What are Tier 1 medications?
Tier 1. These drugs offer the lowest co-payment and are often generic version of brand name ...
What are Tier 6 drugs?
during the forecast period. The growth of this market is majorly driven by the rising number of organ transplant procedures, the use of TDM across various therapeutic fields, the increasing preference for precision medicine, a growing focus on R&D related to TDM, and technological advancements in immunoassay instruments.
Why are there different Medicare prescription drug tiers?
What are the Medicare prescription drug tiers? There are different tiers based on cost and type of medication. Sometimes a Medicare beneficiary can choose from either a name brand or generic brand of a specific drug. Here is an example of the way the tiers are built out: Tier 1 – low copay: generic prescription drugs
What is Tier 1 Medicare?
Each tier costs a different amount. Generally, a drug in a lower tier will cost you less than a drug in a higher tier. Here's an example of a Medicare drug plan's tiers (your plan’s tiers may be different): Tier 1—lowest copayment: most generic prescription drugs; Tier 2—medium copayment: preferred, brand-name prescription drugs
What are Tier 1 Tier 2 and Tier 3 drugs?
Level or Tier 1: Low-cost generic and brand-name drugs. Level or Tier 2: Higher-cost generic and brand-name drugs. Level or Tier 3: High-cost, mostly brand-name drugs that may have generic or brand-name alternatives in Levels 1 or 2. Level or Tier 4: Highest-cost, mostly brand-name drugs.
What are the drug tiers for Medicare?
What Is a Tiered Formulary?Drug TierType of Drugs IncludedTier 1Most generic drugsTier 2Most common brand name drugs Preferred brand name drugs Some high-cost generic drugsTier 3Non-preferred brand name drugsTier 4 (Specialty Tier)Unique or very high-cost drugs
What are the 4 standardized levels of Medicare prescription drug coverage?
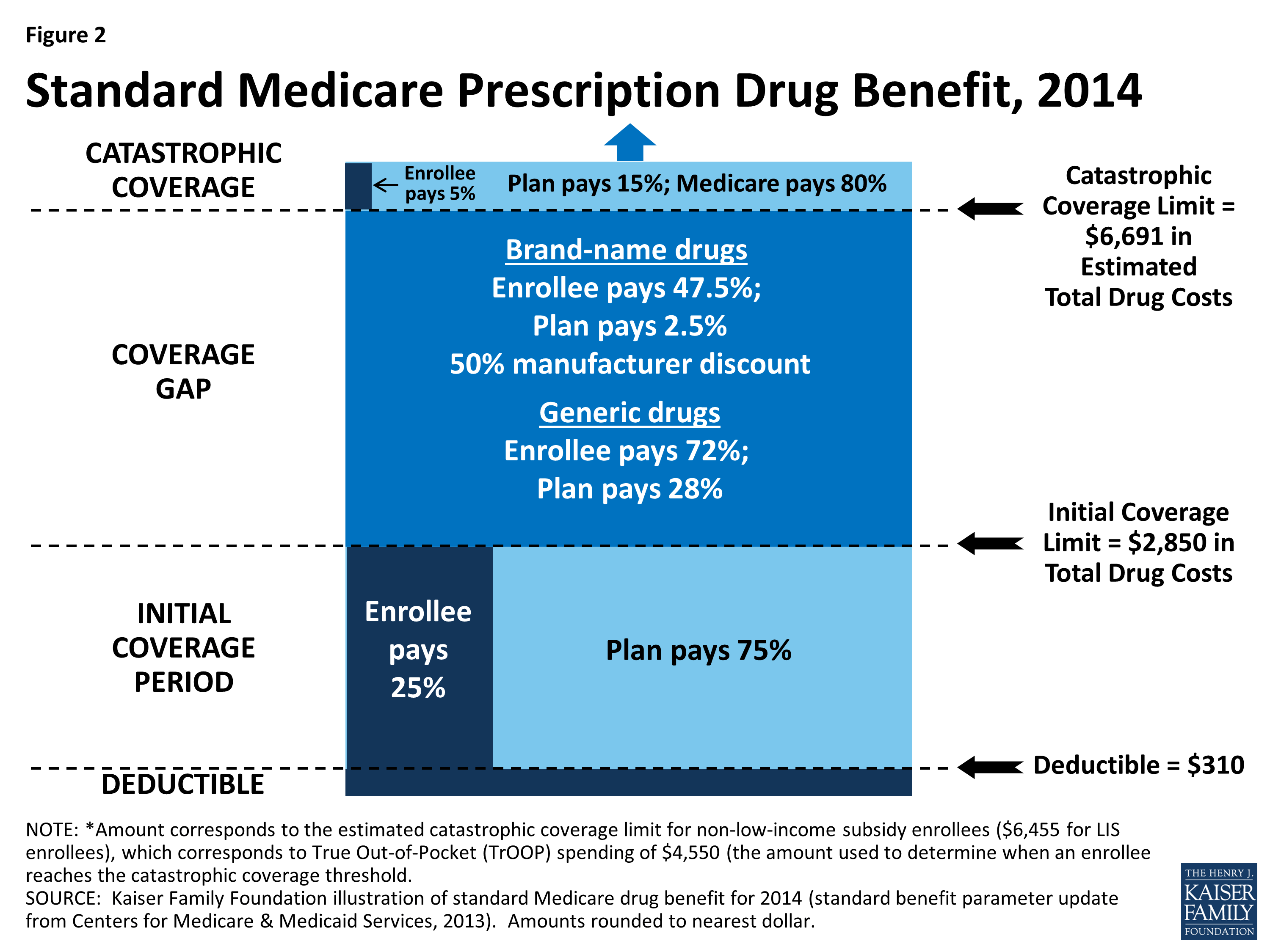
Throughout the year, your prescription drug plan costs may change depending on the coverage stage you are in. If you have a Part D plan, you move through the CMS coverage stages in this order: deductible (if applicable), initial coverage, coverage gap, and catastrophic coverage.
What are the Tier 2 drugs?
What does each drug tier mean?Drug TierWhat it meansTier 2Generic. These are also generic drugs, but they cost a little more than drugs in Tier 1.Tier 3Preferred brand. These are brand name drugs that don't have a generic equivalent. They're the lowest-cost brand name drugs on the drug list.4 more rows•Apr 27, 2020
What is a Tier 1 and Tier 2 drug?
There are typically three or four tiers: Tier 1: Least expensive drug options, often generic drugs. Tier 2: Higher price generic and lower-price brand-name drugs. Tier 3: Mainly higher price brand-name drugs. Tier 4: Highest cost prescription drugs.
What are the different drug tiers?
Understanding Drug TiersTier 1These drugs offer the lowest co-payment and are often generic version of brand name drugsTier 2These drugs offer a medium co-payment and are often brand name drugs that are usually more affordable.2 more rows•Jul 7, 2022
How many stages do Part D plans have?
four different phasesThere are four different phases—or periods—of Part D coverage: Deductible period: Until you meet your Part D deductible, you will pay the full negotiated price for your covered prescription drugs. Once you have met the deductible, the plan will begin to cover the cost of your drugs.
What is the best Part D prescription plan?
Best-rated Medicare Part D providersRankMedicare Part D providerMedicare star rating for Part D plans1Kaiser Permanente4.92UnitedHealthcare (AARP)3.93BlueCross BlueShield (Anthem)3.94Humana3.83 more rows•Mar 16, 2022
What is the max out-of-pocket for Medicare Part D?
The out-of-pocket spending threshold is increasing from $6,550 to $7,050 (equivalent to $10,690 in total drug spending in 2022, up from $10,048 in 2021).
What is the difference between Tier 1 and Tier 2 insurance?
Tier 1 usually includes a select network of providers that have agreed to provide services at a lower cost for you and your covered family members. Tier 2 provides you the option to choose a provider from the larger network of contracted PPO providers, but you may pay more out-of-pocket costs.
What tier is atorvastatin?
For example: atorvastatin is a generic, tier 1 drug with a quantity limit of 30 doses per 30 days. REPATHA is a brand-name, tier 3 drug. Before it's prescribed, you would need prior authorization from Medical Mutual to determine if it's covered.
What tier is insulin?
A large number of plans placed insulin products on Tier 3, the preferred drug tier, with a $47 copayment per prescription during the initial coverage phase; more plans used this combination of tier placement and cost-sharing requirement for coverage of insulin than any other combination in 2019 (Table 3, Table 4).
Which tier of Medicare does a drug need?
Which tier your drug needs depends on the formulary of your Medicare Part D plan. Every Medicare Prescription Drug Plan is required to have a list of covered drugs called a formulary. You can find out the drug Tier for each of your covered drugs by checking the plan’s formulary.
What are the tiers of Medicare Part D?
The Medicare Part D tiers refer to how drugs are organized in a formulary. They include both generic and brand name drugs, covered for different prices. Most commonly there are tiers 1-5, with 1 covering the lowest-cost drugs and 5 covering the most expensive specialty medications.
What is Tier 1 Medicare?
Tier 1 is the least expensive of the Medicare Part D tiers, and includes the lower-cost preferred generic drugs. Preferred drugs means a certain set of types of medications that have been approved by the insurance company to be in this low-cost grouping. Generic refers to non-name brand versions of each type of drug.
What is tier 6 insurance?
Tier 6 tends to refer to a few generic drugs for diabetes and high cholesterol available with some specific insurance plans . Tier 6 is designed to offer an affordable option for some of the most commonly needed drugs, and tend to cover only those specific drugs.
Does Medicare Part D cost more than tier 1?
Medicare Part D tiers 1 and 2 are often set up to exempt you from paying a deductible, whereas with drugs in the higher tiers you may have to pay the full drug cost until you meet the deductible, then pay a copay/coinsurance.
What are the tiers of Medicare?
Here's an example of a Medicare drug plan's tiers (your plan’s tiers may be different): Tier 1—lowest. copayment. An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug.
How many drugs does Medicare cover?
All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug. However, in most cases, a similar drug should be available.
What is formulary exception?
A formulary exception is a drug plan's decision to cover a drug that's not on its drug list or to waive a coverage rule. A tiering exception is a drug plan's decision to charge a lower amount for a drug that's on its non-preferred drug tier.
What happens if you don't use a drug on Medicare?
If you use a drug that isn’t on your plan’s drug list, you’ll have to pay full price instead of a copayment or coinsurance, unless you qualify for a formulary exception. All Medicare drug plans have negotiated to get lower prices for the drugs on their drug lists, so using those drugs will generally save you money.
How many prescription drugs are covered by Medicare?
Plans include both brand-name prescription drugs and generic drug coverage. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes. This helps make sure that people with different medical conditions can get the prescription drugs they need. All Medicare drug plans generally must cover at least 2 drugs per ...
What does Medicare Part D cover?
All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes,” like drugs to treat cancer or HIV/AIDS. A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary.
Why does Medicare change its drug list?
Your plan may change its drug list during the year because drug therapies change, new drugs are released, or new medical information becomes available.
How to find out if a drug is covered by a plan?
Since the formulary can change throughout the year, you’ll need to find out if your medicines are covered. Most plans offer an online formulary search tool. Just type in the name of the medicine and you’ll see if your plan covers it, and what tier it falls into. If you have more questions about your plan’s drug coverage, contact your member services line for help.
What is formulary based on?
The formulary is divided into levels, called “tiers.” The tiers are based on the cost of the medicine. The amount you pay each time you fill a prescription depends on the tier the medicine is in.
What is formulary in insurance?
The formulary for success. Every insurance company has a formulary, which is a list of approved medicines they will help pay for. (Remember, if your Medicare plan has a deductible, you’ll have to meet that before your plan starts helping.)
What to do if your doctor prescribes a non-preferred medicine?
If your doctor prescribes a non-preferred medicine, ask your pharmacist to work with your insurance company and doctor to find a less expensive generic or preferred alternative you can take. It will be as safe and effective at treating you, but could cost you less.
Does insurance change formulary?
Your insurance plan’s formulary will change throughout the year as medicines that offer new benefits or lower costs enter the market. Sometimes a drug may be taken off the list. While this sounds scary, it’s important to know that in most cases, a better or lower cost alternative will be added to the list in its place. If your doctor decides that you need a medication that isn’t on the list, he or she can always request authorization from your insurance company to see if you can get help from your insurance company to pay for it.
Does Medicare require a formulary?
By law, a Medicare drug formulary is required to include a certain number of options to treat specific conditions.
How many tiers are there in Medicare?
Many Medicare prescription drug plans use a four-tier system. However, since the plans are offered by private insurers, you also find five- and six-tier systems.
Which tier of prescriptions has the highest cost?
You find higher cost brand name drugs on Tier 3, and probably some specialty prescriptions. Tier 4 is where you find prescriptions with the highest cost – mostly specialty drugs.
What Is a Drug Formulary?
A drug formulary is the list of prescription drugs covered by your plan. It includes both generic and brand name medications.
How Are Drugs Priced on the Tiers?
Prescription drug pricing varies according to the insurer. However, generally speaking, you pay either a co-pay, which is a set dollar amount, or co-insurance, which is a percentage of the drug cost.
How much does a tier 1 drug cost?
For example, the drugs on Tier 1 in a four-tier system typically cost between $10 and $25. However, the Tier 1 medications on a five- or six-tier formulary are more likely to cost $3 to $5.
What restrictions does your insurance have on your coverage?
In addition to the formulary and tier pricing, your insurer may place other restrictions on coverage. The most common are step therapy and prior authorization.
How to save money on prescriptions?
The easiest way to save money on your prescriptions is to follow your plan's rules. And understanding your PDP's drug formulary, tier pricing, and other restrictions is the first step toward working within those guidelines.
What is a Medicare tier?
Medicare tiers are levels of coverage for prescription medications. The tier that a medication is assigned to determines how much you’ll pay for it. Be sure that any medication you take is included in at least one tier of a prescription plan before you enroll in it. All Medicare Part D prescription drug plans or Medicare Part C (Advantage) ...
What is the lowest tier of Medicare?
Most Medicare prescription drug plans divide the medications they cover into tiers that each cost a different amount. The lowest tier is typically the lowest cost and features generic versions of brand name medications. Generic prescription drugs are lower priced than brand name medications that no longer have a patent.
What are the most popular generics?
Some of the most commonly prescribed generic medications in the United States include:
What do you need to prove a generic drug is the same as a brand name?
For FDA approval, the producers of the generic prescription drug must prove their version is the same as the brand name medication in all aspects, including: active ingredients. concentration. form (liquid, capsule, topical, etc.) dosage.
What is the formulary for prescription drugs?
These plans can vary, however, when it comes to the list of prescription drugs they cover. This list is called a formulary, and it classifies medications into tiers.
What is generic medicine?
Generic prescription drugs are lower priced than brand name medications that no longer have a patent. Approved by the FDA, generic medications are considered as effective as their brand name counterparts.
Why do they use tiers?
They use these tiers to lower drug costs. Each tier costs a different amount. Typically, the lower tiers cost less than the higher ones.
How many tiers are there in a drug plan?
Many plans determine what the patient costs will be by putting drugs into four tiers. These tiers are determined by:
Which tier of drugs have the highest co-payment?
These drugs offer a medium co-payment and are often brand name drugs that are usually more affordable. Tier 3. These drugs have the highest co-payment and are often brand-name drugs that have a generic version available. Tier 4. These drugs are considered specialty drugs and are typically used to cover serious illness.
What is the formulary of a healthcare plan?
Under a healthcare plan, the list of covered prescription drugs is called a formulary .
What is formulary in medicine?
The formulary is usually divided into tiers or levels of coverage based on the type or usage of the medication. Each tier will have a defined out-of-pocket cost that the patient must pay before receiving the drug.
Is a drug on the formulary?
The drug you need is not on the formulary and it is the best treatment option for you. The drug needs pre-authorization, has limits, or requires step-therapy. The drug is covered but you would like it to be covered at a higher level.
How many tiers are there in MSHO?
For those in an MSHO plan, your plan has only one tier. Your copay depends on whether the drug is generic or brand-name.
What is the difference between generic and brand name drugs?
The main differences between generic and brand-name drugs are their appearance and cost. Trademark laws require generic drugs to look different from brand-name versions. Generic drugs also usually cost less than the brand-name versions.
How far in advance do you have to change your drug list?
If we plan to remove drugs from the list or plan to add restrictions, we’ll let you know at least 60 days in advance. Also, there may be times when we immediately replace a brand-name drug on our list with a new generic drug. The new generic drug will appear on the same cost-sharing tier or lower, with the same restrictions or fewer. After the change is made, we’ll provide you with information about the specific change.
Do you have to try another drug before you get covered?
For example, if Drug A and Drug B both treat your medical condition, HealthPartners may not cover Drug B until you try Drug A first. If Drug A doesn’t work for you, we would then cover Drug B.
Can you get a prescription if it is not on the drug list?
If we approve your request, your medicine will be covered even if it’s not on the drug list.
Do covered drugs have extra requirements?
Sometimes, some covered drugs may have extra requirements or limits.
Do you have to pay for a prescription drug deductible?
It depends. If your plan has a deductible, you’ll need to pay the full cost of each prescription that applies toward the deductible until the deductible is met. After that, HealthPartners will share the cost of your prescription drugs.