edits include a status indicator of 0, 1, or 9.
Which modifier is used for Medicare patients?
The GA modifier must be used when physicians, practitioners, or suppliers want to indicate that they expect that Medicare will deny a service as not reasonable and necessary and they do have on file an ABN signed by the beneficiary.
What are CPT modifiers?
CPT modifiers (also referred to as Level I modifiers) are used to supplement the information or adjust care descriptions to provide extra details concerning a procedure or service provided by a physician. Code modifiers help further describe a procedure code without changing its definition.
What is modifier 50 used for?
Use modifier 50 to report bilateral procedures performed during the same operative session by the same physician in either separate operative areas (e.g., hands, feet, legs, arms, ears) or in the same operative area (e.g., nose, eyes, breasts).
What is the 32 modifier used for?
When to use Modifier 32. Modifier -32 indicates a service that is required by a third-party entity, Worker's Compensation, or some other official body. Modifier 32 is no used to report a second opinion request by a patient, a family member or another physician. This modifier is used only when a service is mandated.
What is the difference between modifier 50 and 51?
Modifier 50 Bilateral procedure describes procedures or services that take place on identical, opposing structures (e.g., shoulder joints, breasts, eyes). Use modifier 51 Multiple procedures to show that the same provider performed multiple procedures (other than E/M services) during the same session.
What is a CPT modifier?
CPT Modifiers are an important part of the managed care system or medical billing. A service or procedure that has both a professional and technical component. (26 or TC) A service or procedure that was performed more than once on the same day by the same physician or by a different physician. (76 or 77)
Why is CPT modifier important?
CPT Modifiers are also playing an important role to reduce the denials also. Using the correct modifier is to reduce the claims defect and increase the clean claim rate also. The updated list of modifiers for medical billing is mention below
What is a modifier 76?
Modifier 76- Repeat procedure or service by the same physician or other qualified healthcare professional. It may be necessary to indicate that procedure or service was repeated by the same physician or other qualified health professional subsequent to the original procedure or service.
What is NCCI PTP modifier?
An NCCI PTP-associated modifier is a modifier that Medicare and Medicaid accept to bypass an NCCI PTP edit under appropriate clinical circumstances. Bypassing or overriding an edit is also called unbundling.
Why do medical coders use modifiers?
Medical coders use modifiers to tell the story of a particular encounter. For instance, a coder may use a modifier to indicate a service did not occur exactly as described by a CPT ® or HCPCS Level II code descriptor, but the circumstance did not change the code that applies. A modifier also may provide details not included in the code descriptor, ...
What is a pricing modifier?
A pricing modifier is a medical coding modifier that causes a pricing change for the code reported. The Multi-Carrier System (MCS) that Medicare uses for claims processing requires pricing modifiers to be in the first modifier position, before any informational modifiers. On the CMS 1500 claim form, the appropriate field is 24D (shown below). You enter the pricing modifier directly to the right of the procedure code on the claim. Most providers use the electronic equivalent of this form to bill Medicare for professional (pro-fee) services.
What is a modifier 59?
Modifier 59 Distinct procedural service is a medical coding modifier that indicates documentation supports reporting non-E/M services or procedures together that you normally wouldn’t report on the same date. Appending modifier 59 signifies the code represents a procedure or service independent from other codes reported and deserves separate payment.
What is informational modifier?
An informational modifier is a medical coding modifier not classified as a payment modifier. Another name for informational modifiers is statistical modifiers. These modifiers belong after pricing modifiers on the claim.
Why is modifier 59 difficult to master?
Like modifier 25, modifier 59 is difficult to master because it requires determining whether the code is truly distinct and separately reportable from other codes. The CPT ® definition of modifier 59 advises that the modifier may be appropriate for a code when documentation shows at least one of the following:
What is a co surgeon?
The CO-SURG (Co-surgeons) column is related to modifier 62 Two surgeons. Medicare’s Global Surgery Booklet provides these examples: 1 A procedure requires two physicians of different specialties to perform it. Each reports the code with modifier 62 appended 2 Two surgeons simultaneously perform parts of a procedure, such as for a heart transplant or bilateral knee replacements. Again, each surgeon reports the code with modifier 62 appended.
What is modifier 22?
22—Increased Procedural Services: Documentation is required when billing with this modifier. A short explanation of why this modifier was applied will also help expedite the processing of claims.#N#24—Unrelated E&M Service by Same Physician During a Postoperative Period: Used when a physician performs an E&M service during a postoperative period for a reason (s) unrelated to the original procedure.#N#25—Significant, Separately Identifiable E&M Service by the Same Physician on the Same Day of the Procedure or Other Service: Used by provider to indicate that on the same date of service, the provider performed two significant, separately identifiable services that are not “unbundled”.#N#26 or PC—Professional Component: Certain procedures are a combination of a physician component and a technical component, and this modifier is used when the physician is providing only the interpretation portion. TC—Technical Component: Certain procedures are a combination of a provider component and a technical component, and this modifier is used when the provider is performing only the technical portion of a service.#N#32—Mandated Services: Services related to mandated consultation and/or related services (e.g., third party payer, governmental, legislative, or regulatory requirement) may be identified by adding modifier 32 to the basic procedure.#N#47—Anesthesia by Surgeon: Regional or general anesthesia provided by a surgeon may be reported by adding this modifier to the surgical procedure. Amount allowed is 25% of the surgical procedure allowance.
What is a modifier in Medicare?
Modifiers Definition#N#A modifier provides the means by which the reporting provider can indicate that a service or procedure that has been performed has been altered by some specific circumstance but not changed in its definition or code.#N#For Medicare purposes, modifiers are two-digit codes that may consist of alpha and/or numeric characters, which may be appended to Healthcare Common Procedure Coding System (HCPCS) procedure codes to provide additional information needed to process a claim. This includes HCPCS Level 1, also known as Current Procedural Terminology® (CPT®) codes, and HCPCS Level II codes. Modifiers answer questions such as: which one, how many, what kind and when.#N#What is the purpose of using a modifier?
Can you use modifier 22 on E&M?
However, this modifier should not be used on E&M services. E&M codes with a modifier 22 will be denied. If modifier 22 is used on any surgical procedure, then it must only be used on surgeries which have a global period of 000, 010, 090, or YYY identified on the Medicare Physician Fee Schedule Relative Value File
Does a modifier affect reimbursement?
In some cases, addition of a modifier may directly affect payment. Placement of a modifier after a CPT® or HCPCS code does not ensure reimbursement. Medical documentation may be requested to support the use of the assigned modifier.

Four New Modifiers to Use Instead of Modifier 59 – Xe, XS, XP & Xu
What Is Modifier 59?
- Modifier 59 is used to define a “Distinct Procedural Service.” These are procedures and services performed by a healthcare provider that are not typically reported together, but are appropriate and separately billable given the circumstances. When modifier 59 is appended to a CPT code, it indicates that the service is separate and distinct from another service with which it would usual…
Why New Modifiers?
- Modifier 59 is not only the most used modifier, but it’s also the most abused. And while the abuse may be unintentional at times, the improper coding leads to incorrectly paid claims. As audits have increased, CMS has realized that more specific modifiers may be helpful in deterring this abuse. The -X{EPSU} modifiers are essentially a subset of modifier 59. CMS believes their usag…
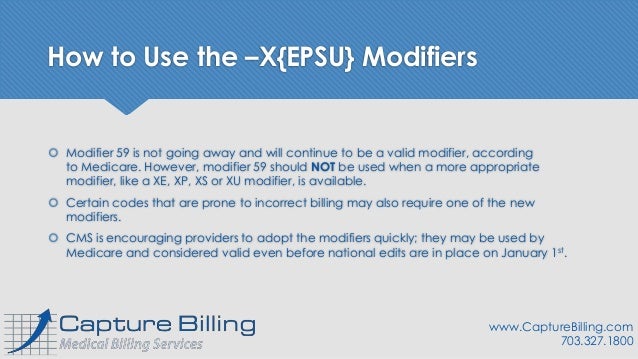
How to Use The –X{EPSU} Modifiers
- Modifier 59 is not going away and will continue to be a valid modifier, according to Medicare. However, modifier 59 should NOTbe used when a more appropriate modifier, like a XE, XP, XS or XU modifier, is available. Certain codes that are prone to incorrect billing may also require one of the new modifiers. CMS is encouraging providers to adopt the modifiers quickly; they may be us…
Additional Information
- Medicare Learning Network: MLM MM8863 Manual System: Transmittal 1422 Here is a link to my other post with some examples of how to use the new modifiers. CLICK FOR MODIFIER EXAMPLES Still confused? Feel free to ask questions in the comments and we’ll do our best to answer!