Medicare Guidelines
- Medical Necessity / Diagnosis Codes. ...
- Tests Covered by the Local Coverage Determinations (LCD):
- Tests Covered by Medicare on a Defined Frequency
- Screening Pap Smears:
- Screening Fecal Occult Blood Tests: Medicare covers fecal occult blood tests on asymptomatic patients once every 12 months for individuals who have attained age 50.
What does medically necessary mean in Medicare?
Medicare, for example, defines medically necessary as: “Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice.” Medical necessity refers to a decision by your health plan that your treatment, test, or procedure is necessary for your health or to treat a diagnosed medical problem.
How to determine medical necessity?
satisfies the plan’s requirements for medical necessity. This can be done by reviewing the Letter of Medical Necessity, medical records, and the plan’s medical policies for coverage. A “concurrent review” occurs during the treatment to decide if the ongoing treatment is medically necessary.
How to meet medical necessity requirements?
TMHP begins the medical necessity review process upon receiving an MDS assessment and the Long-Term Care Medicaid Information Section from a Medicaid contracted nursing facility. In order for “medical necessity” to exist, TMHP must determine that the person meets the conditions set forth below: 1.
What is considered medically necessary?
“Medically necessary” is a standard that Medicare uses when deciding whether to cover a health-care service or item. This applies to everything from flu shots and preventive screenings, to kidney dialysis and wheelchairs.

What will qualify as a medical necessity?
"Medically Necessary" or "Medical Necessity" means health care services that a physician, exercising prudent clinical judgment, would provide to a patient. The service must be: For the purpose of evaluating, diagnosing, or treating an illness, injury, disease, or its symptoms.
How do I know if Medicare has medical necessity?
Determining Medical Necessity No one wants to hear that a service is “not medically necessary.” To find out if Medicare covers what you need, talk to your doctor or other health care provider about why certain services or supplies are necessary, and ask if Medicare will cover them.
How does Medicare define reasonable and necessary?
"Reasonable and Necessary" Furnished in a setting appropriate to the patient's medical needs and condition; Ordered and furnished by qualified personnel; Meets, but does not exceed, the patient's medical need; and. Is at least as beneficial as an existing and available medically appropriate alternative; or.
What is an example of medical necessity?
The most common example is a cosmetic procedure, such as the injection of medications, such as Botox, to decrease facial wrinkles or tummy-tuck surgery. Many health insurance companies also will not cover procedures that they determine to be experimental or not proven to work.
What are the four factors of medical necessity?
Medicare defines “medically necessary” as health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
What is not medically necessary?
“Not Medically Necessary” is the term applied to health care services that a physician, exercising prudent. clinical judgment, would provide to a patient for the purpose of preventing, evaluating, diagnosing or.
What are NCD guidelines?
A national coverage determination (NCD) is a United States nationwide determination of whether Medicare will pay for an item or service. It is a form of utilization management and forms a medical guideline on treatment.
What are LCD and NCD guidelines?
When a contractor or fiscal intermediary makes a ruling as to whether a service or item can be reimbursed, it is known as a local coverage determination (LCD). When CMS makes a decision in response to a direct request as to whether a service or item may be covered, it's known as a national coverage determination (NCD).
What does reasonable and necessary mean?
CMS finalized that an item or service would be considered ''reasonable and necessary'' if it is. safe and effective; not experimental or investigational; and. appropriate for Medicare patients, including the duration and frequency that is considered appropriate for the item or service, in terms of whether it is—
What factor is medical necessity based on?
Medical necessity is based on “evidence based clinical standards of care”. This means that there is evidence to support a course of treatment based on a set of symptoms or other diagnostic results. Not all diagnoses for all procedures are considered medically necessary.
Which of the following services is most likely to be considered medically necessary?
Rev Cycle FinalQuestionAnswerWhich of the following services is most likely to be considered medically necessary?Standard of care for health conditionAll of the following sets represent criteria for medical necessity and utilization review except:Federal register index and ratings183 more rows
How do you get a letter of medical necessity?
A patient can write the letter, but it needs to be made official by a doctor. Any arguments for any service ultimately have to come from a treating physician. That means the doctor needs to know you, have some history with you, and in the end either write or 'sign off on' the letter.
What is medically necessary?
According to HealthCare.gov, medically necessary services are defined as “health care services or supplies that are needed to diagnose or treat an illness, injury, condition, disease, or its symptoms – and that meet accepted standards of medicine.”.
What are some services not considered medically necessary?
According to CMS, some services not considered medically necessary may include: Services given in a hospital that, based on the beneficiary’s condition, could have been furnished in a lower-cost setting. Hospital services that exceed Medicare length of stay limitations.
What are the services that exceed Medicare length of stay limits?
Hospital services that exceed Medicare length of stay limitations. Evaluation and management services that exceed those considered medically reasonable and necessary. Therapy or diagnostic procedures that exceed Medicare usage limits. Screening tests, examinations, and therapies for which the beneficiary has no symptoms or documented conditions, ...
How to find out if Medicare covers what you need?
To find out if Medicare covers what you need, talk to your doctor or other health care provider about why certain services or supplies are necessary, and ask if Medicare will cover them.
Does Medicare cover medical supplies?
The Medicare program covers many services and supplies that are needed to diagnose or treat medical conditions. Most beneficiaries do not have problems receiving covered services and treatments they need for their health. However, it is important to understand the types of services and supplies that are considered “not medically reasonable ...
What is medical necessity?
The healthcare landscape requires providers to not only establish medical necessity, but also to clinically validate it. This requires the right documentation, processes, and procedures.
When discussing medical necessity denials or potential denials with a clinician, what is the medical necessity criteria?
When discussing medical necessity denials or potential denials with a clinician, present the medical necessity criteria the payer used to make the determination. This will prevent the debate of why non-clinical personnel can tell a provider a service is not medically necessary.
What does ABN mean in Medicare?
If a provider feels a service is medically necessary for a Medicare patient and, upon policy review, the payer denies medically necessity, an ABN will protect the provider from loss of revenue. The patient should be given the ABN form to complete in its entirety and sign prior to having the service rendered.
Why is medical necessity important?
“Medical necessity” is an important concept for medical coders and auditors to understand. Health insurance companies (payers) use criteria to determine whether items or services provided to their beneficiaries or members are medically necessary.
Why is it important for the physician, coder, biller, and insurance company to all be on the same answer
It is important for the physician, coder, biller, and insurance company to all be on the same page when it comes to medical necessity. A provider may feel specific procedures or tests are medically necessary for a patient, but the insurance company can also make that determination based on their clinical policies.
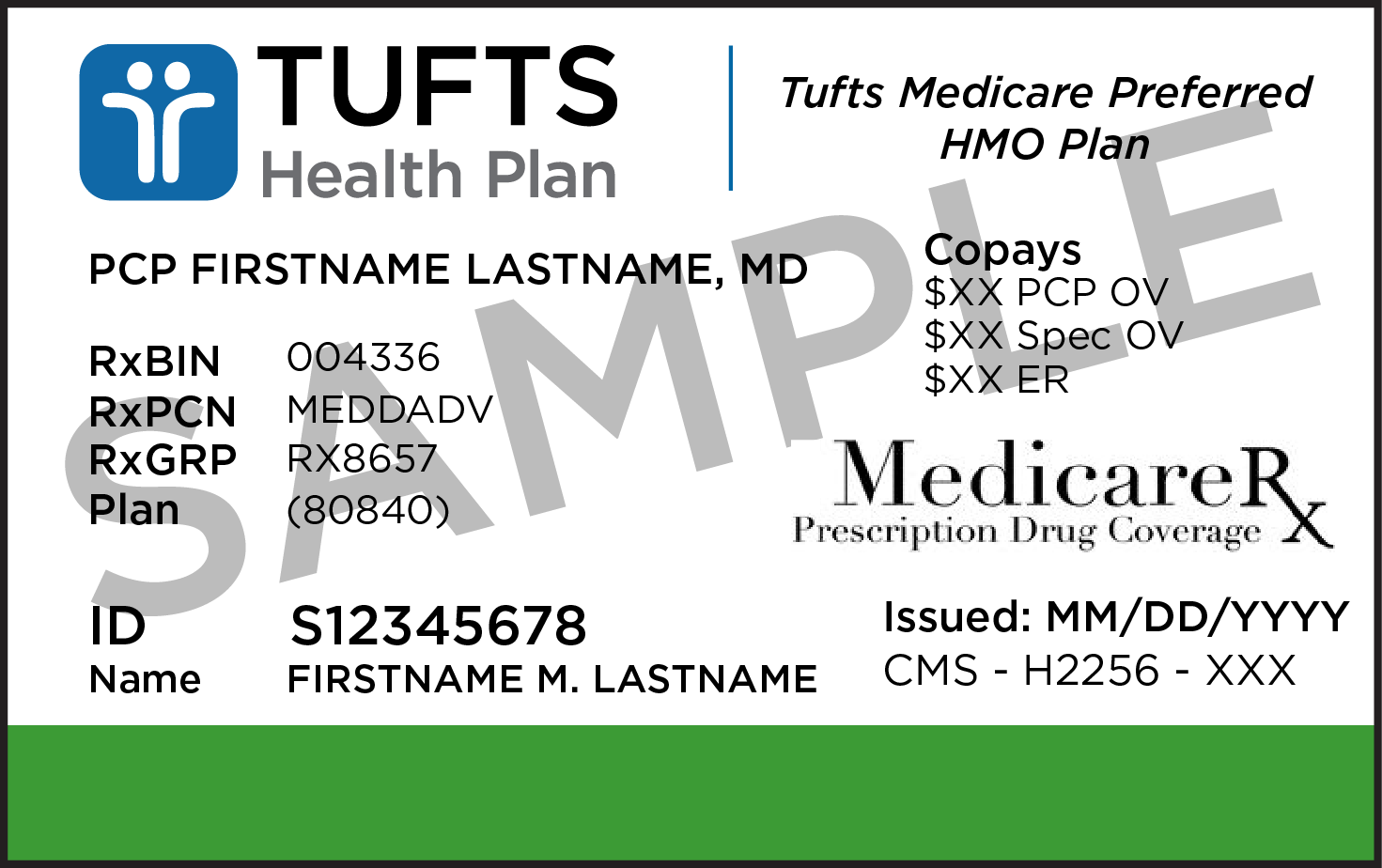
What is billing provider for Medicare?
For Medicare patients, billing providers should refer to local and national coverage determinations for medical necessity criteria. Commercial insurances may also have their own policies. Providers should document the patient’s progress, response to treatment, and any necessary change (s) in diagnosis or treatment.
How often are preventive services limited?
Payers often set frequency limitations on certain services. For instance, preventive services are generally limited to one per year. To protect the provider’s or facility’s revenue stream, due diligence must be taken to properly identify any coverage limitations ahead of the patient’s encounter.
What is medical necessity?
Medicare defines “medical necessity” as services or items reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member.
How to support medical necessity for services reported?
To better support medical necessity for services reported, you should apply the following principles: 1. List the principal diagnosis, condition, problem, or other reason for the medical service or procedure. 2.
What happens if a provider knows that a claim is not medically necessary?
If a pattern of such claims can be established, and the provider knows or should know that the services reported were not medically necessary, the provider may face monetary penalties, exclusion from Medicare program, and criminal prosecution.
Is coverage limited for medical services?
For all payors and insurance plans, even if a service is reasonable and necessary, coverage may be limited if the service is provided more frequently than allowed under a national coverage policy, a local medical policy, or a clinically accepted standard of practice.
Can a rule out statement be used for outpatient?
For office and/or outpatient services, never use a “rule-out” statement (a suspected but not confirmed diagnosis); a clerical error could permanently tag a patient with a condition that does not exist. Code symptoms, if no definitive diagnosis is yet determined, instead of using rule-out statements. 4.
Can you be denied if you are not medically necessary?
Claims for services deemed to be not medically necessary will be denied. Further, if Medicare (or any other payer) pay for services that they later determine to be not medically necessary, they may demand that those payments be refunded (with interest).
What happens if a beneficiary does not qualify for Medicare?
When a beneficiary has an effective election on file with CMS but does not have a condition that would qualify for Medicare Part A inpatient hospital or posthospital extended care services if the beneficiary were an inpatient of a hospital or a resident of a SNF that is not an RNHCI, then services furnished in an RNHCI are not covered by Medicare. A Medicare claim for services that were furnished to that beneficiary would be treated as a claim for noncovered services. If the beneficiary only needs assistance with activities of daily living, then the beneficiary's condition could not be considered as meeting the Medicare Part A requirements. Prior to submitting a claim to Medicare it is the responsibility of the RNHCI’s utilization review committee to determine that the beneficiary meets the Medicare Part A requirements.
What is an admission order for Medicare Part A?
At the time that each Medicare Part A fee-for-service patient is admitted to an IRF, a physician must generate admission orders for the patient's care. These admission orders must be retained in the patient’s medical record at the IRF.
What are nonmedical DME items?
The DME items include canes, crutches, walkers, commodes, a standard wheelchair, hospital beds, bedpans, and urinals. Those RNHCIs offering home services may order these items without a physician order and without compromising the beneficiary election for RNHCI care. The need for each item of DME ordered must be supported by the RNHCI patient’s plan of care for the home setting and the RNHCI nurses’ notes for home services. It must be noted that the benefit is applicable only to what we shall refer to as “nonmedical DME items” and does not include any of the related services provided by RNHCI staff members.
What are the exclusions for RNHCI?
The RNHCI home benefit must exclude the same services that are excluded from the home health benefit, which include: drugs and biologicals; transportation; services that would not be covered as inpatient services; housekeeping services; services covered under the End Stage Renal Disease program ; prosthetic devices; and medical social services provided to family members. These exclusions are defined at 42 CFR 409.49. Additionally, the RNHCI home benefit excludes the items or services provided by any HHA that is not an RNHCI; or any supplier, independent RNHCI nurse or aide that is working directly for a beneficiary rather than under arrangements with the RNHCI. Medicare requires a brief letter of intent from the provider in order to determine the number of RNHCIs that will be implementing the home service benefit.
What is RNHCI in Medicare?
Beneficiaries elect the RNHCI benefit if they are conscientiously opposed to accepting most medical treatment, since accepting such services would be inconsistent with their sincere religious beliefs. The Medicare home health benefit provides skilled nursing, physical therapy, occupational therapy, speech language pathology and home health aide services to eligible beneficiaries under a physician’s plan of care. The home health benefit also provides medical supplies, a covered osteoporosis drug and durable medical equipment (DME) while under a plan of care (see chapter 7).
What are non-covered services?
Medical and hospital services are sometimes required to treat a condition that arises as a result of services that are not covered because they are determined to be not reasonable and necessary or because they are excluded from coverage for other reasons. Services "related to" non-covered services (e.g., cosmetic surgery, non-covered organ transplants, non-covered artificial organ implants, etc.), including services related to follow-up care and complications of non-covered services which require treatment during a hospital stay in which the non-covered service was performed, are not covered services under Medicare. Services "not related to" non-covered services are covered under Medicare.
Is a broken leg covered by Medicare?
A beneficiary was hospitalized for a non-covered service and broke a leg while in the hospital. Services related to care of the broken leg during this stay is a clear example of "not related to" services and are covered under Medicare.
What services does a diabetic need?
Services may include: An initial nutrition and lifestyle assessment. Individual and/or group nutritional therapy services. Help managing the lifestyle factors that affect your diabetes. Follow-up visits to check on your progress in managing your diet.
Does Medicare cover nutrition therapy?
Nutrition therapy services. Medicare Part B (Medical Insurance) may cover medical nutrition therapy (MNT) services and certain related services if you have diabetes or kidney disease, or you’ve had a ki dney transplant in the last 36 months.
Determining Medical Necessity
Not Medically Necessary Services and Supplies
- The Medicare program covers many services and supplies that are needed to diagnose or treat medical conditions. Most beneficiaries do not have problems receiving covered services and treatments they need for their health. However, it is important to understand the types of services and supplies that are considered “not medically reasonable and nece...
Advance Beneficiary Notice of Noncoverage
- If you need something that is usually covered, but your doctor, health care provider, or supplier thinks that Medicare will not cover it, you will have to read and sign a notice called an “Advance Beneficiary Notice of Noncoverage” (ABN), and will serve as your acceptance that you may have to pay for the item, service, or supply.
Certificate of Medical Necessity
- A Certificate of Medical Necessity (CMN) or a DME Information Form (DIF) (also called a letter of medical necessity), is a form needed to help document the medical necessity and other coverage criteria for selected durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS). Questions about Medicare? Medicare.org’s information and resources can help make it easy to f…