What is a Medicare fee schedule?
· Local Coverage Articles are a type of educational document published by the Medicare Administrative Contractors (MACs). Articles often contain coding or other guidelines that are related to a Local Coverage Determination (LCD). Finding a specific code. Some articles contain a large number of codes.
What is the cervical colposcopy code 57452?
Listed below are basic costs for people with Medicare. If you want to see and compare costs for specific health care plans, visit the Medicare Plan Finder. For specific cost information (like whether you've met your deductible , how much you'll pay for an item or service you got, or the status of a claim ), log into your secure Medicare account.
How much are Medicare taxes for Medicare Part A?
· Fee Schedules - General Information. A fee schedule is a complete listing of fees used by Medicare to pay doctors or other providers/suppliers. This comprehensive listing of fee maximums is used to reimburse a physician and/or other providers on a fee-for-service basis. CMS develops fee schedules for physicians, ambulance services, clinical ...
How much does Medicare pay for home health care?
· Physician Fee Schedule Look-Up Tool | CMS Physician Fee Schedule Look-Up Tool Get Eligibility Information: Cognitive Assessment & Care Plan Services Data You can now check Medicare eligibility (PDF) for Cognitive Assessment & Care Plan Services (CPT 99483) data. If you need help, contact your eligibility service provider.

Does Medicare pay for flow cytometry?
Claims for Flow Cytometry services are payable under Medicare Part B in the following places of service: For CPT codes 86355, 86356, 86357, 86359, 86360 and 86361: office (11), independent clinic (49), federally qualified health center (50), rural health clinic (72), and independent laboratory (81);
Does Medicare allow G2212?
CMS finalized in their calendar year 2021 rule that they do not agree with the CPT® chart for using time for 99417. For Medicare patients, use the HCPCS code G2212.
Is 99446 covered by Medicare?
New Medicare coverage for interprofessional consults and virtual check-ins. Beginning Jan. 1, Medicare will pay separately for interprofessional consults. The new CPT codes are 99451–99452 and 99446–99449 and payment ranges from about $18 to about $73 dollars depending on the time involved.
Is 0097U covered by Medicare?
Medicare will allow only one GIP multiplex panel (CPT code 87505, 87506, 87507 or 0097U) per day per beneficiary by the same or different provider consistent with the related LCD.
How is G2212 billed?
Providers may bill G2212 only when choosing the level of E/M services based on time, not MDM. Providers must spend an entire 15 minutes providing E/M services for each unit of G2212 billed. In other words, 1-14 additional minutes of E/M service does not warrant a unit of G2212.
Is G2212 covered by Medicaid?
b. CPT code 99417 is listed on the OHA prioritized list as a covered service, but G2212 is not currently listed. Moda Health will accept 99417 for processing for Medicaid plans. c.
Who can Bill 99446?
CPT code 99446 is defined as an interprofessional telephone or internet assessment and management service provided by a consultative physician, including a verbal and written report to the patient's treating/requesting physician or other QHP, and involves 5–10 minutes of medical consultative discussion and review.
How do I bill for an e consult?
Code 99451 is reported by the consultant, allowing him/her to access data/information through the electronic health record (EHR), in addition to telephone or internet. Code 99452 is reported by the requesting/treating physician/QHP (e.g., the primary care physician).
What is the difference between a consultation and a referral?
A consultation is a request by a qualified provider for the advice or opinion of a physician regarding the evaluation and/or management of a specific problem. A referral is the transfer of care from one physician to a second physician when the second takes over responsibility for treatment of the patient.
What is CPT 0097U?
0097U. GASTROINTESTINAL PATHOGEN, MULTIPLEX REVERSE TRANSCRIPTION AND MULTIPLEX AMPLIFIED PROBE TECHNIQUE, MULTIPLE TYPES OR SUBTYPES, 22 TARGETS (CAMPYLOBACTER [C. JEJUNI/C. COLI/C. UPSALIENSIS], CLOSTRIDIUM DIFFICILE [C.
What does CPT 87798 test for?
Infectious agent detection by nucleic acidCPT® Code 87798 in section: Infectious agent detection by nucleic acid (DNA or RNA), not otherwise specified.
What is the CPT code for gastrointestinal panel?
Medicare will allow only one GIP multiplex panel (CPT code 87505, 87506 or 87507) per day per beneficiary by the same or different provider consistent with the related LCD.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
How much will Medicare cost in 2021?
Most people don't pay a monthly premium for Part A (sometimes called " premium-free Part A "). If you buy Part A, you'll pay up to $471 each month in 2021. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $471. If you paid Medicare taxes for 30-39 quarters, the standard Part A premium is $259.
How much is coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). Beyond Lifetime reserve days : All costs. Note. You pay for private-duty nursing, a television, or a phone in your room.
How much is the Part B premium for 91?
Part B premium. The standard Part B premium amount is $148.50 (or higher depending on your income). Part B deductible and coinsurance.
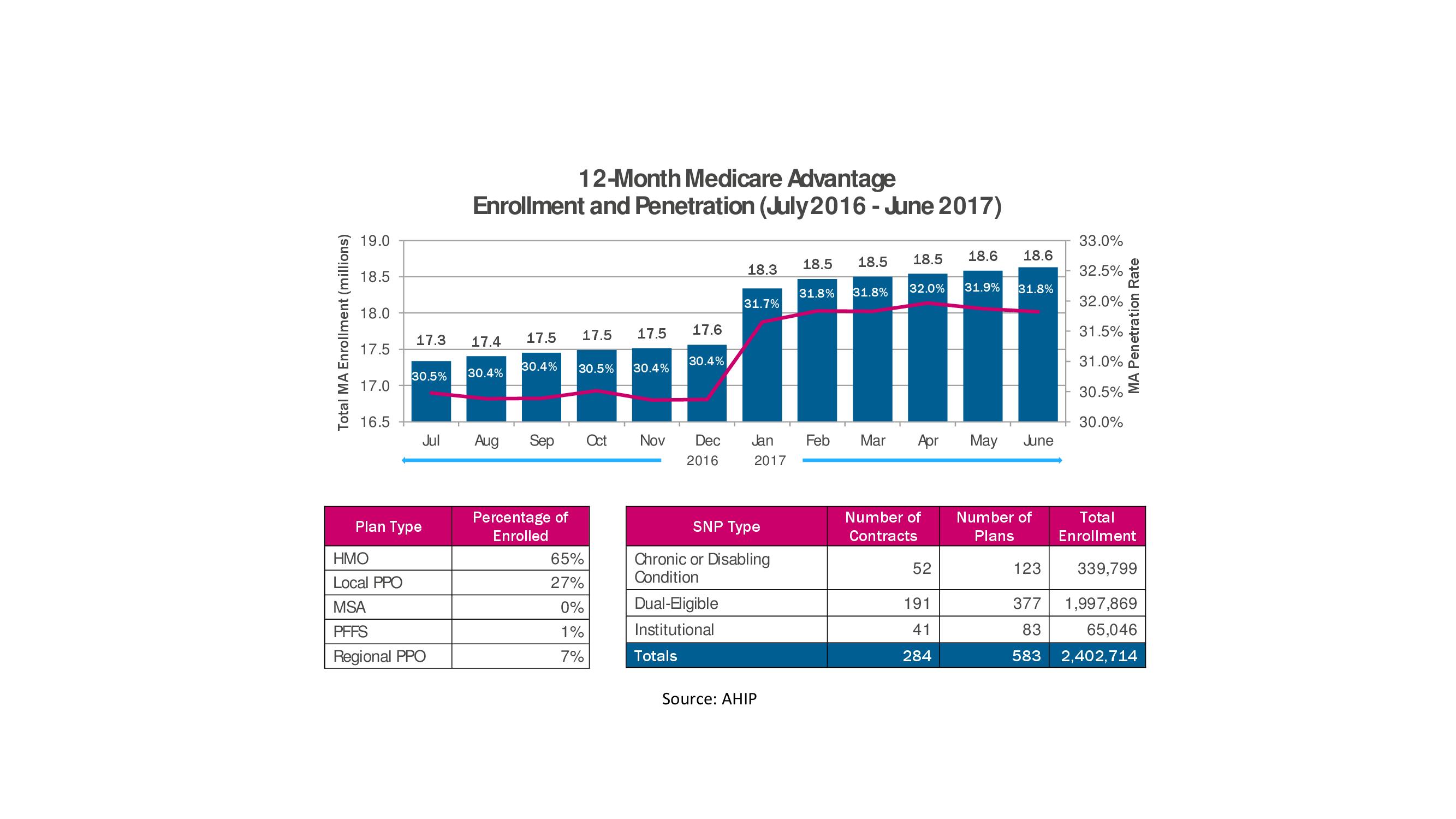
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How long does a SNF benefit last?
The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins. You must pay the inpatient hospital deductible for each benefit period. There's no limit to the number of benefit periods.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.
Why is it difficult to know the exact cost of a procedure?
For surgeries or procedures, it may be dicult to know the exact costs in advance because no one knows exactly the amount or type of services you’ll need. For example, if you experience complications during surgery, your costs could be higher.
Does Medicare cover wheelchairs?
If you’re enrolled in Original Medicare, it’s not always easy to find out if Medicare will cover a service or supply that you need. Generally, Medicare covers services (like lab tests, surgeries, and doctor visits) and supplies (like wheelchairs and walkers) that Medicare considers “medically necessary” to treat a disease or condition.
What is the benefit period for Medicare?
benefit period. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services. A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row.
How much coinsurance is required for a day 91?
Days 91 and beyond: $742 coinsurance per each “lifetime reserve day” after day 90 for each benefit period (up to 60 days over your lifetime).
Does Medicare cover outpatient care?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
Does Medicare cover private duty nursing?
Medicare doesn’t cover: Private duty nursing. A phone or television in your room. Personal items, like toothpaste, socks, or razors (except when a hospital provides them as part of your hospital admission pack). A private room, unless medically necessary.
Who is covered by Part A and Part B?
All people with Part A and/or Part B who meet all of these conditions are covered: You must be under the care of a doctor , and you must be getting services under a plan of care created and reviewed regularly by a doctor.
What is personal care?
Custodial or personal care (like bathing, dressing, or using the bathroom), when this is the only care you need
Does Medicare cover home health services?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process.
Can a nurse practitioner provide home health care without a physician?
During the COVID-19 pandemic, nurse practitioners, clinical nurse specialists, and physician assistants can now provide home health services, without the certification of a physician.
What is CPT code 47370?
CPT Code 47370 – Laparoscopy, surgical, ablation of one or more liver tumor (s); radiofrequency
When to use modifier 59?
Modifier 59 is used appropriately for different anatomic sites during the same encounter only when procedures which are not ordinarily performed or encountered on the same day are performed on different organs, or different anatomic regions, or in limited situations on different, non-contiguous lesions in different anatomic regions of the same organ
What is 20604 in ultrasound?
20604 Arthrocentesis, aspiration and/or injection, small joint or bursa (eg, fingers, toes); with ultrasound guidance, with permanent recording and reporting (Do not report 20600, 20604 in conjunction with 76942) (If fluoroscopic, CT, or MRI guidance is performed, see 77002, 77012, 77021)
Is 76942 a biopsy code?
A: Yes. Code 76942, Ultrasonic guidance for needle placement (eg, biopsy, aspiration, injection, localization device), imaging supervision and interpretation, requires that the ultrasound is used to guide the needle such as for that the ultrasound is used to guide the needle such as for a needle biopsy or fine needle aspiration (FNA) of an organ or body area.
What is the unit of service for CPT code 76942?
Under the National Correct Coding Initiative, NCCI, which sets CMS payment policy as well as many private payers, one unit of service is allowed for CPT code 76942 in a single patient encounter regardless of the number of needle placements performed. Per NCCI, “The unit of service for these codes is the patient encounter, not number of lesions, number of aspirations, number of biopsies, number of injections, or number of localizations.
Can you get denied for ultrasound for knee joint injections?
Therefore, unless there is documentation provided to support the medical necessity for the ultrasound guidance for knee joint injections, the ultrasound guidance may be denied as coverage and reimbursement of healthcare services provided to Medicare beneficiaries requires that services be medically necessary in order to be eligible for reimbursement.
Can you report 76942 twice?
Therefore, if several passes are made into two separate lesions in the same organ ( ie, two lesions in same breast), then code 76942 would be reported twice.