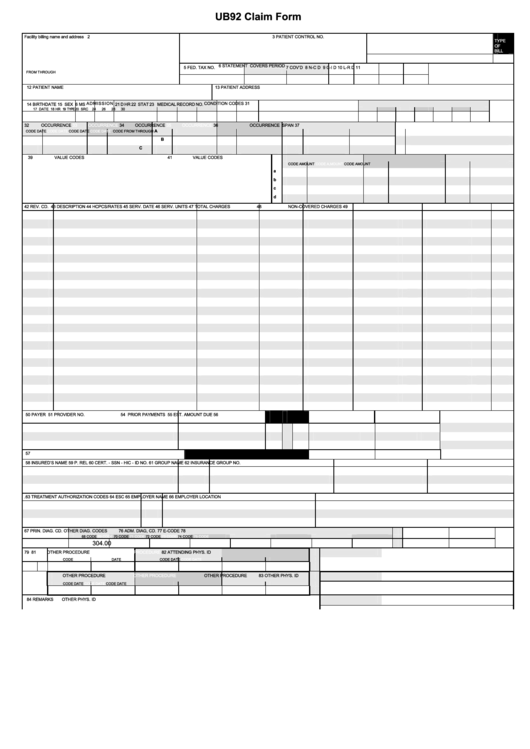
What are the Medicare condition codes UB 04?
Medicare Condition Codes UB 04 CC Codes Description of CC D0 Changes to service dates (When only chan ... D1 Use when changes to charges D2 Use when changes to revenue codes, HCPCs ... D3 Use when second or subsequent interim PP ... 7 more rows ...
Who can use the UB-04 form for billing medical claims?
Any institutional provider can use the UB-04 for billing medical claims. This includes: To fill out the form accurately and completely, be sure to do the following: Check with each insurance payer to determine what data is required. Ensure that all data is entered correctly and accurately in the correct fields.
What is a condition code on a Medicare bill?
Condition code only applicable on a xx8 type of bill. Use when canceling a claim for reasons other than the Medicare ID or provider number. Use when canceling a claim to repay a payment. Condition code only applicable to a xx8 type of bill.
How do I locate a service facility on a UB-04 form?
Use only the physical address for the service facility location field. Include National Provider Identifier (NPI) information where indicated. More detailed instructions can be found at www.cms.gov or www.nubc.org . There are 81 fields or lines on a UB-04. They're referred to as form locators or "FL."

What are the condition codes for Medicare?
Condition codesCondition CodeDescriptionD5Cancel to correct Medicare Beneficiary ID number or provider IDD6Cancel only to repay a duplicate or OIG overpaymentD7Change to make Medicare the secondary payerD8Change to make Medicare the primary payer7 more rows•Oct 13, 2021
What does UB-04 mean in medical terms?
uniform medical billing formThe UB-04 uniform medical billing form is the standard claim form that any institutional provider can use for the billing of inpatient or outpatient medical and mental health claims. It is a paper claim form printed with red ink on white standard paper.
What are the condition codes?
Condition CodesA – Serviceable issuable without qualification. ... B – Serviceable issuable with qualification. ... C – Serviceable priority issue. ... D – Serviceable test modification. ... E – Unserviceable limited restoration. ... F – Unserviceable reparable. ... G – Unserviceable incomplete. ... H – Unserviceable condemned.More items...
When would a UB-04 form be used in what setting?
The UB-04 (CMS-1450) form is the claim form for institutional facilities such as hospitals or outpatient facilities. This would include things like surgery, radiology, laboratory, or other facility services.
What are value codes on UB04?
Value CodesCodeDescriptionAddtional Description80Covered DaysEffective 03/01/07 Hardcopy UB04 Claims81Non-Covered DaysEffective 03/01/07 Hardcopy UB04 Claims82Coinsurance DaysEffective 03/01/07 Hardcopy UB04 Claims83Lifetime Reserve DaysEffective 03/01/07 Hardcopy UB04 Claims142 more rows•Sep 26, 2018
What is condition code W2 for Medicare?
By using the "W2" condition code, the hospital attests that there is no pending appeal with respect to a previously submitted Part A claim, and that any previous appeal of the Part A claim is final or binding or has been dismissed, and that no further appeals shall be filed on the Part A claim.
What does condition code 47 mean?
Partial Episode Payment The receiving HHA is required to submit a NOA with condition code 47 to indicate a transfer of care when an admission period may already be open for the same member at another HHA.
What is Medicare condition code 20?
Claims are billed with condition code 20 at a beneficiary's request, where the provider has already advised the beneficiary that Medicare is not likely to cover the service(s) in question.
When to use condition code xx8?
Condition code only applicable on a xx8 type of bill. Use when canceling a claim for reasons other than the Medicare ID or provider number. Use when canceling a claim to repay a payment. Condition code only applicable to a xx8 type of bill.
When is end stage renal disease covered by Medicare?
End Stage Renal Disease (ESRD) patient in the first 30 months of entitlement covered by employer group health insurance. Medicare may be a secondary insurer if the patient is also covered by an employer group health insurance during the patient's first 30 months of ESRD entitlement.
What is a denial notice for Medicare?
Billing for denial notice. Provider determined services are at a non-covered level or excluded, but it is requesting a denial notice from Medicare in order to bill Medicaid or other insurers.
When is an inpatient admission changed to an outpatient?
The change in patient status from inpatient to outpatient is made prior to discharge or release while the patient is still a patient of the hospital.
Is a non-PPS bill reported by providers?
Non-PPS bill not reported by providers. MAC records this from system for non-PPS hospital bills.
What is UB-04?
This form, also known as the UB-04, is a uniform institutional provider bill suitable for use in billing multiple third party payers. Because it serves many payers, a particular payer may not need some data elements. The National Uniform Billing Committee (NUBC) maintains lists of approved coding for the form. All items on Form CMS-1450 are described. The FI must be able to capture all NUBC-approved input data described in section 75 (of the Medicare Claims Processing Manual Chapter 25) for audit trail purposes and be able to pass all data to other payers with whom it has a coordination of benefits agreement.
Who is the author of the AHA coding handbook?
The handbook is authored by Nelly Leon-Chisen, RHIA , Director of Coding and Classification at the AHA.
What is the type of bill for a 36, 37, 38, 39?
c. If codes 36, 37, 38, or 39 are entered, the type of bill must be 11X and the provider must be a non-PPS hospital or exempt unit.
What code must be accompanied by dates?
c. Code must be accompanied by dates.
What is 79 code?
n. Code 79 is for payer use only. Providers do not report this code.
What is the VC code for conditional payment?
Accident/Medical Payment Coverage – Date of accident/injury for which there is medical payment coverage. Reported with VC 14 or VC 47. If filing for a Conditional Payment, report with Occurrence Code 24.
What is the VC code for accident related to employment?
Accident/Employment-Related - Date of an accident/injury related to beneficiary's employment. Reported with VC 15 or VC 41. If filing for a Conditional Payment, report with Occurrence Code 24.
What is the primary payer code for Medicare Part A?
Beneficiary must have Medicare Part A entitlement (enrolled in Part A) for this provision to apply. Primary Payer Code = G.
What is primary payer code?
Primary Payer Codes Primary Payer codes are not reported by the provider via electronic submission of a MSP claim. Primary Payer codes are applied to the claim upon transfer to the Fiscal Intermediary Standard System (FISS) based on the corresponding electronic data reported. Primary Payer Codes of A to L (except C) must match MSP VC reported on claim. For example, MSP VC 12 = Primary Payer Code A, etc.
What is a date of denied insurance?
Date Insurance denied - Date of receipt of a denial of coverage by a higher priority payer. This could be date of primary payer's Explanation of Benefit (EOB) statement, letter or other documentation. Date is required on all Conditional Payment claims.
What is the code for no fault insurance?
Reported with VC 14 or 47. If filing for a Conditional Payment, report with Occurrence Code 24.
Is EGHP secondary to Medicare?
To navigate directly to a particular type of code, click on the type of code from the following list: Beneficiary's and/or spouse's EGHP is secondary to Medicare. Beneficiary and/or spouse are employed and there is an EGHP that covers beneficiary but either:
What is UB-04 form?
The UB-04 uniform medical billing form is the standard claim form that any institutional provider can use for the billing of inpatient or outpatient medical and mental health claims. It is a paper claim form printed with red ink on white standard paper. Although developed by the Centers for Medicare ...
What is UB-04?
The UB-04 uniform medical billing form is the standard claim form that any institutional provider can use for the billing of inpatient or outpatient medical and mental health claims. It is a paper claim form printed with red ink on white standard paper. Although developed by the Centers for Medicare and Medicaid Services (CMS), the form has become the standard form used by all insurance carriers. 1
What is NUBC billing?
The National United Billing Committee (NUBC) is a voluntary and multidisciplinary committee that develops data elements for claims and transactions. The NUBC is responsible for the design and printing of the UB-04 form. 1.
How many fields are there on a UB-04?
There are 81 fields or lines on a UB-04. They're referred to as form locators or "FL.". Each form locator has a unique purpose: Form locator 1: Billing provider name, street address, city, state, zip, telephone, fax, and country code.
What is the difference between UB-04 and CMS 1500?
What is the difference between the UB-04 and the CMS 1500 forms? The UB-04 form is used by institutional providers, such as nursing homes and hospitals, while the CMS-1500 form is the standard claim form used by a non-institutional provider or supplier, such as a physician or a provider of durable medical equipment. 2.
How many occurrences are in Form 18-28?
Form locator 18-28: Condition codes using the two-digit codes from the NUBC manual for up to 11 occurrences.