Medicare pays for one IPPE per beneficiary per lifetime for beneficiaries within the first 12 months of the effective date of the beneficiary’s first Medicare Part B coverage period. This document explains the elements in the IPPE.
Medicare Part B covers physician services, outpatient hospital services, certain home health services, durable medical equipment, and certain other medical and health services not covered by Medicare Part A.
When does Medicare pay for IPPE?
Medicare pays 1 patient IPPE per lifetime not later than the first 12 months after the patient’s Medicare Part B benefits eligibility date. Medicare pays the IPPE costs if the provider accepts assignment.
Are Medicare Part B beneficiaries eligible for the IPPE?
It is important to remember that Medicare beneficiaries are only eligible for the IPPE if they are in their first 12 months of Medicare Part B coverage. After the first 12 months of coverage, beneficiaries are eligible for the Annual Wellness Visit. This benefit is covered 100% for the beneficiary.
Are there any additional once in a lifetime benefits with IPPE?
Additional once in a lifetime benefits in conjunction with the IPPE. Screening Electrocardiogram (EKG) – Medicare no longer deems the screening EKG as a mandatory service component of the IPPE. However, there is a once-in-a-lifetime screening EKG that is allowed as a result of a referral from an IPPE and must be performed at the time of the IPPE.
What is the IPPE?
The IPPE is an introduction to Medicare and covered benefits and focuses on health promotion, disease prevention, and detection to help patients stay well. We encourage providers to inform patients about the AWV and perform such visits.

What is included in Medicare Ippe?
The Initial Preventive Physical Examination (IPPE) is also known as the “Welcome to Medicare Preventive Visit.” The IPPE is a preventive visit offered to newly-enrolled Medicare beneficiaries. Despite its name, the IPPE does not include an extensive physical examination.
How much does Medicare reimburse for annual wellness visit?
around $117Patients are eligible for this benefit every year after their Initial Annual Wellness Visit. The reimbursement is around $117.
What is the difference between Ippe and Awv?
A: The IPPE is a 1-time visit that occurs within the first 12 months of a patient's enrollment in Medicare Part B. The AWV can take place every 12 months, either 12 months after the IPPE or after more than 12 months of enrollment.
What is included in the annual wellness visit?
It involves a physical exam by a doctor and includes bloodwork and other tests. The annual wellness visit will just include checking routine measurements such as height, weight, and blood pressure.
How many times can a patient have an Ippe performed?
Initial Preventive Physical Examination (IPPE) The IPPE, known as the “Welcome to Medicare” preventive visit, promotes good health through disease prevention and detection. Medicare pays for 1 patient IPPE per lifetime not later than the first 12 months after the patient's Medicare Part B benefits eligibility date.
Do Medicare wellness visits need to be 12 months apart?
Q - Do Medicare wellness visits need to be performed 365 days apart? A - No. A Medicare wellness visit may be performed in the same calendar month (but different year) as the previous Medicare wellness visit.
Can Medicare annual wellness visits be done over the phone?
As a result, Medicare beneficiaries will now be able to use audio-only telephone visits to receive annual wellness visits (G0438-G0439), advance care planning (99497-99498), tobacco and smoking cessation counseling (99406-99407), and many behavioral health and patient education services.
Can an RN perform an Awv?
Whether a LPN or RN can perform any parts of the AWV/IPPE, CMS explains this is up to the individual provider. Also, remember that the IPPE/AWV is not a Complete Physical Exam, but merely hits on some of CMS desired metrics.
How many preventive physical exams does Medicare cover?
one initial preventive physicalA person is eligible for one initial preventive physical examination (IPPE), also known as a Welcome to Medicare physical exam, within the first 12 months of enrolling in Medicare Part B. Medicare enrollment typically begins when a person turns 65 years old.
What is not included in a wellness visit?
Your insurance for your annual wellness visit does not cover any discussion, treatment or prescription of medications for chronic illnesses or conditions, such as high blood pressure, high cholesterol or diabetes.
Does Medicare wellness exam include blood work?
Any blood work or lab tests that may be part of a physical exam, are also not included under a Medicare Annual Wellness Visit. The purpose of the annual wellness visit under Medicare is to paint a picture of your current state of health and to create a baseline for future care.
Can I refuse the Medicare Annual Wellness visit?
The Medicare Annual Wellness Visit is not mandatory. While you may take advantage of these visits for free once per year, it's not a requirement to keep your Medicare benefits. There is no penalty if you choose not to go.
Who pays for IPPE?
Medicare pays the IPPE costs if the provider accepts assignment.
What is an IPPE visit?
The IPPE, known as the “Welcome to Medicare” preventive visit, promotes good health through disease prevention and detection. Medicare pays for 1 patient IPPE per lifetime not later than the first 12 months after the patient’s Medicare Part B benefits eligibility date. 1.
How long does Medicare cover AWV?
Medicare covers an AWV for all patients who aren’t within 12 months after the eligibility date for their first Medicare Part B benefit period and who didn’t have an IPPE or an AWV within the past 12 months. Medicare pays for only 1 IPPE per patient per lifetime and 1 additional AWV per year thereafter.
How many times can you report ACP?
There are no limits on the number of times you can report ACP for a certain patient in a certain time period. When billing this patient service multiple times, document the change in the patient’s health status and/or wishes regarding their end-of-life care. Preparing Eligible Medicare Patients for the AWV.
What is a patient in Medicare?
The term “patient” refers to a Medicare beneficiary.
Does Medicare cover EKG?
No. Medicare waives both the coinsurance/copayment and the Medicare Part B deductible for the IPPE (HCPCS code G0402). Neither is waived for the screening electrocardiogram (ECG/EKG) (HCPCS codes G0403, G0404, or G0405).
Is IPPE covered by Medicare?
The IPPE is an introduction to Medicare and covered benefits and focuses on health promotion, disease prevention, and detection to help patients stay well. We encourage providers to inform patients about the AWV and perform such visits. The SSA explicitly prohibits Medicare coverage for routine physical examinations.
What is an IPPE in Medicare?
The initial preventive physical examination (IPPE), or “Welcome to Medicare Preventive Visit” is a preventive visit authorized by sections 1861 (s) (2) (w) and 1861 (ww) of the Social Security Act (and implementing regulations at 42 CFR 410.16, 411.15 (a) (1), and 411.15 (k) (11)).
When is the IPPE billable?
Effective for a beneficiary who has the IPPE on or after January 1, 2009, and within his/her 12-month enrollment period of Medicare Part B, the IPPE and screening EKG services are billable with the appropriate HCPCS G code (s).
What is HCPCS G0439?
All subsequent AWVs shall be billed with HCPCS G0439 (Annual Wellness Visit, including PPPS, subsequent visit). In the event that a beneficiary selects a new health professional to complete a subsequent AWV, the new health professional will continue to bill the subsequent AWV with HCPCS G0439.
What is the HCPCS code for IPPE?
If the primary physician or qualified NPP performs only the IPPE, he/she shall bill HCPCS code G0344 only. The physician or entity that performs the screening EKG that includes both the interpretation and report shall bill HCPCS code G0366. The physician or entity that performs the screening EKG tracing only (without interpretation and report) shall bill HCPCS code G0367. The physician or entity that performs the interpretation and report only (without the EKG tracing) shall bill HCPCS code G0368. Medicare will pay for a screening EKG only as part of the IPPE. HCPCS codes G0344, G0366, G0367 and G0368 will not be billable codes effective on or after January 1, 2009.
When was HCPCS G0438 billed?
For the first AWV provided on or after January 1, 2011, the health professional shall bill HCPCS G0438 (Annual wellness visit, including PPPS, first visit). This is a once per beneficiary per lifetime allowable Medicare Part B benefit.
When did Medicare deductibles go away?
As a result of the Affordable Care Act (ACA), effective for the IPPE provided on or after January 1, 2011, the Medicare deductible and coinsurance (for HCPCS code G0402 only) are waived.
How long after the first Medicare Part B coverage period can you furnish?
Must furnish no later than 12 months after the effective date of the first Medicare Part B coverage period
What is the Medicare remittance advice code?
Your Medicare contractors will use the appropriate Remittance Advice Remark Code, i.e., N117 (This service is paid only once in a patient’s lifetime) when denying additional claims for an IPPE and/or a screening EKG.
What modifier is used for OPPS?
Hospitals subject to OPPS (TOBs 12X and 13X) must use modifier 25 when billing the IPPE G0344 along with technical component of the EKG, G0367, on the same claim. The same is true when billing IPPE code G0402 along with the technical component of the screening EKG, code G0404.
What is CMS 410.16?
Pursuant to Section 101 (b) of the Medicare Improvement for Patients and Providers Act of 2008 (MIPPA), CMS is amending section 410.16 and related regulation provisions of the Code of Federal Regulations . Effective January 1, 2009, this expanded coverage is subject to certain eligibility and other limitations that allow payment for an IPPE, also
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Is my test, item, or service covered?
Find out if your test, item or service is covered. Medicare coverage for many tests, items, and services depends on where you live. This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What is original Medicare?
Your costs in Original Medicare. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. .
What is a coinsurance percentage?
Coinsurance is usually a percentage (for example, 20%). , and the Part B deductible may apply if: Your doctor or other health care provider performs additional tests or services during the same visit. The preventative benefits don't cover these additional tests or services.
What to do if you have a prescription for opioids?
If you have a current prescription for opioids, your provider will review your potential risk factors for opioid use disorder, evaluate your severity of pain and current treatment plan, provide information on non-opioid treatment options, and may refer you to a specialist, if appropriate. Your provider will also review your potential risk factors for substance use disorder and refer you for treatment, if needed.
Does preventive insurance cover additional tests?
The preventive benefits don't cover these additional tests or services.
Does Medicare have to pay coinsurance?
The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. doesn’t apply. However, you may have to pay. coinsurance. An amount you may be required to pay as your share of the cost for services after you pay any deductibles.
What is an IPPE in Medicare?
An IPPE or AWV performed on Medicare Part B patients qualifies as an “initiating” visit for care management conducted within the year prior to starting. This allow FQHCs to be reimbursed for care management services, including Chronic Care Management (CCM), Behavioral Health Integration (BHI), and/or Psychiatric Collaborative Care Model (CoCM), for substance use disorders.
Does Medicare require a face to face visit?
Medicare requires a face-to-face initiating visit (i.e., IPPE, AWV or any Evaluation and Management Visit [E&M]) with the billing practitioner for new patients or established patients not seen within one (1) year prior to starting care management services.
Is IPPE part of CMS?
CMS/Medicare covers several types of initiating visits, including IPPE, AWV, and E/M. The initiating visit is not part of care management services and is billed separately. If a comprehensive IPPE, AWV, or E/M was billed for an established FQHC patient within the past year, an initiating visit is not required.
What is an IPPE?
The Initial Preventive Physical Examination (IPPE) is also known as the “Welcome to Medicare Preventive Visit.” The goals of the IPPE are health promotion and disease prevention and detection. Medicare pays for one IPPE per beneficiary per lifetime for beneficiaries
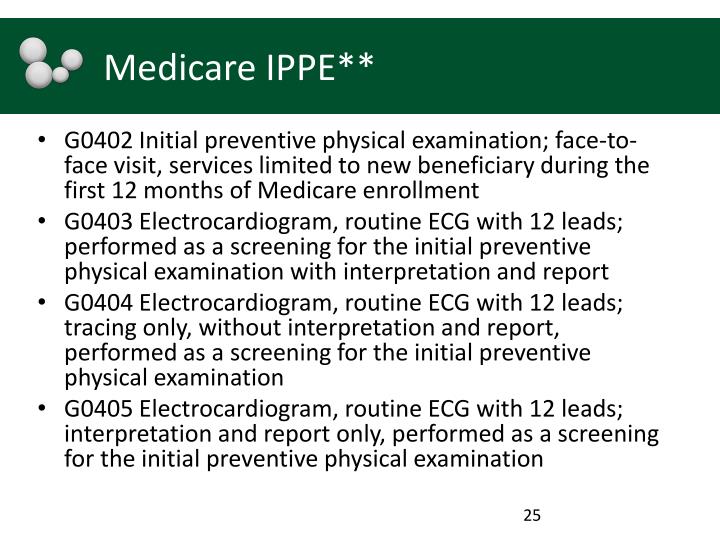
How many leads does a G0403 have?
G0403 Electrocardiogram, routine ECG with 12 leads; performed as a screening for the initial preventive physical
Is IPPE a one time benefit?
get an IPPE. This is a one-time benefit. Diagnosis
Is IPPE a separate service?
NOTE: The IPPE is a separate service from the Annual Wellness Visit (AWV). For more information about the AWV, refer to “The ABCs of the Annual Wellness Visit (AWV)” at http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLN Products/MLN-Publications-Items/CMS1246474.html on the Centers for Medicare & Medicaid Services (CMS) website.
What is the IPPE for Medicare?
The IPPE is designed for “health promotion and disease detection,” per Medicare. The following requirements of the IPPE can found at the CMS website at: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/preventive-services/medicare-wellness-visits.html
What is IPPE exam?
Medicare calls this exam the Initial Preventative Physical Exam, or IPPE, but it is more widely known as the “Welcome to Medicare Visit.”. This is a great benefit that also includes several exams that are normally not covered.
Does Medicare pay for ultrasound for aortic aneurysm?
Medicare will pay for this once-in-a-lifetime benefit as long as your patient meets the following requirements:
Does Medicare require an EKG?
Screening Electrocardiogram (EKG) – Medicare no longer deems the screening EKG as a mandatory service component of the IPPE. However, there is a once-in-a-lifetime screening EKG that is allowed as a result of a referral from an IPPE and must be performed at the time of the IPPE.
