Coverage: Medicare Part B helps pay for individual and group psychotherapy with doctors or certain other licensed professionals allowed by the state where you get the services. Medicare pays 80 percent of the Medicare-approved amount. You pay 20 percent of the Medicare-approved amount, the Part B deductible, and coinsurance costs.
Full Answer
Does Medicare cover psychotherapy?
Medicare benefits may help cover the costs of certain types of therapeutic services. As described by the American Psychiatric Association (APA), psychotherapy uses a number of techniques to help patients improve their mental health by addressing troublesome behaviors and emotional difficulties.
How much physical therapy will Medicare pay for?
On average, Medicare part B will pay between $97 and $105 for a 60-minute, 4-unit physical therapy treatment. The initial evaluation visit typically reimburses at a higher rate of $130 to $160 on average due to the higher relative value of the initial evaluation code. What determines Medicare Part B Reimbursement rates for Physical Therapy?
How much of hospice does Medicare pay for?
How much hospice care costs depends on the type of illness and how early patients enter hospice. In 2018, the Society of Actuaries estimated that hospice patients with cancer received Medicare Part A and Part B benefits totaling around $44,030 during the last 6 months of their lives.
Does Medicare cover 90837?
Medicare telehealth includes 17 mental and behavioral health services: • 90785 Interactive complexity (Note: This service must be listed separately in addition to the code for primary procedure) • 90791 Psychiatric diagnostic evaluation • 90832 Psychotherapy, 30 minutes with patient • 90834 Psychotherapy, 45 minutes with patient • 90837 Psychotherapy, 60 minutes with patient

Does Medicare reimburse me for psychotherapy?
Medicare Part B covers mental health services you get as an outpatient, such as through a clinic or therapist's office. Medicare covers counseling services, including diagnostic assessments including, but not necessarily limited to: Psychiatric evaluation and diagnostic tests. Individual therapy.
How Much Does Medicare pay for 90837?
$132.69What is the difference between the “facility rate” and “nonfacility rate” for telehealth services?CodeService2021 Facility Rate90832Psychotherapy 30-minutes$68.7490837Psychotherapy 60-minutes$132.6996132Neuropsych Test Eval$106.0896158Hlth Bhvr Intrv Indvl$58.971 more row•Dec 10, 2021
Does Medicare pay for cognitive behavioral therapy?
Cognitive Behavioral Therapy (CBT) as psychotherapy via telemental health is covered by Medicare for certain eligible beneficiaries.
What is the Medicare reimbursement rate?
roughly 80 percentAccording to the Centers for Medicare & Medicaid Services (CMS), Medicare's reimbursement rate on average is roughly 80 percent of the total bill. Not all types of health care providers are reimbursed at the same rate.
What is the difference between 90837 and 90834?
Both 90834 and 90837 are designed to bill for the same service – psychotherapy. The primary distinguishing factor between the two codes is time; 90834 is defined as 45 minutes of psychotherapy, while 90837 is defined as 60 minutes.
What does cognitive behavioral therapy involve?
CBT treatment usually involves efforts to change thinking patterns. These strategies might include: Learning to recognize one's distortions in thinking that are creating problems, and then to reevaluate them in light of reality. Gaining a better understanding of the behavior and motivation of others.
Is hypnotherapy covered by Medicare?
Hypnotherapy isn't typically covered by Medicare, though it could potentially be covered in some circumstances if your doctor is able to bill Medicare for the services.
Does Medicaid cover therapy?
Therapy Is Covered By Medicaid Medicaid also covers in-person and online individual and group therapy. Many providers offer family therapy, too. So long as you have a diagnosis and a medical prescription for a specific therapy, your health insurance provider should cover it.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. applies. If you get your services in a hospital outpatient clinic or hospital outpatient department, you may have to pay an additional. copayment.
What is Medicare preventive visit?
A one-time “Welcome to Medicare” preventive visit. This visit includes a review of your possible risk factors for depression. A yearly “Wellness” visit. Talk to your doctor or other health care provider about changes in your mental health. They can evaluate your changes year to year.
What is a health care provider?
health care provider. A person or organization that's licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers. to diagnose or treat your condition.
Do you pay for depression screening?
You pay nothing for your yearly depression screening if your doctor or health care provider accepts assignment. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
What is the Medicare Part B coverage for a clinical psychologist?
Clinical psychologists diagnose and treat mental, emotional, and behavioral disorders – and are one of the health care providers covered by Medicare Part B. Coverage: Medicare pays 80 percent of the Medicare-approved amount. You pay 20 percent of the Medicare-approved amount, the Part B deductible, and coinsurance costs.
What percentage of Medicare does a nurse practitioner pay?
Nurse practitioners. Physician assistants. Coverage: Medicare pays 80 percent of the Medicare-approved amount. You pay 20 percent of the Medicare-approved amount, the Part B deductible, and coinsurance costs.
What is Medicare Part B?
Coverage: Medicare Part B helps pay for a psychiatric evaluation. Medicare pays 80 percent of the Medicare-approved amount. You pay 20 percent of the approved amount, the Part B deductible, and coinsurance costs.
Does Medicare cover marriage counseling?
Medicare does not cover other types of relationship counseling, such as marriage counseling. You’re only covered for mental health services from a licensed psychiatrist, clinical psychologist, or other health care professional who accepts Medicare assignment.
Does Medicare cover depression screening?
Coverage: A yearly depression screening and preventive visit does not cost anything if your doctor or health care provider accepts assignment.
Does Medicare cover mental health?
Medicare Coverage of Mental Health Services. A person’s mental health refers to their state of psychological, emotional, and social well-being – and it’s important to take care of it at every stage of life , from childhood to late adulthood. Fortunately, Medicare beneficiaries struggling with mental health conditions may be covered ...
Medicare Part B covers a variety of mental health services, including psychotherapy
Yes, Medicare does generally cover psychotherapy. Each person’s mental health needs are different, and Medicare covers a wide variety of therapeutic options. In most cases, getting your mental healthcare needs covered will be very simple. However, there are many things to keep in mind as you begin the process.
Which Mental Health Services Does Medicare Cover?
Medicare covers a wide variety of mental health treatments. This includes psychotherapy and counseling services provided by a clinical psychologist or psychiatrist, clinical social worker, nurse practitioner, clinical nurse specialist, or physician assistant. Group psychotherapy and family counseling are often covered in most cases as well.
Does Medicare Cover Mental Health Medications?
Under Original Medicare, prescription drugs form a unique category and are usually not covered if they are self-administered. This is also the case when it comes to psychiatric medications, such as antidepressants, anticonvulsants, and antipsychotic medications.
Medicare Part A: What Mental Healthcare is Covered?
Part A, often referred to as “hospital insurance”, covers your healthcare costs in an inpatient setting. This could be a general hospital or a psychiatric hospital. In either case, Original Medicare will cover you in the same way.
Understanding Part A Benefit Periods
The cost for Part A is determined by where you are in your benefit period. A benefit period begins the day that you are admitted to a hospital (general or psychiatric), and ends when you’ve gone 60 days without any inpatient care.
How Much Does Part A Cost?
Part A has a deductible which you have to pay during each benefit period. If you are admitted to a hospital, you will begin paying your deductible. Once it is fully paid, then your coverage will begin. If you enter a new benefit period, even in that same year, then you will have to pay your deductible again.
Medicare Part B: Psychotherapy and More
Medicare Part B covers your outpatient care. Most forms of psychotherapy and group therapy will fall under Part B.
What factors affect insurance reimbursement rate for psychotherapy?
Factors that effect your insurance reimbursement rate for psychotherapy: Location, paying more for under-served locales and less for over-served locations. License, education, and specialization. Specialization. Consumer demand at the time of signing your contract.
Does insurance pay for mental health therapists?
In summary, some private insurance companies reimburse mental health therapists for far more than others. A great way to quickly learn which companies pay the most is to simply ask your colleagues about their experiences with different reimbursement rates for private insurance companies.
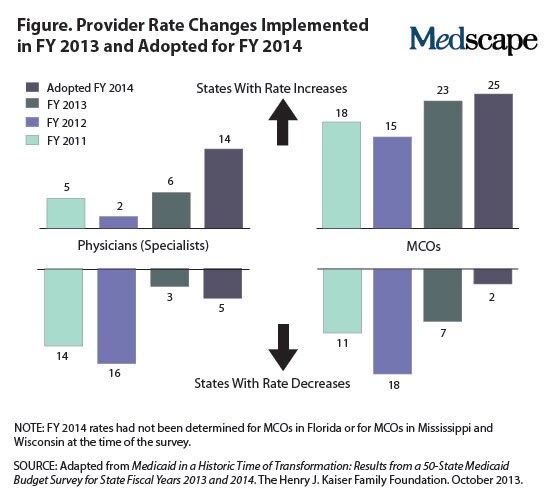
Does Medicare cover mental health?
Medicare doesn’t cover all licenses and is far more selective than Medicaid about which providers they will allow into their network. As a result, mental health reimbursement rates for Medicare are higher than Medicaid rates by a substantial margin.
How many depression screenings are there in Medicare?
Medicare Part B pays for one depression screening each year. The screening must happen in the office of a primary care doctor or similar to ensure there is appropriate follow-up care.
What is Medicare Part A?
Medicare does provide coverage for therapy, as well as for other mental health care needs. Medicare Part A helps cover hospital stays. Medicare Part B helps cover doctor visits and day programs in a hospital.
What is a Medicare preventive visit?
When a person first enrolls in Medicare, they receive a Welcome to Medicare preventive visit. During this visit, a doctor reviews risks of depression. Yearly wellness visits can then include discussions with a person’s doctor on any changes to mental health that may have occurred since the last visit.
What is mental health?
A person’s mental health includes their mental, emotional, and social well-being. These functions affect feelings, thoughts, and actions, including how a person manages stress and makes friends. Mental health is important in every stage of life, and life events can trigger both physical and emotional responses.
How many reserve days do you have to use for Medicare?
all costs after lifetime reserve days have been used in full. A person has 60 lifetime reserve days to use during their lifetime. In Part B, there are out-of-pocket costs for diagnosis and treatment. A person must pay 20% of the Medicare-approved amount after the Part B deductible is met.
Does Medicare cover transportation?
During partial hospitalization Medicare does not cover: meals. transport. support groups (group therapy is covered) job skills testing or training that is not part of treatment. Medicare parts A and B do not cover prescribed medication taken at home, but a person can use Medicare Part D to help pay for these costs.
Does Medicare pay for mental health screenings?
Medicare also covers a yearly mental health screening with an approved Medicare health expert. Original Medicare does not pay for meals, transport, or most prescribed drugs. A person needs Medicare Part D to cover prescription medication.
When is the 2019 Medicare Physician Fee Schedule released?
These provisions are part of the final rule on the 2019 Medicare Physician Fee Schedule and Quality Payment Program, released by CMS in early November. Highlights of the Final Rule include.
What is the final rule for Medicare?
Final Rule on 2019 Medicare Physician Fee Schedule and Quality Payment Program. For 2019, the Centers for Medicare and Medicaid Services (CMS) has reduced administrative burdens on physicians associated with documentation and preserved separate payments for each of the existing levels of evaluation and management ...
Does Medicare update fee schedules?
Back to Medicare. Medicare maintains and updates fee schedules for all health care related costs including physicians, ambulance services, clinical labs, and durable medical equipment. The Medicare Physician Fee Schedule is updated on an annual basis through the rule-making process.
Does Medicaid pay poorly?
Sadly, Medicaid pays poorly and is overly complex, often requiring license-level modifiers and taxonomy codes. The reason I would recommend working with Medicaid is to establish a very busy practice (perhaps with a billing team on your side) and/or because you want to serve this population of folks in need.
Is Medicaid subcontracted?
Many Medicaid polices are subcontracted out to lower paying organizations. This can skew data downward in comparison to brands that to not facilitate a Medicaid plan in that State. Likewise, EAP sessions have far more hoops, billing nuance, and prior-to-session manual labor (authorizations) involved in billing.