If you’re a Medicare beneficiary that’s 65 or older, Medicare will pay for your home dialysis and supplies as long as your doctor deems them medically necessary. Medicare will often pay for a face-to-face meeting between you and your doctor as part of its coverage.
How much does Medicare pay for dialysis?
Your costs in Original Medicare. Inpatient dialysis treatments: If you have Original Medicare, Medicare pays most kidney doctors a monthly amount. After you pay the Part B yearly Deductible [glossary] , Medicare pays 80% of the monthly amount. You pay the remaining 20% Coinsurance.
What does Medicare Part B cover for dialysis?
Certain drugs for self-dialysis: Part B covers heparin, the antidote for heparin (when medically necessary), topical anesthetics, and erythropoiesis-stimulating agents (ESAs) (like epoetin alfa or darbepoetin alfa) to treat anemia related to your renal disease. Outpatient doctors’ services: Part B covers outpatient doctors’ services.
Does Medicare cover dialysis for ESRD?
Medicare Part B (Medical Insurance) to get the full benefits, including outpatient and home dialysis, available under Medicare for people with ESRD, and you must pay the premium to get Part B. Paying for dialysis services Medicare pays your dialysis facility to give you these Part B-covered dialysis services and items:
Does Medicare pay for ambulance transportation to dialysis?
In most cases, Medicare doesn’t pay for transportation to dialysis facilities. Learn more about medically necessary ambulance transportation to a dialysis facility. Important: You need Medicare Part B (and must pay the Part B premium) to get full ESRD benefits under Medicare, including outpatient and home dialysis.

How Much Does Medicare pay per dialysis treatment?
Medicare costs for dialysis treatment and supplies If you have Original Medicare, you'll continue to pay 20% of the Medicare-approved amount for all covered outpatient dialysis-related services, including those related to self-dialysis. Medicare will pay the remaining 80%.
Do any Medicare Advantage plans cover dialysis?
Medicare Advantage, or Part C, is the alternative to original Medicare. This plan also covers dialysis, but many people will not qualify for this option.
How much is dialysis treatment?
One dialysis treatment generally costs around $500 or more. For the usual three treatments per week, that would amount to more than $72,000 per year.
What is included in the dialysis bundle?
The “Dialysis Bundle” includes the dialysis treatment, laboratory tests, supplies, all injectable drugs, biologicals and their oral equivalent, and services provided for the dialysis treatment.
What benefits are dialysis patients entitled to?
The Social Security Administration (SSA) offers two types of disability benefit programs that you may be eligible for. Social Security disability benefits for kidney dialysis patients are available. To qualify for disability, you need to meet the SSA's Blue Book listing for dialysis.
Can kidneys start working again after dialysis?
Acute kidney failure requires immediate treatment. The good news is that acute kidney failure can often be reversed. The kidneys usually start working again within several weeks to months after the underlying cause has been treated. Dialysis is needed until then.
What is the life expectancy on dialysis?
Life expectancy on dialysis can vary depending on your other medical conditions and how well you follow your treatment plan. Average life expectancy on dialysis is 5-10 years, however, many patients have lived well on dialysis for 20 or even 30 years.
At what creatinine level should dialysis start?
National Kidney Foundation guidelines recommend you start dialysis when your kidney function drops to 15% or less — or if you have severe symptoms caused by your kidney disease, such as: shortness of breath, fatigue, muscle cramps, nausea or vomiting.
What happens if you only do dialysis twice a week?
These findings suggest that twice-weekly HD treatment can achieve a sufficient dialysis dose, similar to that of thrice-weekly HD treatment, if RKF is appropriately preserved. HD patients receiving infrequent HD treatment are at risk of high interdialytic weight gain and hypervolemic status.
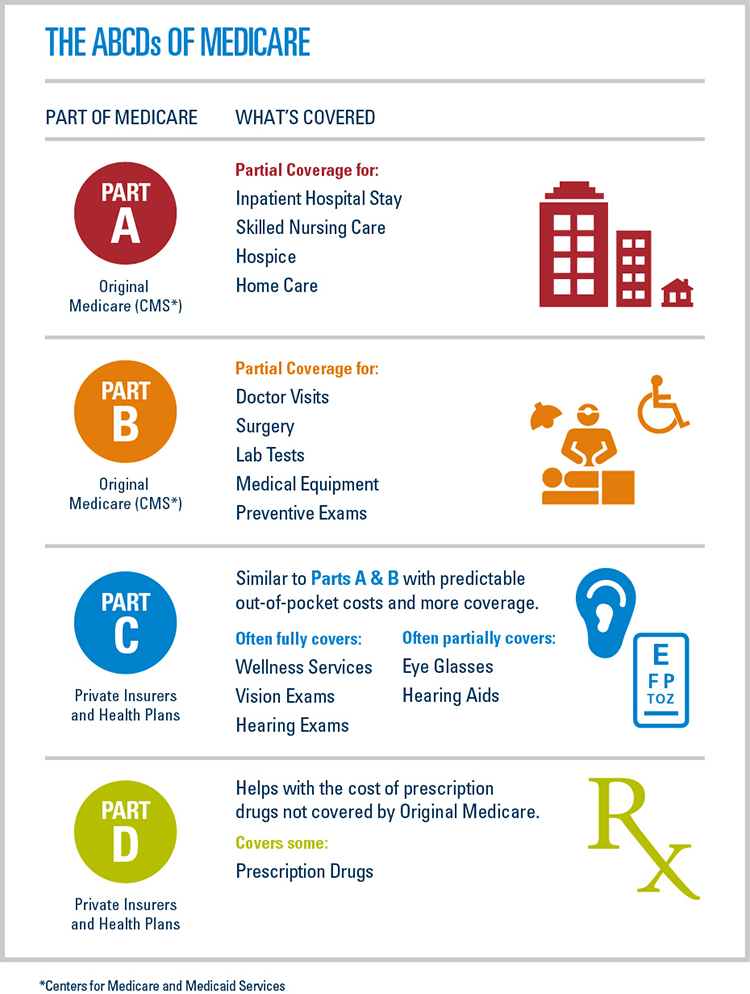
Is dialysis Part A or B?
Part B covers dialysis overseen in a Medicare-approved outpatient dialysis facility. You will typically pay a 20% coinsurance for the cost of each session, which includes equipment, supplies, lab tests, and most dialysis medications.
Does the government pay for kidney dialysis?
The Health 202: The government funds kidney dialysis for all who need it.
How much does Medicare pay for dialysis?
Once you pay your Part B deductible ( $203 per year in 2021), Medicare pays 80 percent of the monthly amount of your inpatient dialysis treatments, and you pay the remaining 20 percent coinsurance. If you get services for less than one month, your doctor may be paid per day.
What is covered by Medicare for self-dialysis?
Certain drugs for self-dialysis. Medicare Part B covers some drugs used in self-dialysis, including heparin and topical anesthetics (when medically necessary). ESRD-related drugs that only have an oral form of administration are only covered by Medicare Part D and Medicare SNPs. Medicare Part D plans (also known as Medicare Prescription Drug Plans) ...
How old do you have to be to get Medicare for ESRD?
To qualify for Medicare coverage of ESRD, you must: Be under the age of 65 and diagnosed with ESRD by a doctor. Have enough work history to qualify for Social Security Disability Insurance or Social Security Retirement Benefits or enough work history to qualify for benefits through the Railroad Retirement Board.
How to qualify for Medicare SNP?
To qualify for a Medicare SNP, you must get a note from your doctor confirming that you have the condition (in this case, ESRD) addressed by the Special Needs Plan.
Does Medicare cover dialysis?
All Medicare Advantage plans include an annual out-of-pocket spending limit, and most plans include prescription drug coverage, both of which Original Medicare doesn’t cover.
Is End-Stage Renal Disease covered by Medicare Advantage?
People with ESRD may qualify for Medicare, a Medicare Advantage plan or a Medicare Special Needs Plan (SNP).
When does Medicare start covering dialysis?
If you enroll in Medicare based on ESRD and you’re currently on dialysis, your Medicare coverage usually begins on the 1st day of your dialysis treatment’s 4th month. Coverage can start the 1st month if: During the first 3 months of dialysis, you participate in home dialysis training at a Medicare-certified facility.
What insurance covers dialysis?
Original Medicare (Part A hospital insurance and Part B medical insurance) covers many of the supplies and services needed for dialysis, including:
What is Medicare Part B?
Medicare Part B covers injectable and intravenous drugs and biologicals and their oral forms provided by the dialysis facility.
How long does it take for Medicare to resume?
Medicare coverage will resume if: within 12 months after the month , you stop getting dialysis, you start dialysis again or have a kidney transplant. within 36 months after the month you get a kidney transplant you get another kidney transplant or start dialysis.
How much is Medicare Part B 2020?
In 2020, the monthly premium for Medicare Part B is $144.60 and the annual deductible for Medicare Part B is $198. Once those premiums and deductibles are paid, Medicare typically pays 80 percent of the costs and you pay 20 percent.
How much is the deductible for Medicare Part A 2020?
The annual deductible for Medicare Part A is $1,408 (when admitted to a hospital) in 2020. This covers the first 60 days of hospital care in a benefit period. According to the U.S. Centers for Medicare & Medicare Services, about 99 percent of Medicare beneficiaries do not have a premium for Part A.
How long does Medicare cover kidney transplants?
If you’re only eligible for Medicare due to permanent kidney failure, your coverage will stop: 12 months after the month dialysistreatments are stopped. 36 months following the month youhave a kidney transplant. Medicare coverage will resume if: