
Full Answer
How exactly does Medicare cover mental health?
Under Medicare Part B, you can expect to pay the following for outpatient mental health treatment:
- $203 yearly deductible in 2021
- 20% of the Medicare-approved amount for each service after meeting Part B deductible
- Copayment or coinsurance fees for services at hospital outpatient clinics or departments
Who can bill Medicare for mental health services?
Part B covers mental health services and visits with these types of health professionals: An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
Does Medicaid improve mental health?
While these programs do not focus exclusively on mental health, Medicaid is the single largest funder of mental health services in the country, which makes this support especially valuable. The federal government also provides Mental Health Block Grants (MHBG) that support states in building out their community mental health services.
Is your mental health care covered by Medicare?
It helps to have your policy number ready before you call ... experts at 800-686-1578 can help consumers understand what mental health care and medications different plans cover. Medicare does not have to follow parity laws, except for cost-sharing ...
What is the Medicare approved amount for psychotherapy?
Mental health services, such as individual counseling provided in an outpatient setting will be covered at 80% of the approved charge with Medicare Part B after the annual deductible ($233 for 2022) is met. You pay the other 20%.
Does Medicare cover depression and anxiety?
Medicare cares about your mental health and offers services to support you. Mental health conditions, like depression or anxiety, can happen at any time to anyone. So, it's important to talk to your doctor if you're experiencing: Thoughts of ending your life.
Does Medicare take care of mental health?
Medicare Part B covers mental health services you get as an outpatient, such as through a clinic or therapist's office. Medicare covers counseling services, including diagnostic assessments including, but not necessarily limited to: Psychiatric evaluation and diagnostic tests. Individual therapy.
What does Medicare cover for depression?
An annual depression screening that you receive in a primary care setting. Speak to your doctor or primary care provider for more information. The depression screening is considered a preventive service, and Medicare covers depression screenings at 100% of the Medicare-approved amount.
How many free psychology sessions are under Medicare?
As such, Medicare rebates are available for psychological treatment by registered psychologists. Under this scheme, individuals diagnosed with a mental health disorder can access up to 10 individual Medicare subsidised psychology sessions per calendar year. As of October 9, 2020 this has been doubled to 20.
Does Medicare pay for bipolar?
Many mental conditions, such as bipolar disorder, depression, and schizophrenia, can be managed by prescription medications. Medicare Part D provides you with coverage for prescriptions. Before selecting a Part D plan, be sure to evaluate the plan's formula to make sure it covers your important mental health drugs.
How Much Does Medicare pay for 90837?
$132.69What is the difference between the “facility rate” and “nonfacility rate” for telehealth services?CodeService2021 Facility Rate90832Psychotherapy 30-minutes$68.7490837Psychotherapy 60-minutes$132.6996132Neuropsych Test Eval$106.0896158Hlth Bhvr Intrv Indvl$58.971 more row•Dec 10, 2021
Does Medicare Part B cover depression?
Medicare Part B covers mental health services related to your outpatient treatment, including intensive outpatient treatment programs and yearly depression screenings. This type of treatment is important for anyone who needs ongoing mental health support.
What is the Medicare patient's responsibility for one depression screening a year?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers one depression screening per year.
What does screening for depression mean?
What is depression screening? A depression screening, also called a depression test, helps find out if you have depression. Depression is a common, though serious, illness. Everyone feels sad at times, but depression is different than normal sadness or grief. Depression can affect how you think, feel, and behave.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. applies. If you get your services in a hospital outpatient clinic or hospital outpatient department, you may have to pay an additional. copayment.
What is a health care provider?
health care provider. A person or organization that's licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers. to diagnose or treat your condition.
What is Medicare preventive visit?
A one-time “Welcome to Medicare” preventive visit. This visit includes a review of your possible risk factors for depression. A yearly “Wellness” visit. Talk to your doctor or other health care provider about changes in your mental health. They can evaluate your changes year to year.
Can you do individual and group psychotherapy with a doctor?
Individual and group psychotherapy with doctors or certain other licensed professionals allowed by the state where you get the services.
Do you pay for depression screening?
You pay nothing for your yearly depression screening if your doctor or health care provider accepts assignment. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
How long does Medicare cover mental health?
If you’re in a psychiatric hospital, you’re covered for only up to 190 days of inpatient services over your lifetime. After that, you’d need to receive mental health services in a general hospital to be covered.
What percentage of Medicare beneficiaries are living with mental health issues?
Mental health issues are common among older adults: Thirty-one percent of Original Medicare beneficiaries are living with mental illness, according to a July 2020 report by the Commonwealth Fund, a private foundation focused on health care. And in a July 2020 survey by the Kaiser Family Foundation, 46% of Americans ages 65 and up said ...
How much is the deductible for mental health?
What you’ll pay for inpatient mental health care. A deductible of $1,484 applies to inpatient psychiatric care for each benefit period. You will owe no coinsurance for the first 60 days of a hospital stay for psychiatric treatment. But you will owe copays of 20% of the Medicare-approved amount for mental health services you receive from doctors ...
How much is the psychiatric deductible?
A deductible of $1,484 applies to inpatient psychiatric care for each benefit period. You will owe no coinsurance for the first 60 days of a hospital stay for psychiatric treatment. But you will owe copays of 20% of the Medicare-approved amount for mental health services you receive from doctors and other providers while you're an inpatient.
How much is coinsurance after 90 days?
Your daily coinsurance jumps to $742 per each “lifetime reserve day” after day 90. (In Original Medicare, lifetime reserve days are a set number of days that are covered by Medicare when you're in the hospital for more than 90 days; you have up to 60 days in your lifetime.) After that, you pay all costs.
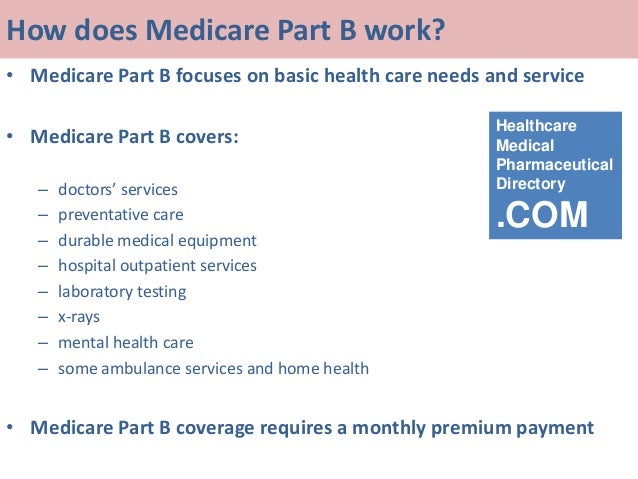
What is Medicare Part B?
Medicare Part B, which pays doctor bills and related health care expenses, covers many mental health services rendered to patients not admitted to a hospital. Covered costs include: A “Welcome to Medicare” visit that includes a review of your risk factors for depression.
What is a psychotherapist evaluation?
Psychiatric evaluation to diagnose mental illness and prepare a care plan. Diagnostic testing. Individual and group psychotherapy or counseling provided by physicians or certain other professionals licensed to do so in your state.
How long does Part A pay for mental health?
If you're in a psychiatric hospital (instead of a general hospital), Part A only pays for up to 190 days of inpatient psychiatric hospital services during your lifetime.
What is Medicare Part A?
Mental health care (inpatient) Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. covers mental health care services you get in a hospital that require you to be admitted as an inpatient.
How much is Medicare coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). In Original Medicare, these are additional days that Medicare will pay for when you're in a hospital for more than 90 days.
How much is original Medicare deductible?
Your costs in Original Medicare. $1,484. deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. for each. benefit period.
Can you have multiple benefit periods in a general hospital?
for mental health services you get from doctors and other providers while you're a hospital inpatient. Note. There's no limit to the number of benefit periods you can have when you get mental health care in a general hospital. You can also have multiple benefit periods when you get care in a psychiatric hospital.
Does Medicare pay for mental health?
In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. for mental health services you get from doctors and other providers while you're a hospital inpatient.
Who does Medicare subcontract to?
Medicare subcontracts out to many different subcontractors like Noridian or Palmetto or Novitas or NGS or WPS or FCSO.
Is a payment average a guarantee?
These are payment averages that do not represent the rates of any of the aforementioned insurance companies are a not a guarantee of any rate or payment amount.
Is Medicaid easy to work with?
Not all companies are easy to work with even if they pay well. Medicaid can be the trickiest of them all, not listed here.
Does Medicaid pay poorly?
Sadly, Medicaid pays poorly and is overly complex, often requiring license-level modifiers and taxonomy codes. The reason I would recommend working with Medicaid is to establish a very busy practice (perhaps with a billing team on your side) and/or because you want to serve this population of folks in need.
When is the 2019 Medicare Physician Fee Schedule released?
These provisions are part of the final rule on the 2019 Medicare Physician Fee Schedule and Quality Payment Program, released by CMS in early November. Highlights of the Final Rule include.
What is the final rule for Medicare?
Final Rule on 2019 Medicare Physician Fee Schedule and Quality Payment Program. For 2019, the Centers for Medicare and Medicaid Services (CMS) has reduced administrative burdens on physicians associated with documentation and preserved separate payments for each of the existing levels of evaluation and management ...
Does Medicare update fee schedules?
Back to Medicare. Medicare maintains and updates fee schedules for all health care related costs including physicians, ambulance services, clinical labs, and durable medical equipment. The Medicare Physician Fee Schedule is updated on an annual basis through the rule-making process.
What factors affect insurance reimbursement rate for psychotherapy?
Factors that effect your insurance reimbursement rate for psychotherapy: Location, paying more for under-served locales and less for over-served locations. License, education, and specialization. Specialization. Consumer demand at the time of signing your contract.
What does your Medicaid license impact?
Your Medicaid License impacts the “Practitioner Level” that you have which influences your reimbursement rates.
Does Medicare cover mental health?
Medicare doesn’t cover all licenses and is far more selective than Medicaid about which providers they will allow into their network. As a result, mental health reimbursement rates for Medicare are higher than Medicaid rates by a substantial margin.
Does Medicaid pay out based on coding?
Medicaid requirements for licensing vary state by state. Likewise, Medicaid pays out differing rates based on very specific criteria and coding.
Is a mental health therapist licensed?
In most states, mental health therapists are initially licensed as an LPC or LMHC or LPCMH or LCPC or LPCC (and on and on), depending on your state. While it’s safe to assume you already know your license for your state, you can also check this PDF document here to confirm your license and what’s required.
Does insurance pay for mental health therapists?
In summary, some private insurance companies reimburse mental health therapists for far more than others. A great way to quickly learn which companies pay the most is to simply ask your colleagues about their experiences with different reimbursement rates for private insurance companies.
Does Medicare cover psychotherapy?
Medicare reduces insurance reimbursement rates for psychotherapy on a relative basis . Here’s that same charge but with a calculated reduction on rates of 40%:
