Does Medicare cover ciprofloxacin in the donut hole?
FREE – $1. After your deductible has been satisfied, you will enter the Post-Deductible (also called Initial Coverage) stage, where you pay your copay and your plan covers the rest of the drug cost. Copay Range. FREE – $20. In the Donut Hole (also called the Coverage Gap) stage, there is a temporary limit to what Medicare will cover for ...
What happens if I Can’t convince Medicare to pay for medication?
Copay Range. $34 – $363. In the Deductible stage, you may be responsible for the full cost of your drug. Copay Range. $13 – $363. After your deductible has been satisfied, you will enter the Post-Deductible (also called Initial Coverage) stage, where you pay your copay and your plan covers the rest of the drug cost. Copay Range.
What happens if I don’t pay my Medicare Part D-irmaa?
FREE – $1. After your deductible has been satisfied, you will enter the Post-Deductible (also called Initial Coverage) stage, where you pay your copay and your plan covers the rest of the drug cost. Copay Range. FREE – $20. In the Donut Hole (also called the Coverage Gap) stage, there is a temporary limit to what Medicare will cover for ...
What happens if I get drugs that Medicare Part B doesn’t cover?
Here are some ways that may lower the cost of your ciprofloxacin ER prescription. ... If your Medicare co-pay is higher than $57.92, you can save money by using a GoodRx coupon instead. See Prices. Lower Cost Alternative. Less expensive drugs that work the same way may be available. Learn More. Select Your Medicare Plan.
Is ciprofloxacin covered by Medicare?
Yes. 100% of Medicare prescription drug plans cover this drug.
Is Cipro covered by insurance?
Generic ciprofloxacin is covered by most Medicare and insurance plans, but some pharmacy coupons or cash prices may be lower. Compare quinolone antibiotics.
Will Medicare reimburse me for prescriptions?
Medicare Part D reimbursements Medicare Part D covers prescription drugs. Private insurance companies also administer these plans. An individual will pay a monthly insurance premium for their Part D coverage. They must purchase their prescription medications from an agreed network of pharmacies.
What drugs does Medicare not pay for?
Medicare does not cover:Drugs used to treat anorexia, weight loss, or weight gain. ... Fertility drugs.Drugs used for cosmetic purposes or hair growth. ... Drugs that are only for the relief of cold or cough symptoms.Drugs used to treat erectile dysfunction.More items...
How much does Cipro cost at CVS?
Average 12 Month Prices for Cipro (Brand) & Ciprofloxacin Hcl (Generic)PharmacyCipro Retail PriceCiprofloxacin Hcl Retail PriceCVS Pharmacy$111.73$23.41Walmart$109.90$33.22Walgreens$108.82$24.59Kroger Pharmacy$96.46$17.942 more rows
Is Cipro good for urinary tract infection?
Both Cipro and Bactrim are effective for treating UTIs. However, Cipro is not a first-choice medication for this condition, due to the risk of serious side effects. Cipro should only be used for UTIs when first-choice medications cannot be used.
How do I get Medicare to reimburse?
Start by asking the provider or supplier to file the Medicare claim on your behalf. If for some reason you need to file the claim (for example, if the provider doesn't file it by the deadline), fill out the Patient Request for Medical Payment Form (CMS-1490S). Be sure to follow the instructions on the form.
How do I claim Medicare reimbursement?
Sign in to myGov and select Medicare. If you're using the app, open it and enter your myGov pin. On your homepage, select Make a claim. Make sure you have details of the service, cost and amount paid to continue your claim.
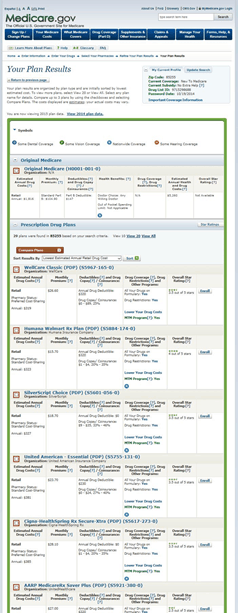
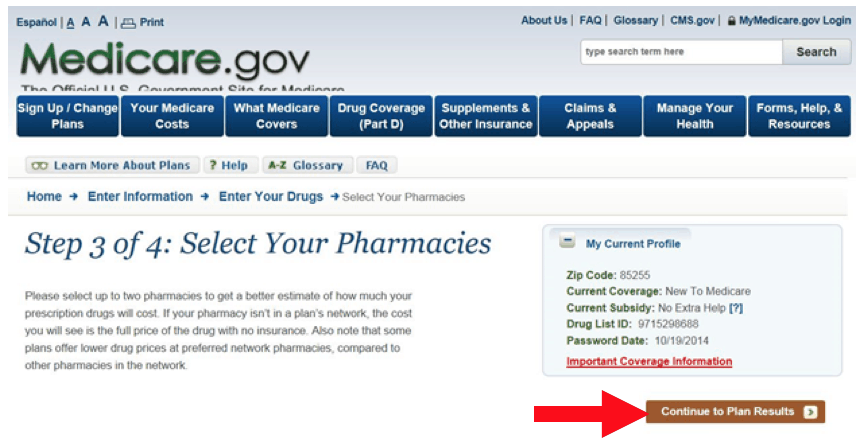
How do you find out what drugs are covered by Medicare?
Get information about specific drug plans and health plans with drug coverage in your area by visiting Medicare.gov/plan-compare or by calling 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048.
Are prescription drugs covered under a Medicare plan?
Medicare drug coverage helps pay for prescription drugs you need. Even if you don't take prescription drugs now, you should consider getting Medicare drug coverage.
What drugs are covered under Medicare Part B?
Drugs that are covered by Medicare Part B include the following.Certain Vaccines. ... Drugs That Are Used With Durable Medical Equipment. ... Certain Antigens. ... Injectable Osteoporosis Drugs. ... Erythropoiesis-Stimulating Agents. ... Oral Drugs for ESRD. ... Blood Clotting Factors. ... Immunosuppressive Drugs.More items...•
What is the best Part D drug plan for 2021?
The 5 Best Medicare Part D Providers for 2022Best in Ease of Use: Humana.Best in Broad Information: Blue Cross Blue Shield.Best for Simplicity: Aetna.Best in Number of Medications Covered: Cigna.Best in Education: AARP.
How much does Medicare cover in the donut hole?
Therefore, you may pay more for your drug. Copay Range. $7 – $363. In the Post-Donut Hole (also called Catastrophic Coverage) stage, Medicare should cover most of the cost of your drug.
What is the donut hole in Medicare?
In the Donut Hole (also called the Coverage Gap) stage, there is a temporary limit to what Medicare will cover for your drug. Therefore, you may pay more for your drug.
What is the deductible stage of a drug?
In the Deductible stage, you may be responsible for the full cost of your drug.
Does Medicare cover prescription drugs?
No. In general, Medicare prescription drug plans (Part D) do not cover this drug. Be sure to contact your specific plan to verify coverage information. A limited set of drugs administered in a doctor's office or hospital outpatient setting may be covered under Medical Insurance (Part B).
Is Medicare price accurate?
Medicare prices are provided by the Centers for Medicare and Medicaid Services (CMS). They are accurate as-of April 2020 and the information may be updated. If you encounter any issues, please let us know .
What tier is ciprofloxacin?
Tier 1. Medicare prescription drug plans typically list ciprofloxacin on Tier 1 of their formulary. Generally, the higher the tier, the more you have to pay for the medication. Most plans have 5 tiers.
Does Medicare cover donut holes?
In the Donut Hole ( also called the Coverage Gap) stage, there is a temporary limit to what Medicare will cover for your drug. Therefore, you may pay more for your drug. Copay Range. FREE – $1. In the Post-Donut Hole (also called Catastrophic Coverage) stage, Medicare should cover most of the cost of your drug.
Is Medicare price accurate?
Medicare prices are provided by the Centers for Medicare and Medicaid Services (CMS). They are accurate as-of April 2020 and the information may be updated. If you encounter any issues, please let us know .
Overview
In general, Medicare prescription drug plans (Part D) do not cover this drug. Be sure to contact your specific plan to verify coverage information. A limited set of drugs administered in a doctor's office or hospital outpatient setting may be covered under Medical Insurance (Part B).
Ways to Save on Cipro XR
Here are some ways that may lower the cost of your ciprofloxacin ER prescription.
Overview
In general, Medicare prescription drug plans (Part D) do not cover this drug. Be sure to contact your specific plan to verify coverage information. A limited set of drugs administered in a doctor's office or hospital outpatient setting may be covered under Medical Insurance (Part B).
Ways to Save on Ciprofloxacin ER
Here are some ways that may lower the cost of your ciprofloxacin ER prescription.
What happens if your medicare doesn't pay for a prescription?
Your Medicare prescription drug coverage may approve an exception if: Your doctor thinks it is medically necessary for you to get a prescription medication that isn’t on your plan’s formulary.
How much does Medicare have to be to be reviewed?
Your claim must be at least $ 1,630 in 2019 to qualify for a Federal Court Review of your Medicare drug coverage. The instructions for requesting this level of appeal are included in your decision notice from the Appeals Council.
What is the appeal process for Medicare?
If you still can’t convince the plan through which you receive your Medicare prescription drug coverage to pay for a prescription medication your doctor ordered, you can begin the appeals process. There are five levels of appeal. Level 1: Redetermination. You, your doctor, or an appointed representative can send a written request ...
How long does it take to get a redetermination from a health insurance plan?
Level 1: Redetermination. You, your doctor, or an appointed representative can send a written request for a redetermination from your plan. Your plan has 7 days to respond, or 72 hours if you ask for an expedited decision. If your plan denies coverage, you move to the next step.
Does Medicare cover prescription drugs?
If you have Medicare Part D coverage for prescription drugs, either as a stand-alone Medicare Part D Prescription Drug Plan or through a Medicare Advantage plan with Part D prescription drug coverage, your plan might cover medications your doctor believes are medically necessary for your care. Every Medicare Prescription Drug Plan has its own ...
Does Medicare cover Part D?
Medicare Part D prescription drug coverage is offered by private insurance companies authorized by Medicare, and each plan may have different coverage requirements and out-of-pocket costs. Before you fill your prescription, you might want to ask your doctor if there is a generic medication or other cheaper equivalent that he or she can prescribe to treat your condition.
Can Medicare pay for a prescription?
However, there may be times when your Medicare drug coverage refuses to pay for a certain prescription drug that your doctor determines necessary to treat your condition. Here’s what you can do if ...
How long is the Medicare Part D penalty?
Medicare Part D Penalty for Late Enrollment. All eligible Medicare beneficiaries have a seven-month Initial Enrollment Period (IEP) when they can enroll in Medicare Part A and/or Part B, as well as sign up for a Medicare Advantage Plan (Part C) and/or a Medicare Prescription Drug Plan (Part D). The IEP starts 3 months before you turn 65, includes ...
How does Medicare calculate penalty?
Medicare calculates the penalty by multiplying 1 percent of the “national base beneficiary premium” ($35.02 in 2018) times the number of full , uncovered months you didn’t have Part D or creditable coverage. The monthly premium is rounded to the nearest $.10 and added to your monthly Part D premium. The national base beneficiary premium may increase each year, so your penalty amount may also increase each year.
What is Medicare Part D?
Medicare Prescription Drug Plan (Part D): Medicare Part D, also called the Medicare prescription drug benefit, and sometimes called “PDPs” can be added to your Original Medicare (Part A and/or Part B) coverage. Medicare Prescription Drug Plans typically charge a monthly fee that varies by plan and is paid in addition to your Part B premium.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C): Medicare Advantage plans not only provide all of the same coverage as Medicare Part A (Hospital Insurance) and Medicare Part B (Medical Insurance), they also generally offer additional benefits, such as vision, dental, and hearing, and prescription drug coverage. Medicare Advantage Plans ...
How to contact Medicare.org?
Contact a Medicare.org licensed sales agent at (888) 815-3313 – TTY 711 to help you find the right Medicare coverage for your needs.
When can you change your Medicare coverage?
Each year, from October 15th – December 7th, you can make changes to parts of your Medicare coverage – which includes changes to your prescription drug coverage – during Medicare’s Annual Enrollment Period (AEP). Here’s what you can do during AEP:
Does Medicare cover prescription drugs?
Original Medicare (Part A and Part B) does not cover prescription drugs. If you want prescription drug coverage, you must join a plan run by an insurance company or other private company approved by Medicare.
What happens if you get a drug that Part B doesn't cover?
If you get drugs that Part B doesn’t cover in a hospital outpatient setting, you pay 100% for the drugs, unless you have Medicare drug coverage (Part D) or other drug coverage. In that case, what you pay depends on whether your drug plan covers the drug, and whether the hospital is in your plan’s network. Contact your plan to find out ...
How long does Medicare cover ESRD?
If you're entitled to Medicare only because of ESRD, your Medicare coverage ends 36 months after the month of the kidney transplant.
What is a prodrug?
A prodrug is an oral form of a drug that, when ingested, breaks down into the same active ingredient found in the injectable drug. As new oral cancer drugs become available, Part B may cover them. If Part B doesn’t cover them, Part D does.
Does Medicare pay for osteoporosis?
Injectable osteoporosis drugs: Medicare helps pay for an injectable drug if you’re a woman with osteoporosis who meets the criteria for the Medicare home health benefit and has a bone fracture that a doctor certifies was related to post-menopausal osteoporosis.
Does Medicare cover transplant drugs?
Medicare covers transplant drug therapy if Medicare helped pay for your organ transplant. Part D covers transplant drugs that Part B doesn't cover. If you have ESRD and Original Medicare, you may join a Medicare drug plan.
Does Medicare cover infusion pumps?
Drugs used with an item of durable medical equipment (DME) : Medicare covers drugs infused through DME, like an infusion pump or a nebulizer, if the drug used with the pump is reasonable and necessary.
Does Medicare pay for nutrition?
Parenteral and enteral nutrition (intravenous and tube feeding): Medicare helps pay for certain nutrients if you can’t absorb nutrition through your intestinal tract or take food by mouth.
What are some examples of medications that are not covered by Medicare?
Some examples of medications that may not be covered by Medicare include: Weight loss or weight gain medications . Medications used to treat cold or cough symptoms. Fertility medications. Vitamins and minerals (with the exception of prenatal vitamins or fluoride preparation products)
How to appeal a Medicare Part D formulary exception?
If your Medicare Part D Prescription Drug Plan or Medicare Advantage Prescription Drug plan denies your request for a formulary exception, you can file a request for redetermination, which is the first of five levels of appeal ( a new decision on the rejection) with the Medicare plan. If that decision is unfavorable as well, you can appeal the decision with an independent review entity, which is the second level of the appeals process. If you disagree with the decision made at any level of the appeals process, you can move on to the next level if it meets certain criteria established by Medicare. At each level, you’ll receive information on how to move to the next level of appeal if you disagree with the decision.
What to do if your Medicare plan is denied?
If your request for a formulary exception is denied, you may want to switch to a different Medicare Part D Prescription Drug Plan or Medicare Advantage Prescription Drug plan. Of course, before you switch plans, make sure the new Medicare plan covers the medications you need by checking the plan’s formulary.
How long does it take for Medicare to respond to an expedited formulary exception?
If you submit an expedited request, your Medicare plan must respond within 24 hours with its decision.
What is a formulary in Medicare?
A formulary is a list of prescription drugs covered by the Medicare plan. Every Medicare Prescription Drug Plan and Medicare Advantage Prescription Drug plan has one, although the specific medications included by each plan’s formulary will vary. Formularies may change at any time; you’ll be notified by your Medicare plan if necessary.
How to request a formulary exception?
A formulary exception can be granted if your doctor and/or Medicare plan determines that the prescription drug you requested is medically necessary for your health, so you will need a written statement from your doctor or health-care provider to support your case. (In some cases, your doctor can also make an oral statement to your Medicare Prescription Drug Plan or Medicare Advantage Prescription Drug plan.) Once your Medicare plan has received the statement from the prescribing physician, it will make a determination whether or not to cover the non-formulary medication. For a standard formulary exception request, your plan will make its decision and notify you within 72 hours of receiving the prescribing doctor’s statement.
How to change Medicare Advantage plan?
You can switch Medicare plans and make changes to your coverage during the Annual Election Period (AEP), which runs from October 15 to December 7 each year. During this period, you can: 1 Enroll in a Medicare Part D Prescription Drug Plan or Medicare Advantage Prescription Drug plan for the first time. 2 Switch from one Medicare Part D Prescription Drug Plan to another. 3 Disenroll from your Medicare Part D Prescription Drug Plan. 4 Switch from one Medicare Advantage Prescription Drug plan to another. 5 Disenroll from your Medicare Advantage Prescription Drug plan and go back to Original Medicare. You can then add on a stand-alone Medicare Part D Prescription Drug Plan.