What is a Medicare Advantage plan?
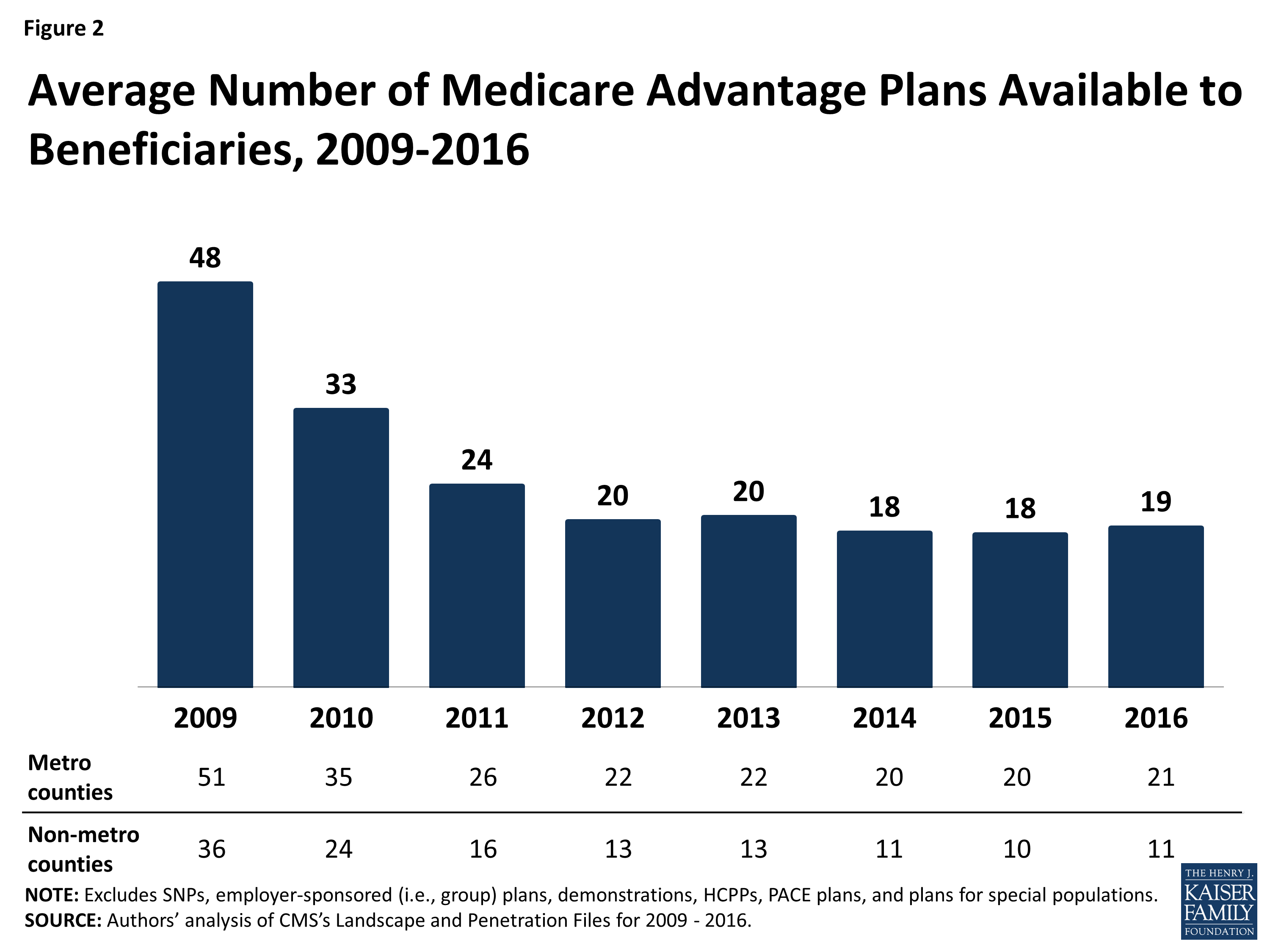
Beneficiary access to Medicare Advantage is strong. In 2018, Medicare Advantage included 2,317 individual plan options.5 In total, 99% of all Medicare beneficiaries have access to a Medicare Advantage plan and most beneficiaries have multiple plans to choose from in their
What is a 3 star rating for Medicare Advantage?
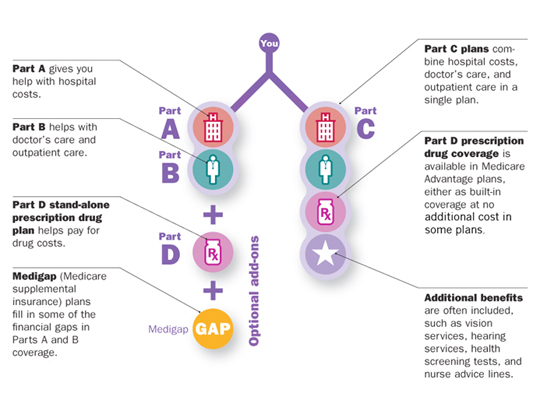
Medicare Advantage Plans cover almost all Part A and Part B services. However, if you’re in a Medicare Advantage Plan, Original Medicare will still cover the cost for hospice care, some new Medicare benefits, and some costs for clinical research studies. In all types of Medicare Advantage Plans, you’re always covered for
How are Medicare Advantage and prescription drug plans rated?
Most Medicare Advantage Plans include Medicare prescription drug coverage (Part D). In addition to your Part B premium, you usually pay one monthly premium for the plan’s medical and prescription drug coverage. Plan benefits can change from year to year. Make sure you understand how a plan
How do I look for Medicare Advantage plan reviews?
Oct 14, 2021 · A Best Insurance Company for Medicare Advantage Plans is defined as a company whose plans were all rated as at least three out of five stars by CMS and whose plans have an average rating of 4.5 or ...
How can a Medicare beneficiary use the star ratings?
If a Medicare Advantage Plan, Medicare drug plan, or Medicare Cost Plan with a 5-star rating is available in your area, you can use the 5-star Special Enrollment Period to switch from your current Medicare plan to a Medicare plan with a “5-star” quality rating.
What Medicare Advantage plan has the highest rating?
Best Medicare Advantage Plan Providers of 2022Best Reputation: Kaiser Foundation Health Plan.Best Customer Ratings: Highmark Blue Cross Blue Shield.Best for Extra Benefits: Aetna Medicare Advantage.Best for Large Network: Cigna-HealthSpring.Best for Promoting Health for Seniors: AARP/UnitedHealthcare.More items...
How are CMS Star Ratings calculated?
The results are now published annually. The Star Ratings are calculated based on a hospital's performance on certain measures found on the Care Compare website. Hospitals submit data to the Hospital IQR, OQR, Value-Based Purchasing, Readmission Reduction and HAC Reduction programs.Jan 15, 2021
How do I increase my star rating for Medicare Advantage?
7 Ways to Improve Your Star RatingEnsure Medication Benefits Are Central to the Consumer Onboarding Experience. ... Develop Targeted Outreach Programs Around Medication Adherence and Preventive Screening. ... Make Every Interaction Count. ... Be Proactive with Consumer Feedback. ... Communicate Consistently and in Different Channels.More items...•Nov 20, 2020
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
What are the negatives of a Medicare Advantage plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan; if you decide to switch to Medigap, there often are lifetime penalties.
Why are star ratings important to Medicare Advantage plans?
The Star Ratings system rewards higher-performing plans. This means that those with three or more stars receive annual bonus payments from the CMS. The higher the rating, the higher the bonus.Oct 7, 2021
How are star ratings determined?
Summary star ratings are an average of a provider's question level star ratings. Patient star ratings are calculated by dividing the patient's aggregate mean score by 20. For clients using only one question in the patient star rating, the star rating would simply be the individual question score, divided by 20.
What does a five-star rating mean?
The definition of five-star is something, such as a hotel or restaurant, that has the highest rating. An example of five-star is a top notch, world-class hotel. adjective. 4. Indicating the highest classification, based on a given set of criteria for determining excellence.
Who sets the standards for Medicare star ratings?
The Centers for Medicare & Medicaid Services (CMS) publishes the Medicare Part C and D Star Ratings each year to measure the quality of health and drug services received by beneficiaries enrolled in Medicare Advantage (MA) and Prescription Drug Plans (PDPs or Part D plans).Oct 13, 2020
Why are CMS star ratings important?
Medicare star ratings are important because they give you an idea about which plans in your area have the highest satisfaction ratings. Star ratings only pertain to Medicare Advantage and Part D plans. For both types of coverage, the ratings provide a way to compare your plan options beyond their cost.Oct 6, 2021
What is CMS star rating based on?
A nursing home's Overall Quality rating on Nursing Home Compare (www.medicare.gov) is based on its ratings for Health Inspections, Quality Measures (QMs), and Staffing. Ratings for each domain and the overall rating range from 1 star to 5 stars, with more stars indicating higher quality.
What is a special needs plan?
Special Needs Plan (SNP) provides benefits and services to people with specific diseases, certain health care needs, or limited incomes. SNPs tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
Can a provider bill you for PFFS?
The provider shouldn’t provide services to you except in emergencies, and you’ll need to find another provider that will accept the PFFS plan .However, if the provider chooses to treat you, then they can only bill you for plan-allowed cost sharing. They must bill the plan for your covered services. You’re only required to pay the copayment or coinsurance the plan allows for the types of services you get at the time of the service. You may have to pay an additional amount (up to 15% more) if the plan allows providers to “balance bill” (when a provider bills you for the difference between the provider’s charge and the allowed amount).
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
What is MSA plan?
Medicare Medical Savings Account (Msa) Plan. MSA Plans combine a high deductible Medicare Advantage Plan and a bank account. The plan deposits money from Medicare into the account. You can use the money in this account to pay for your health care costs, but only Medicare-covered expenses count toward your deductible.
What is a special needs plan?
Special Needs Plans (SNPs) Other less common types of Medicare Advantage Plans that may be available include. Hmo Point Of Service (Hmopos) Plans. An HMO Plan that may allow you to get some services out-of-network for a higher cost. and a. Medicare Medical Savings Account (Msa) Plan.
Does Medicare Advantage include drug coverage?
Most Medicare Advantage Plans include drug coverage (Part D). In many cases , you’ll need to use health care providers who participate in the plan’s network and service area for the lowest costs.
What is Medicare Advantage Plan?
Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are an “all in one” alternative to Original Medicare. They are offered by private companies approved by Medicare. If you join a Medicare Advantage Plan, you still have. Medicare.
What happens if you don't get a referral?
If you don't get a referral first, the plan may not pay for the services. to see a specialist. If you have to go to doctors, facilities, or suppliers that belong to the plan for non-emergency or non-urgent care. These rules can change each year.
Does Medicare cover dental?
Covered services in Medicare Advantage Plans. Most Medicare Advantage Plans offer coverage for things Original Medicare doesn’t cover, like some vision, hearing, dental, and fitness programs (like gym memberships or discounts). Plans can also choose to cover even more benefits. For example, some plans may offer coverage for services like ...
What are the star ratings for Medicare?
The Medicare Star Ratings are assigned to Medicare plans based on five aspects of each plan: 1 Screening tests and vaccines#N#This criterion evaluates the type of access that plan members have to preventive services such as annual physicals, screenings, and vaccines. 2 Management of chronic conditions#N#This measures how efficiently care is coordinated for plan members with chronic conditions and how often they receive treatment for long-term health issues. 3 Member experience with the plan#N#Plan members’ overall satisfaction with the plan is factored into this rating criteria. 4 Member complaints and changes in plan performance#N#This reflects how often plan members issued complaints about the plan, experienced problems receiving covered services or opted out of the plan entirely. It also measures how the plan’s performance improved from the previous year. 5 Customer service#N#Medicare evaluates the quality of service at the plan’s call center and how efficiently appeals and enrollments were processed.
What to consider when shopping for Medicare Advantage?
There are several things you may want to consider when shopping for a Medicare Advantage plan (Medicare Part C), such as plan cost, coverage and availability. You can get some help as you compare Medicare Advantage plans by using plan ratings and insurance company reviews.
When is the open enrollment period for Medicare?
This period lasts from October 15 to December 7 each year.
Does Medicare Advantage have coinsurance?
Medicare Advantage plans may offer a variety of benefits that are not covered by Original Medicare , and these additional benefits can differ from one plan to the next.
Who is Christian Worstell?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. .. Read full bio
When was the Medicare Advantage rule released?
CMS followed up with the release of the final rule, Contract Year 2019 Policy and Technical Changes to the Medicare Advantage, Medicare Cost Plan, Medicare Fee-for-Service, the Medicare Prescription Drug Benefit Programs, and the Program for All-inclusive Care for the Elderly (PACE) on Friday, April 6, 2018.
What are the requirements for Medicare Part B?
The final rule eliminates the requirement that providers and prescribers participate in Medicare Part B as a condition of participating in MA, Part D or PACE. As an alternative, CMS will adopt a “preclusion list” of individuals and entities that fall within either of two categories: 1 Are currently revoked from Medicare, are under a re-enrollment bar, and CMS determines that the underlying conduct that led to the revocation is detrimental to the Medicare program 2 Have engaged in behavior for which CMS could have revoked the individual or entity to the extent applicable if they had been enrolled in Medicare, and CMS determines that the underlying conduct that would have led to the revocation would have been detrimental to the Medicare program
What is the CMS final rule?
In the final rule, CMS finalized a reinterpretation of statutory language to allow supplemental benefits that compensate for physical impairments, reduce the impact of injuries or health conditions, and/or reduce avoidable emergency room utilization.
When was the MA capitation released?
The Centers for Medicare and Medicaid Services (CMS) on April 2, 2018, released the final version of the 2019 Medicare Advantage (MA) Capitation Rates, combined with the MA and Part D Payment Policies and the Part D Call Letter.
What is the proposed rule?
The proposed rule stated that the policy is intended to foster greater “competition, innovation, available benefit offerings, and provide beneficiaries with affordable plans that are tailored for their unique health care needs and financial situation.”.
Does CMS require multiple bids?
CMS will eliminate the requirement that permits MAOs to submit multiple bids for the same area only if the plans substantially different from one another based on key plan characteristics such as premiums, cost sharing, or benefits offered. The proposed rule stated that the policy is intended to foster greater “competition, innovation, available benefit offerings, and provide beneficiaries with affordable plans that are tailored for their unique health care needs and financial situation.”
What is a V-BID plan?
The MA Value-based Insurance Design Model (V-BID) offers supplemental benefits or reduced cost sharing to enrollees with certain chronic conditions. CMS will expand the model in 2019 to begin allowing plans to submit V-BID proposals for the following states: