Full Answer
Does Medicare cover COPD treatments?
There are many treatment options for COPD, including medication, pulmonary rehabilitation and supplemental oxygen. Medicare Part B generally covers 80 percent of all approved costs for services and oxygen. How much you pay for your medications, including inhalers, depends on your specific Medicare drug plan.
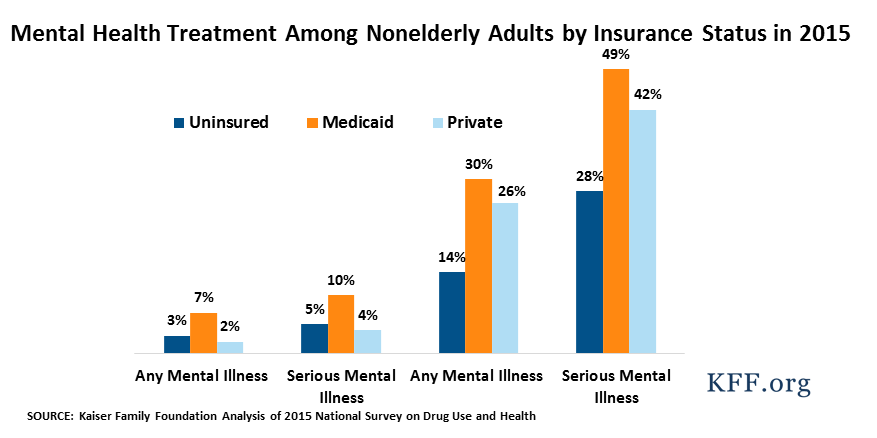
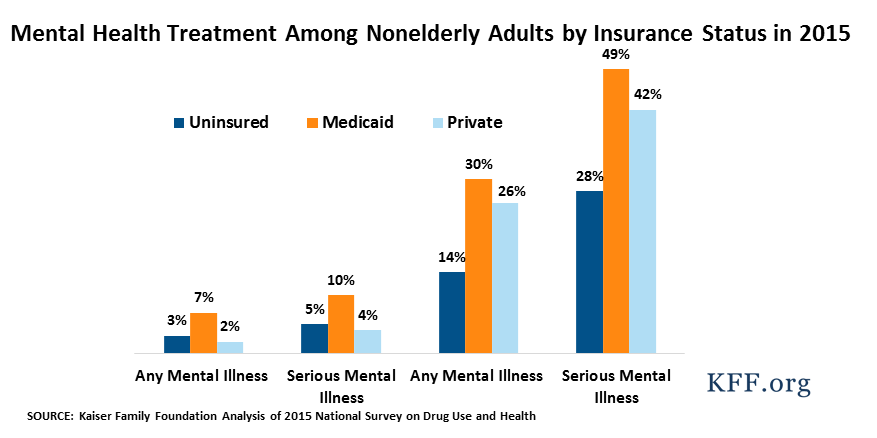
Does Medicaid cover behavioral therapy?
You may not even realize that you are eligible for mental health care, especially since Medicaid expanded under the Affordable care Act. For adults, Medicaid covers behavioral health services including addiction and recovery treatment services.
Does FMLA cover addiction treatment?
You can have FMLA cover addiction treatment as long as it is provided by a health care provider, or they can refer you to a specialized treatment provider of health care services. In order to be protected by FMLA you must provide your employer with prior notice, or else you may still face termination.
Does Medicare cover drug rehab programs?
Yes, Medicare can cover the costs of drug or alcohol detox. In fact, drug or alcohol detox generally falls under the broad category of Mental Health Services. Therefore, Medicare covers drug or alcohol rehab (in most cases). There are a few stipulations you should be aware of when using Medicare to cover the cost of detox.

Is substance use disorder considered a disability?
Are Substance Use Disorders Considered Disabilities? In short, yes. Diagnosable drug and alcohol addictions, or substance use disorders (SUDs), are considered disabilities under Section 504 of the Rehabilitation Act, the Americans with Disabilities Act (ADA), and Section 1557 of the Affordable Care Act.
Does Medicare cover opioid?
Medicare pays doctors and other providers for office-based opioid use disorder treatment, including management, care coordination, psychotherapy and counseling activities. These services, which help people recover from opioid use disorder, include: Medication (like methadone, buprenorphine, naltrexone, and naloxone)
Does Medicare cover H0020?
Providers are now required to bill Medicare as the primary payor and MaineCare as the secondary payor when billing code H0020. H0020 claims for dual eligible Medicare members will deny without an attached Explanation of Benefits (EOB).
Can substance use disorders be managed in primary care?
Most evidence-based treatments for substance use disorders can be offered as outpatient consultation in a primary care clinic. Providing such services in the context of healthcare can reduce stigma and increase patient access to appropriate treatment.
Does Medicare pay for Suboxone?
Suboxone (buprenorphine/naloxone) is not covered by original Medicare (Parts A and B). However, if you have original Medicare you can enroll in Medicare Part D for prescription drug coverage. Medicare Part D may help cover the cost of Suboxone if your doctor: indicates that it is medically necessary.
Is Tramadol covered by Medicare?
Yes. 100% of Medicare prescription drug plans cover this drug.
Does Medicare cover H0033?
H codes such as H0033 are primarily used by state Medicaid programs and may be used by commercial payers but are not reimbursable by Medicare.
What is code H2010?
HCPCS code H2010 for Comprehensive medication services, per 15 minutes as maintained by CMS falls under Other Mental Health and Community Support Services .
Does Medicare cover Narcan?
Narcan is usually covered under Medicare Part D, the prescription drug benefit. It should be noted, however, that costs and coverage vary by plan. If you have Original Medicare, you can enroll in a stand-alone Prescription Drug Plan (PDP) to get help paying for medications prescribed by your physicians.
What is the most common substance use disorder in the United States?
Alcohol use disorder is still the most common form of substance use disorder in America, fueled by widespread legal access and social approval of moderate drinking.
Is Naltrexone a pill?
Naltrexone can be prescribed and administered by any practitioner licensed to prescribe medications, and is available in a pill form for Alcohol Use disorder or as an extended-release intramuscular injectable for Alcohol and Opioid Use disorder.
Which of the following are characteristics associated with addictive behaviors?
Individuals suffering from addiction will: be unable to stop consuming a substance or end a specific behavior. display a lack of control concerning the substance, thing, or behavior they are addicted to. experience increased desires for the specific substance, thing, or behavior.
How does Medicare cover inpatient substance use treatment?
If inpatient SUD treatment is deemed reasonable and medically necessary, Medicare covers it just as they would any other hospitalization. The benef...
Does Medicare cover outpatient substance use treatment?
Medicare Part B covers some basic outpatient screening and treatment for substance use disorders. But although Medicare provides solid coverage for...
Does Medicare cover day treatment programs?
Partial hospitalization, which is also referred to as a day treatment program, is the next step up from an intensive outpatient program. Partial ho...
To what degree are residential programs for SUD covered by Medicare?
Residential programs for SUD treatment are a step above partial hospitalization but a step below inpatient care. The patient lives at the residenti...
Does Medicare Advantage cover substance use treatment?
Medicare Advantage plans are required to cover the same services that Original Medicare (ie, Parts A and B) covers, but the specifics of the covera...
How many days of hospitalization does Medicare cover?
A supplement plan can extend the number of days you have hospitalization coverage. If you get inpatient care at a psychiatric hospital, Medicare covers 190 days of lifetime care. The limit on lifetime days is a problem if you need intensive mental health services or suffer a relapse.
How many reserve days does Medicare pay for?
After the 90th day, the coinsurance amount doubles, and you begin using lifetime reserve days. Medicare only allows 60 of these during your lifetime. If you’ve been an inpatient for over 90 days and you don’t have lifetime reserve days, Medicare won’t pay for care.
What is Part B drug?
Part B covers medicines that are given to you by a doctor, meaning they can’t be self-administered. Part B outpatient drugs that treat substance abuse and addiction have different criteria. Ask your doctor any questions about treatment.
What is supplement plan?
Substance abuse treatment can be a long and challenging road, and the costs can add up. A supplement plan can make these costs manageable by picking up cost-sharing. An agent is a professional that can answer your questions and compare all options in your area.
Does Part A cover inpatient care?
Part A may cover the cost of the stay for an inpatient facility. Your doctor must write a recommendation for treatment and believe it to be necessary. You must pay Part A deductibles, copayments, or coinsurance amounts that may apply. Also, any inpatient medications for treatment may have coverage by Part A.
Does Medicare cover drug addiction?
Medicare’s substance abuse treatment coverage includes rehab for all types of drug addiction. Coverage extends to those with illegal drug addiction, alcohol addiction, and addiction to prescription drugs.
Does Part D cover methadone?
Part D covers methadone for pain, but your copay depends on your plan. Part D doesn’t cover methadone for substance abuse treatment, but Part B might.
What is covered by Medicare Advantage 2020?
Beginning January 1, 2020, original Medicare and Medicare Advantage cover treatment programs for people with opioid use disorder. The coverage includes: FDA-approved medications for the disorder. counseling. individual or group therapy. intake activities.
What is Medicare SBIRT?
This is an early intervention approach that aims to prevent a person with non-dependent substance use from developing a substance use disorder.
What is part B in a hospital?
If a person with substance use disorder needs inpatient treatment in a general or psychiatric hospital, Part A covers the care. When an individual needs outpatient treatment, Part B provides coverage. Part B coverage may include: a screening. individual or group psychotherapy.
Does Medicare cover substance abuse?
Medicare covers substance abuse treatment if a person’s doctor believes it is medically necessary, and if the services come from a Medicare-approved healthcare provider. The Medicare coverage for substance abuse is broad, as it includes a screening program and most medications, as well as inpatient and outpatient treatment.
Does Medicare cover methadone?
During a hospital stay, Part A covers the medication a doctor prescribes. Medicare may approve the use of metha done when prescribed in an inpatient setting.
Is toxicology free with Medicare?
toxicology testing. periodic evaluations. If a person has original Medicare, this program is free, except for the Part B deductible of $198. Individuals with a Medicare Advantage plan may have to pay a copayment, and it would be useful to ensure that opioid treatment provider is enrolled in Medicare.
Does Medicare cover partial hospitalization?
Medicare covers partial hospitalization, which is a form of treatment for substance use disorder. It sometimes serves as an alternative to inpatient care. The treatment consists of intense outpatient psychiatric sessions that a person receives during the daytime. The program does not require overnight stay.
Does Medicare cover Subutex?
Coverage is not limited to single entity products such as Subutex®, but must include combination products when medically necessary (for example, Suboxone®). For any new enrollees, CMS requires sponsors to have a transition policy to prevent any unintended interruptions in pharmacologic treatment with Part
Is methadone a part D drug?
Part D drug is defined, in part, as “a drug that may be dispensed only upon a prescription.” Consequently, methadone is not a Part D drug when used for treatment of opioid dependence because it cannot be dispensed for this purpose upon a prescription at a retail pharmacy. (NOTE: Methadone is a Part D drug when indicated for pain). State Medicaid Programs may continue to include the costs of methadone in their bundled payment to qualified drug treatment clinics or hospitals that dispense methadone for opioid dependence.
UnitedHealthcare Insurance for Drug and Alcohol Rehab Treatment
UnitedHealthcare (UHC) serves over 45 million people around the world and contracts directly with more than 1.2 million physicians and 6,500 hospitals and treatment facilities in the U.S. alone. 1 But how do they handle drug and alcohol ...
Aetna Insurance Coverage for Drug and Alcohol Rehab Treatment
Aetna Substance Abuse Coverage Deciding to go to a drug or alcohol addiction rehab is difficult enough without having to worry about whether your insurance covers the substance abuse treatment service. This page will help you learn more about: The ...
Does VA Insurance Cover Addiction Treatment?
If you or a loved one is a veteran living with a substance use disorder, help is available through VA insurance. Under the Affordable Care Act (ACA), all insurance plans, including VA insurance, must cover some or all of the cost of mental health ...
Kaiser Permanente Insurance for Drug and Alcohol Addiction Rehab
If you are concerned that you or your loved one needs drug or alcohol addiction rehab, the first place to start is with your primary care doctor, who can help assess your addiction treatment needs and coordinate a referral to a substance abuse ...
Blue Cross Blue Shield Insurance Coverage for Drug and Alcohol Addiction Rehab
Deciding to seek rehabilitation treatment for drug or alcohol addiction can be a step in the right direction, but you may have some concerns about treatment. Paying for treatment, rehab services and navigating rehab insurance coverage levels can be ...
Humana Health Insurance for Drug and Alcohol Addiction Rehab
Drug and Alcohol Rehab Through Humana Health Plans If you or your loved one is struggling with substance abuse and in need of drug or alcohol addiction rehab, you may feel overwhelmed by the range of choices and decisions to make about the best type ...
Getting Drug and Alcohol Rehab Without Insurance
What is Substance Abuse Rehab? Drug and alcohol addiction treatment provides professional rehabilitation services to those who struggle with chemical dependence and other substance abuse issues. Rehab centers typically offer treatment services for ...
How long does Medicare cover mental health?
Medicare covers care in specialized psychiatric hospitals that only treat mental illness when in-patient care is needed for active psychiatric treatment. As with care in a general hospital, Medicare pays for necessary in-patient hospitalization for up to 90 days per benefit period. Medicare beneficiaries who need to be in a hospital for more than 90 days are entitled to 60 lifetime reserve days which can be used only once in a life time.
What is Medicare Advantage Plan?
Medicare Advantage plans contract with Medicare and are paid a fixed amount to provide Medicare benefits.
How long can you get Medicare if you lose your Social Security?
Under this law, people who return to work, and therefore lose their Social Security disability benefits, can continue to receive Medicare coverage for 8½ years after returning to work.
What is a Medigap plan?
A Medigap plan can help beneficiaries afford costs associated with treatment for mental illness and substance use disorders. For more information on Medigap,see: https://www.medicareadvocacy.org/medicare-info/medigap/ (site visited September 22, 2015).
Does Medicare cover psychiatric nurses?
Medicare covers medically necessary diagnostic and treatment services provided by physicians, including psychiatrists, as well as clinical psychologists, social workers, psychiatric nurse specialists, nurse practitioners and physicians’ assistants. Medicare does not cover treatment by licensed professional counselors.
Can you renew Medicare for psychiatric hospitalization?
Once this maximum has been reached, Medicare coverage of psychiatric hospitalization is exhausted and cannot be renewed. This limitation can be harsh for individuals who need frequent and/or lengthy in-patient treatment in a specialized hospital.
Does Medicare pay for substance abuse treatment?
Medicare Part A pays for inpatient substance abuse treatment; individuals will pay the same co-pays as for any other type of inpatient hospitalization. Likewise, Medicare Part B will pay for outpatient substance abuse treatment services from a clinic or hospital outpatient department. Covered items and services for the treatment ...
What services does Medicare Advantage cover?
Some examples of the types of services Medicare Advantage plans may cover include: psychiatric care, such as a consultation with a psychiatrist or a prescription for anti-addiction or withdrawal medication.
What are the benefits of Medicare Advantage?
Many Medicare Advantage plans offer supplemental benefits you can't get with traditional Medicare. The specific supplemental benefits you can get depend on your plan. You may have to meet certain eligibility criteria, such as getting a referral from a doctor. Some supplemental benefits that may offer additional support to people living with addiction include: 1 complementary and holistic care, such as acupuncture and chiropractic care 2 nutrition and wellness consultations 3 in-home care 4 home meal delivery 5 telehealth services 6 transportation to and from medical care
What are the benefits of a doctor for addiction?
Some supplemental benefits that may offer additional support to people living with addiction include: complementary and holistic care, such as acupuncture and chiropractic care. nutrition and wellness consultations. in-home care.
Does Medicare cover substance abuse?
The law requires Medicare to cover substance abuse treatment when "reasonable and necessary.". Medicare Advantage may offer additional coverage. Addiction is a serious medical condition, not a moral or personal failing. Yet many people are too ashamed to seek treatment, or worry that they cannot afford it. The law requires Medicare plans ...
Does Medicare cover addiction treatment?
Medicare Advantage plans have to cover the same addiction treatment as Medicare. Many Medicare Advantage plans are health maintenance organizations (HMO), which require you to seek care from an in-network provider. This may limit the care providers from whom you can get outpatient services like therapy or inpatient services like addiction rehab.