What items are covered by Medicare?
What Part A covers. What Part B covers. What Medicare health plans cover. Preventive & screening services. What's not covered by Part A & Part B. Medicare Part A coverage–hospital …
Is there a deductible for Medicare Part A?
Medicare Part A is also called "hospital insurance," and it covers most of the cost of care when you are at a hospital or skilled nursing facility as an inpatient. Medicare Part A also covers hospice services. For most people over 65, Medicare Part A is free.
How long will Medicare pay for a hospital stay?
Medicare Part A covers hospital stays, providing invaluable assistance with potentially crippling bills for U.S. citizens age 65 and older. While people who have paid Medicare taxes through work for at least 10 years don’t have to pay a monthly premium, Medicare Part A doesn’t cover everything related to hospital stays. It’s essential to understand what’s covered and what’s not …
How much does Medicare pay for hospital stays?
Oct 14, 2021 · Medicare Part A is hospital insurance. It covers the hospital charges and certain expenses you have during a hospital stay, including meals, operating room fees, necessary medical supplies and lab tests. Medicare Part A also covers inpatient hospital care required as part of a clinical research study.

Does Medicare Part A cover hospital?
Medicare Part A will pay for most of the costs of your hospital stay, after you pay the Part A deductible. Medicare Part A is also called "hospital insurance," and it covers most of the cost of care when you are at a hospital or skilled nursing facility as an inpatient. Medicare Part A also covers hospice services.
Does Medicare Part A pay 100% of hospital?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
How much does Medicare Part A pay for hospitalization?
Part A – Hospital Insurance Premiums, Deductibles & CoinsuranceIf You HaveIn 2022, You Will Pay a Monthly Premium ofInpatient Hospital Deductible$1,556Inpatient Hospital Coinsurance$389 per day for days 61–90 $778 per day for days 91-150Skilled Nursing Facility Coinsurance$194.50 per day for days 21-1003 more rows
What services are covered under Medicare Part A?
In general, Part A covers:Inpatient care in a hospital.Skilled nursing facility care.Nursing home care (inpatient care in a skilled nursing facility that's not custodial or long-term care)Hospice care.Home health care.
What is not covered under Medicare Part A?
Part A does not cover the following: A private room in the hospital or a skilled nursing facility, unless medically necessary. Private nursing care.
What is Medicare Part A deductible for 2021?
Medicare Part A Premiums/Deductibles The Medicare Part A inpatient hospital deductible that beneficiaries will pay when admitted to the hospital will be $1,484 in 2021, an increase of $76 from $1,408 in 2020.Nov 6, 2020
Does Medicare Part A cover emergency room visits?
Does Medicare Part A Cover Emergency Room Visits? Medicare Part A is sometimes called “hospital insurance,” but it only covers the costs of an emergency room (ER) visit if you're admitted to the hospital to treat the illness or injury that brought you to the ER.
What is Medicare Part A and B mean?
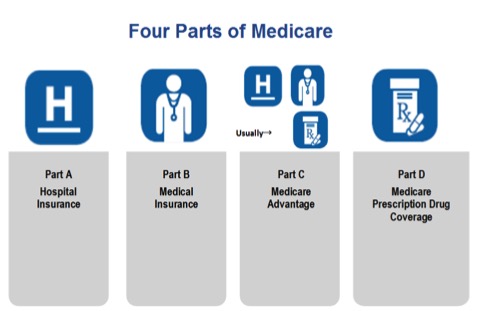
Part A provides inpatient/hospital coverage. Part B provides outpatient/medical coverage. Part C offers an alternate way to receive your Medicare benefits (see below for more information). Part D provides prescription drug coverage.
What do Medicare Parts A and B cover?
Part A (Hospital Insurance): Helps cover inpatient care in hospitals, skilled nursing facility care, hospice care, and home health care. Part B (Medical Insurance): Helps cover: Services from doctors and other health care providers.
Is Medicare Part A free?
Medicare Part A (Hospital Insurance) Most people get Part A for free, but some have to pay a premium for this coverage. To be eligible for premium-free Part A, an individual must be entitled to receive Medicare based on their own earnings or those of a spouse, parent, or child.Dec 1, 2021
What does Medicare Part A cover in 2022?
Medicare Part A covers inpatient hospital, skilled nursing facility, hospice, inpatient rehabilitation, and some home health care services. About 99 percent of Medicare beneficiaries do not have a Part A premium since they have at least 40 quarters of Medicare-covered employment.Nov 12, 2021
What Medicare Part A Covers
When you are admitted to a hospital or skilled nursing facility, Medicare Part A hospital insurance will cover the following for a certain amount o...
What Medicare Part A Does Not Cover
Medicare Part A hospital insurance does not cover:• personal convenience items such as television, radio, or telephone• private duty nurses, or• a...
How Much Medicare Pays For You to Stay in A Hospital
Medicare Part A pays only certain amounts of a hospital bill for any one spell of illness. (And for each spell of illness, you must pay a deductibl...
What Constitutes One Spell of Illness
A spell of illness, called a "benefit period," refers to the time you are treated in a hospital or skilled nursing facility, or some combination of...
Skilled Nursing Facilities and Home Health Care
Under some circumstances, Medicare will cover some of the cost of inpatient treatment in a skilled nursing facility or visits from a home health ca...
What is Covered Under Medicare A?
Medicare Part A is commonly referred to as “hospital insurance” because its primary function is to help older adults manage the cost of hospital bi...
What is Not Covered Under Medicare Part A?
Even in the case of an inpatient stay that Medicare Part A covers, Part A won’t cover:
Does Medicare Part A Cover Doctor Visits?
Part A covers qualifying hospital visits; Part B, rather than Part A, covers doctors’ services at the hospital, much like Part B covers non-emergen...
Does Medicare Part A Cover 100 Percent?
For a qualifying inpatient stay, Medicare Part A covers 100 percent of hospital-specific costs for the first 60 days of the stay — after you pay th...
What Does Medicare Part A Cost?
Most people don’t have to pay a monthly premium for Part A. If you or your spouse have worked 40 quarters (10 years) while paying Medicare taxes, y...
How to Enroll in Medicare Part A?
If you believe you would benefit from Part A coverage and qualify for it, the final step is the Part A enrollment process. If you are near the Medi...
Do you need Medicare Part A for hospital coverage?
If you, like most people, don’t have to pay a monthly premium for Part A, there is no downside to enrolling when you become eligible at age 65. You...
Do you need more than Part A for hospital coverage?
While Part A covers a significant portion of a typical hospital bill and usually provides coverage for U.S. citizens age 65 and older without a mon...
What is unique about Medicare Advantage when it comes to hospital coverage?
Medicare Advantage plans protect you with an annual out-of-pocket maximum — a dollar amount specific to your plan that defines the most money you w...
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
Is Medicare Advantage the same as Original Medicare?
What's covered? Note. If you're in a Medicare Advantage Plan or other Medicare plan, your plan may have different rules. But, your plan must give you at least the same coverage as Original Medicare. Some services may only be covered in certain settings or for patients with certain conditions.
What is Medicare Part A?
Medicare Part A is also called "hospital insurance," and it covers most of the cost of care when you are at a hospital or skilled nursing facility as an inpatient. Medicare Part A also covers hospice services. For most people over 65, Medicare Part A is free. The following list gives you an idea of what Medicare Part A pays for, ...
How much does Medicare pay for hospital bills?
Medicare Part A pays only certain amounts of a hospital bill for any one spell of illness. (And for each spell of illness, you must pay a deductible before Medicare will pay anything. In 2020, the hospital insurance deductible is $1,408.)
How many days can you use Medicare lifetime reserve?
If you are in the hospital more than 90 days during one spell of illness, you can use up to 60 additional "lifetime reserve" days of coverage. During those days, you are responsible for a daily coinsurance payment of $704 per day in 2020. Medicare pays the rest of covered costs.
How long does a skilled nursing home stay in the hospital?
Your skilled nursing stay or home health care must begin within 30 days of being discharged.
How long does Medicare cover psychiatric hospitals?
Psychiatric Hospitals. Medicare Part A hospital insurance covers a total of 190 days in a lifetime for inpatient care in a specialty psychiatric hospital (meaning one that accepts patients only for mental health care, not just a general hospital). If you are already an inpatient in a specialty psychiatric hospital when your Medicare coverage goes ...
How many reserve days do you have to use for Medicare?
You do not have to use your reserve days in one spell of illness; you can split them up and use them over several benefit periods. But you have a total of only 60 reserve days in your lifetime. (Note: If you have a Medicare Advantage Plan, called Medicare Part C, you may not have to pay ...
Does Medicare cover skilled nursing?
Skilled Nursing Facilities and Home Health Care. Under some circumstances, Medicare will cover some of the cost of inpatient treatment in a skilled nursing facility or visits from a home health care agency. Your stay in a skilled nursing home facility or home health care is covered by Medicare Part A only if you have spent three consecutive days, ...
What is Medicare Part A?
Medicare Part A#N#Medicare Part A, also called "hospital insurance ," covers the care you receive while admitted to the hospital, skilled nursing facility, or other inpatient services. Medicare Part A is part of Original Medicare.#N#provides coverage to U.S. citizens age 65 and older for inpatient stays in hospitals and similar medical facilities.
How much does Medicare cover inpatients?
Does Medicare Part A Cover 100 Percent? For a qualifying inpatient stay, Medicare Part A covers 100 percent of hospital-specific costs for the first 60 days of the stay — after you pay the deductible for that benefit period.
What is Medicare Original?
Original Medicare is a fee-for-service health insurance program available to Americans aged 65 and older and some individuals with disabilities. Original Medicare is provided by the federal government and is made up of two parts: Part A (hospital insurance) and Part B (medical insurance). or other medical insurance may provide coverage.
How long does it take to pay coinsurance for Medicare?
After 60 days , you must pay coinsurance that Part A doesn’t cover. For hospital expenses covered by Part B, you have to pay 20 percent coinsurance after meeting your annual deductible. Part A and B are collectively known as Original Medicare and work hand-in-hand to help cover hospital stays.
How long does Medicare Part A and Part B last?
Your IEP begins three months before the month you turn 65. The IEP is open for a total of seven months and allows you to enroll in Medicare Part A and Part B.
Why is Medicare Part A called Medicare Part A?
Medicare Part A is commonly referred to as “hospital insurance” because its primary function is to help older adults manage the cost of hospital bills.
Does Medicare cover chemotherapy?
What does Medicare Part A cover and not cover based on your status as a patient? If, for example, you need chemotherapy, Part A will cover it if it’s administered as a part of an inpatient hospital stay; if it’s done on an outpatient basis, Part A won’t cover it (but Part B will).
What does Medicare Part A cover?
Medicare Part A also covers inpatient hospital care required as part of a clinical research study.
How long does Medicare cover hospital care?
Hospital care. When you’re admitted to a hospital, Medicare Part A covers most of your costs for up to 60 days. You’re responsible for paying a benefit period deductible. This period begins the day you are admitted and ends when you have been out for 60 days in a row. Covered inpatient hospital services include:
What is a Part B?
Part B covers doctor visits and other outpatient services, like physical therapy and preventative care. Part C is an alternative to Parts A and B and is offered by Medicare-approved private insurers. Part D (prescription drug insurance) provides prescription drug coverage.
How long does Medicare Part A last?
Your IEP spans seven months—the three months before your birthday, your birthday month and the three months after your birthday.
What happens if you don't pay for Medicare?
If you didn’t pay into Social Security, you are not eligible for premium-free Medicare Part A coverage and you may be responsible for premiums of up to $458 per month. When you’re hospitalized, Medicare Part A pays most of the costs for stays of up to 60 days.
What is Medicare for 65?
Medicare is a federal health insurance program offered to people 65 years of age and older and younger people with certain disabilities and illnesses. Medicare has four different parts. Part A offers coverage for hospitalizations.
How long does a hospital stay last for a deductable benefit?
You will still be responsible for the benefit period deductible. A benefit period begins the day you are admitted into a hospital or skilled nursing facility and ends when you have been out for 60 days in a row. You may have multiple hospital stays during one benefit period.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What Medicare Part D Doesnt Cover
Medicare Part D is optional prescription drug coverage. You can enroll in this coverage through a stand-alone Medicare Part D Prescription Drug Plan, or through a Medicare Advantage Prescription Drug plan.
Coverage For Psychiatric Hospitalization
For inpatient psychiatric care, Medicare Part A will pay for the same kinds of services as if you were hospitalized in a general hospital:
Medical Equipment And Supplies
Splints, casts, prosthetic devices, body braces, heart pacemakers, corrective lenses after a cataract operation, therapeutic shoes for diabetics, and medical equipment such as ventilators, wheelchairs, and hospital beds if prescribed by a doctorare all covered by Part B medical insurance.
What Does Part B Cover
If a person has to stay at an ER overnight or for longer than 24 hours, hospital personnel should give them a Medicare Outpatient Observation Notice .
Is Medicaid Part Of Medicare
Medicare and Medicaid are different programs. Medicaid is not part of Medicare. Heres how Medicaid works for people who are age 65 and older: Its a federal and state program that helps pay for health care for people with limited income and assets.
How To Enroll In Medicare Part A
If you believe you would benefit from Part A coverage and qualify for it, the final step is the Part A enrollment process. If you are near the Medicare eligibility age of 65, its crucial to understand how your Initial Enrollment Period works.
How Much Does Observation In Hospital Cost With Medicare
If you receive hospital observation services but are not admitted as an inpatient, your doctors services are covered by Medicare Part B.
What is deductible in Medicare?
Deductible: This is an amount you have to spend before Medicare starts to pay for covered services. The deductible amount may change from year to year. Coinsurance: This is the part of the Medicare-approved costs for hospital care you may be required to pay after you’ve met your deductible.
What is original Medicare?
Original Medicare is a federal health insurance program managed by the Centers for Medicare & Medicaid Services (CMS). It provides health-care benefits for American citizens and permanent legal residents (of at least five years in a row) aged 65 or older. Find affordable Medicare plans in your area.
How many days can you draw on Medicare?
However, Medicare allows you a further 60 days of “lifetime reserve” days. This means that for the rest of your life you can draw on any of these 60 days—but no more—to extend Medicare coverage in any benefit period. In 2021, you pay $742 coinsurance per day for each lifetime reserve day.
How long is Medicare coinsurance for 2021?
This coinsurance ($371 in 2021) may vary from year to year and appears in your Medicare benefit coverage booklet. After 90 days of Medicare-covered inpatient hospital care in the same benefit period, you might be responsible for 100% of the costs. However, Medicare allows you a further 60 days of “lifetime reserve” days.
How much is the Medicare deductible for 2021?
You are responsible for the Medicare Part A hospital deductible ($1,484 in 2021), which applies to each new benefit period. You must pay the deductible before Medicare Part A covers services you received in the hospital.
How long does it take to get a coinsurance for a hospital stay?
All covered costs except the Part A deductible during the first 60 days. Coinsurance amounts for hospital stays from 61 to 90 days. After 91 days, a coinsurance amount usually applies for each “lifetime reserve day.”. You may get up to 60 lifetime reserve days during your lifetime.
How long do you have to stay in a hospital before you can get Medicare?
Hospital stay and skilled nursing facility care. Under the Original Medicare program, you must be admitted and spend at least 3 days in the hospital as an inpatient before Medicare will cover your stay in an approved skilled nursing facility (SNF) for further care.
What Does Part A of Medicare Cover?
Part A of Medicare covers inpatient care in a hospital. If you have a hospital stay that doesn't involve receiving inpatient care, it will not be covered by Medicare Part A. Part A also covers skilled nursing facility care, hospice care, some in-home health care, and nursing home care.
What Is the Difference Between Inpatient and Outpatient Care?
Understanding the difference between inpatient and outpatient care is important because this often determines which part of Medicare will cover your medical fees. Inpatient care involves receiving medical care overnight and specifically requires the length of your stay to be directly related to your medical care.
Lengthy Outpatient Stays and MOON Forms
If you are staying at an emergency room or hospital setting for over 24 hours but are not receiving inpatient care, then the hospital will be required to give you a Medicare Outpatient Observation Notice, or MOON form.
The Two-Midnight Rule
A general rule that determines inpatient designation is known colloquially as the “two-midnight rule”. If your doctor expects you to stay in the hospital for a time period that crosses two midnights, then you will be admitted as an inpatient.
When Will Part A Cover Emergency Room Visits?
Although Part A doesn’t always cover emergency room visits, there are situations where it will. Specifically, if you are admitted to the same hospital within three days of your initial emergency room visit.
Part B Coverage: Emergency Room Visits With No Hospital Admission
If you go to the emergency room and are treated as an outpatient, then you will receive Medicare coverage under Part B, not Part A. In this scenario, your coverage will function the same way as if you were at your normal doctor’s office.
Medicare Part B: Additional Fees
You will be responsible for a copayment for each visit, as well as 20 percent of the Medicare-approved amount. Your Part B deductible will also apply for outpatient visits to emergency rooms. If you receive a MOON form, that is one way to know that you will be responsible for these fees.
