How much savings can you have on Medicare?
You may have up to $2,000 in assets as an individual or $3,000 in assets as a couple. As of July 1, 2022 the asset limit for some Medi-Cal programs will go up to $130,000 for an individual and $195,000 for a couple. These programs include all the ones listed below except Supplemental Security Income (SSI).
How do you qualify to get $144 back from Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.
What is the difference between the Medicare and Medicaid programs?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
Is QMB the same as Medicare?
The Qualified Medicare Beneficiary (QMB) Program is one of the four Medicare Savings Programs that allows you to get help from your state to pay your Medicare premiums. This Program helps pay for Part A premiums, Part B premiums, and deductibles, coinsurance, and copayments.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
Who is eligible for Medicare Part B reimbursement?
1. How do I know if I am eligible for Part B reimbursement? You must be a retired member or qualified survivor who is receiving a pension and is eligible for a health subsidy, and enrolled in both Medicare Parts A and B.
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
How do I qualify for dual Medicare and Medicaid?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).
Does Social Security count as income for QMB?
An individual making $1,000 per month from Social Security is under the income limit. However, if that individual has $10,000 in savings, they are over the QMB asset limit of $8,400.
What does Medicare QMB mean?
Qualified Medicare BeneficiaryThe Qualified Medicare Beneficiary (QMB) program provides Medicare coverage of Part A and Part B premiums and cost sharing to low-income Medicare beneficiaries.
What does SLMB mean?
Specified Low-Income Medicare BeneficiaryWhat is this program? The Specified Low-Income Medicare Beneficiary (SLMB) Program is one of the four Medicare Savings Programs that allows you to get help from your state to pay your Medicare premiums.
What is Medicare Savings Program?
A Medicare Savings Program (MSP) is designed to cover all or part of Medicare out-of-pocket expenses that encumber Medicare recipients who live within limited financial means.
What is a Medicare summary notice?
You will also receive a Medicare Summary Notice (MSN), which is proof of being in the program and shows the healthcare provider you should not be billed for services, deductibles, coinsurance or copayments. An exception is outpatient prescriptions.
What is QDWI in Medicare?
Qualified Disabled and Working Individuals (QDWI) Program for Part A premiums. If your application for the QMB Program is accepted, you will receive a QMB card. Be sure to show this card along with your Medicare or Medicaid card every time you receive healthcare services. You will also receive a Medicare Summary Notice (MSN), ...
Is Medicare cost prohibitive?
The cost of Medicare benefits in the form of premiums, coinsurance, copayments and deductibles can raise concerns about affordability, especially when you are on a limited income. For Medicare recipients under a certain income and asset level, Medicare benefits can be cost prohibitive.
What is Medicare Savings Program?
A Medicare Savings Program (MSP) can help pay deductibles, coinsurance, and other expenses that aren’t ordinarily covered by Medicare. We’re here to help you understand the different types of MSPs. Below, we explain who is eligible for these programs and how to get the assistance you need to pay for your Medicare.
How many types of MSPs are there?
There are four kinds of MSPs. Each type of MSP is tailored to different needs and circumstances. Qualified Medicare Beneficiary (QMB) Programs pay most of your out-of-pocket costs. These costs include deductibles, copays, coinsurance, and Part B premiums. A QMB will also pay the premium for Part A if you haven’t worked 40 quarters.
What is QI in Medicare?
Qualifying Individual (QI) Programs are also known as additional Low-Income Medicare Beneficiary (ALMB) programs. They offer the same benefit of paying the Part B premium, as does the SLMB program, but you can qualify with a higher income. Those who qualify are also automatically eligible for Extra Help.
Does Medicare savers have a penalty?
Also, those that qualify for a Medicare Savings Program may not be subject to a Part D or Part B penalty. Although, this depends on your level of extra help and the state you reside in. Call the number above today to get rate quotes for your area.
1. Qualified Medicare Beneficiary (QMB)
Designed for people with an annual income less than 100% of the Federal Poverty Level (FPL) and resources under $7,860 if single or $11,800 if married. This program will cover Medicare premiums (Part A and possibly Part B), deductibles as well as copayments and/or coinsurance.
2. Specified Low-Income Beneficiary (SLMB)
Designed for seniors/adults with disabilities and an annual income between 100-120% FPL and resources under $7,860 if single or $11,800 if married. If eligible, SLMB will cover the Medicare Part B premium ($148.50 in 2021).
3. Qualifying Individual (QI)
A limited program (sponsored by block-grants to states) available on a first-come, first-serve basis. People with Medicare may qualify with an annual income between 120-135% FPL and resources under $7,860 if single or $11,800 if married. This program may also cover the Medicare Part B premium.
4. Qualified Disabled Working Individual (QDWI)
A program for adults under age 65 and disabled who have recently returned to work but are no longer eligible for premium-free Part A. People may qualify with an annual income at or below 200% FPL with resources under $4,000 if single or $6,000 if married.
Medicare Savings Program Advantages
Seniors and younger adults with disabilities who do not qualify for Medicaid may enroll in a Medicare Savings Program.
How can I connect with a trustworthy Medicare broker to learn more about Medicare Savings Programs?
Learn more and connect with a licensed Medicare broker that meets NCOA’s Standards of Excellence. These broker options are committed to serving your Medicare selection needs and priorities, including understanding the Medicare Savings Programs options available to you, at no cost to you.
Get Expert Help with Your Medicare Plan
What best describes you? I’m eligible for Medicare (I’m age 65 or older or I have a disability) I’m approaching eligibility I’m a caregiver for an older adult I’d like more Medicare information
Who funds Medicare savings programs?
These four Medicare savings programs are funded by the federal government but operated by Medicaid in each state:
What can Medicare save you?
Medicare savings programs can help you pay Part A and Part B premiums, deductibles, copays, and coinsurance.
Why were Medicare and Coinsurance created?
These programs were created because not everyone reaches retirement age with the same ability to handle expenses like Medicare premiums, copays, coinsurance, deductibles, and the cost of prescription drugs.
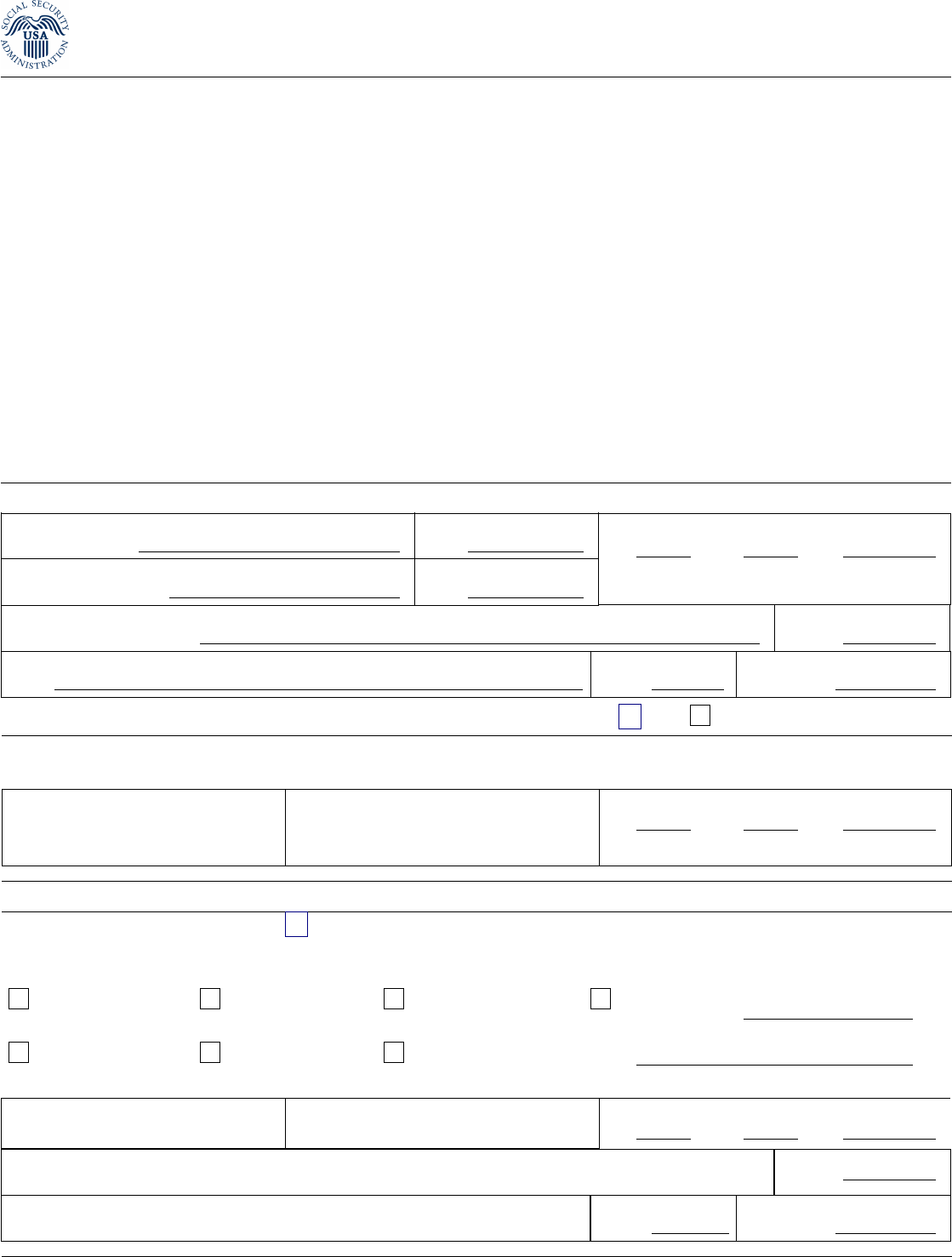
What documents are needed to apply for Medicare?
Before you begin applying, gather supporting documents such as your Social Security and Medicare cards, proof of your address and citizenship, bank statements, IRA or 401k statements, tax returns, Social Security awards statements, and Medicare notices.
How to apply for medicaid?
To apply for the a program, you’ll need to contact your state Medicaid office. You can check online to find your state’s office locations, or call Medicare at 800-MEDICARE. Once you submit your application, you should receive a confirmation or denial within about 45 days. If you’re denied, you can request an appeal.
Can you bill Medicare for QMB?
Other facts to know about Medicare savings programs. Healthcare providers may not bill you. If you are in the QMB program, your healthcare providers aren’ t allowed to bill you for the care you receive — Medicaid will pay them directly. If you are wrongly billed for a healthcare service, make sure the doctor knows you’re in the QMB program.
Does the program for all inclusive care for the elderly require a nursing home?
The Program for All-inclusive Care for the Elderly (PACE) can get you the medical care you need at a PACE center in your area, in your home, or in your community, so you don’t have to go to a nursing home.
What is Medicare Part A?
Entitled to Medicare Part A, eligible for Medicaid under mandatory or optional pathway in addition to MSP, and qualify for Medicaid payment of: •Medicare Part B premiums. •At state option, certain premiums charged by Medicare Advantage plans. •Medicare deductibles, coinsurance, and copayments (except nominal copayments in Part D);
What are the different types of MSPs?
There are four types of MSPs, with the level of assistance varying by income and whether the beneficiary is eligible for full or partial Medicaid benefits (Table 1). TABLE 1. Medicare Savings Programs as of October 2019. Type. Full or partial Medicaid benefits.
How many people were enrolled in Medicaid in 2013?
Enrollment was primarily concentrated in the Qualified Medicare Beneficiary (QMB) program with about 7 million individuals enrolled.
Does Medicaid cover cost sharing?
Medicaid policies for covering Medicare cost sharing have modest but statistically significant effects on access to care. MACPAC’s analysis found that paying a higher percentage of Medicare cost sharing increases dually eligible beneficiaries’ likelihood, relative to that of non-dually eligible Medicare beneficiaries, of using selected Medicare outpatient services and decreases the use of safety net provider services. For more information, see Effects of Medicaid Coverage of Medicare Cost Sharing on Access to Care from our March 2015 report to Congress.
Do states have to pay for Medicare?
States are not obligated to pay the full amount of Medicare cost sharing if the provider payment would exceed the state’s Medicaid rate for the same service. States have the option to pay, for a given Medicare service received by a dually eligible beneficiary, the lesser of (1) the full amount of Medicare deductibles and coinsurance or (2) the amount by which Medicaid’s rate for the same service exceeds what Medicare has already paid. MACPAC’s analysis of state policies has documented that more than 30 states are using the lesser of option. For a state-by-state compendium of Medicaid payment policies for Medicare cost sharing, see MACPAC’s State Medicaid Payment Policies for Medicare Cost Sharing.
What is the MSP program?
Medicare Savings Program (MSP) The Medicare Savings Program (MSP) is a Medicaid-administered program that can assist people with limited income in paying for their Medicare premiums. Depending on your income, the MSP may also pay for other cost-sharing expenses.
What is a QMB on Social Security?
If qualified, you will no longer have this premium amount deducted from your Social Security benefit. Qualified Medicare Beneficiary ( QMB): Pays for Medicare Part A premium for people who do not have enough work history to get premium free Part A. QMB also pays the Part B premium, deductibles and coinsurances.
What is the PACE program?
PACE. PACE (Program of All-inclusive Care for the Elderly) is a Medicare/Medicaid program that helps people meet health care needs in the community.
What is SSI benefits?
A monthly benefit paid by Social Security. SSI is for people with limited income and resources who are disabled, blind, or age 65 or older. SSI benefits aren't the same as Social Security retirement or disability benefits.
