If you do receive your physical therapy at a doctor’s office or other outpatient center, Medicare will cover 80 percent of the Medicare-approved cost. This cost is predetermined by the insurance company as the maximum amount they will pay for a specific service. You will be required to pay the additional 20 percent of the treatment out of pocket.
What does Medicare pay for physical therapy?
Medicare Part B (Medical Insurance) helps pay for Medically necessary outpatient physical therapy. You pay 20% of the Medicare-approved amount, and the Part B deductible applies.
Does Medicare pay for outpatient therapy services?
Medicare law no longer limits how much it pays for your medically necessary outpatient therapy services in one calendar year.
Does Medicare Part C cover physical therapy?
Part C (Medicare Advantage) covers physical therapy as a Medicare-covered service with the same restrictions and requirements as Original Medicare. Depending on your plan, you may need a referral, prior authorization or approval, and an in-network physical therapist for your plan to pay.
Does insurance cover physical therapy in a hospital?
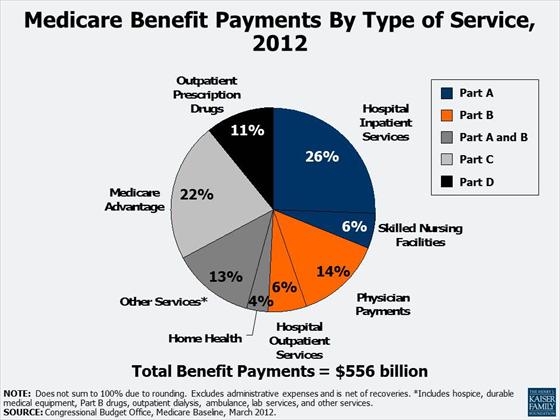
Part A (hospital insurance) covers physical therapy as an inpatient service in a hospital or skilled nursing facility (SNF) if it’s a Medicare-covered stay, or as part of your home health care benefit.
How much does Medicare reimburse for physical therapy?
However, in 2018, the therapy cap was removed. Original Medicare covers outpatient therapy at 80% of the Medicare-approved amount. When you receive services from a participating provider, you pay a 20% coinsurance after you meet your Part B deductible ($233 in 2022).
Will Medicare pay for physical therapy at home?
Medicare Part B medical insurance will cover at home physical therapy from certain providers including private practice therapists and certain home health care providers. If you qualify, your costs are $0 for home health physical therapy services.
What can physical therapists bill for?
Physical therapists can bill for:Telehealth. ... Evaluation and Treatment on the Same Day. ... Therapeutic Massage. ... Maintenance Therapy. ... Durable Medical Equipment (DME) ... One-on-One Services in a Group. ... Student-Led Services. ... Dry Needling.More items...•
How often does a PT have to see a Medicare patient?
The PT must recertify the POC “within 90 calendar days from the date of the initial treatment,” or if the patient's condition evolves in such a way that the therapist must revise long-term goals—whichever occurs first.
How many days of therapy Does Medicare pay for?
How many days of physical therapy will Medicare pay for? Medicare doesn't limit the number of days of medically necessary outpatient therapy service in one year that it will pay for.
Does Medicare cover outpatient physical therapy?
Yes. Physiotherapy can be covered by Medicare so long as it's a chronic and complex musculoskeletal condition requiring specific treatment under the CDM.
How do you maximize physical therapy billing?
Ten Ways Physical Therapists Can Maximize BillingSet goals. As a therapist, you've got a lot of experience in the goal-setting department. ... Track your progress. ... Increase efficiency. ... Educate yourself and your staff. ... Clean up your claims. ... Digitize. ... Know your payer mix. ... Keep an eye on cash flow.More items...•
How Much Does Medicare pay for 97110?
CPT 97110 can be used for therapeutic procedures in time units of 15 minutes. The reimbursement rate is $30.30 and will be paid if the three important factors are reported correctly.
What codes can a physical therapist Bill?
Physical Therapy CPT Codes97161: Physical therapy evaluation, low complexity.97162: Physical therapy evaluation, moderate complexity.97163: Physical therapy evaluation, high complexity.
Does Medicare pay for home caregivers?
Medicare typically doesn't pay for in-home caregivers for personal care or housekeeping if that's the only care you need. Medicare may pay for short-term caregivers if you also need medical care to recover from surgery, an illness, or an injury.
Does Medicare cover physical therapy for arthritis?
Medicare Part B Medicare will usually cover doctor's visits related to arthritis, physical therapy, and some DME, such as splints, braces, walkers, or canes. A person is often required to obtain prior authorization from Medicare before purchasing equipment or pursuing therapy services.
What is plan of care in physical therapy?
The POC consists of statements that specify the anticipated goals and expected outcomes, predicted level of optimal improvement, specific interventions to be used, and proposed duration and frequency of the interventions. The POC describes the specific patient/client management for the episode of physical therapy care.
Does Medicare pay for home caregivers?
Medicare typically doesn't pay for in-home caregivers for personal care or housekeeping if that's the only care you need. Medicare may pay for short-term caregivers if you also need medical care to recover from surgery, an illness, or an injury.
Does Medicare cover physical therapy for arthritis?
Medicare Part B Medicare will usually cover doctor's visits related to arthritis, physical therapy, and some DME, such as splints, braces, walkers, or canes. A person is often required to obtain prior authorization from Medicare before purchasing equipment or pursuing therapy services.
What is the Medicare cap for 2022?
For several years, the cap was $6,700, although most plans have had out-of-pocket caps below that level. For 2021, the maximum out-of-pocket limit for Medicare Advantage plans increased to $7,550 (plus out-of-pocket costs for prescription drugs), and it's staying at that level for 2022.
How Long Does Medicare pay for physical therapy after knee replacement?
Medicare covers inpatient rehab in a skilled nursing facility – also known as an SNF – for up to 100 days. Rehab in an SNF may be needed after an injury or procedure, like a hip or knee replacement.
What is Medicare Part B?
With your healthcare provider’s verification of medical necessity, Medicare Part B covers the evaluation and treatment of injuries and diseases that prohibit normal function. Physical therapy may be needed to remedy the issue, maintain the present functionality or slow the decline.
What are the different types of physical therapy?
Medical News Today describes several different types of physical therapy across a wide spectrum of conditions: 1 Orthopedic: Treats injuries that involve muscles, bones, ligaments, fascias and tendons. 2 Geriatric: Aids the elderly with conditions that impact mobility and physical function, such as arthritis, osteoporosis, Alzheimer’s, hip and joint replacements, balance disorders and incontinence. 3 Neurological: Addresses neurological disorders, Alzheimer’s, brain injury, cerebral palsy, multiple sclerosis, Parkinson’s disease, spinal cord injury and stroke. 4 Cardiovascular: Improves physical endurance and stamina. 5 Wound care: Includes manual therapies, electric stimulation and compression therapy. 6 Vestibular: Restores normal balance and coordination that can result from inner ear issues. 7 Decongestive: Promotes draining of fluid buildup.
How much is the Medicare Part B deductible for 2020?
In 2020, the Part B deductible is $198 per year under Original Medicare benefits.
What is the difference between geriatric and orthopedic?
Orthopedic: Treats injuries that involve muscles, bones, ligaments, fascias and tendons. Geriatric: Aids the elderly with conditions that impact mobility and physical function, such as arthritis, osteoporosis, Alzheimer’s, hip and joint replacements, balance disorders and incontinence.
How much does physical therapy cost on Medicare?
How much does physical therapy cost under Medicare insurance? Patients pay 20% of the Medicare-approved amount for therapy. However, if your physical therapist charges more than the Medicare-approved amount for treatment, you must pay the difference. Since these services are covered under Part B, the Part B deductible also applies.
What is the difference between occupational therapy and physical therapy?
Occupational therapy: Occupational therapy focuses on helping people improve or regain skills necessary for everyday activities.
What are the different types of therapists?
Medicare insurance covers several types of therapy: 1 Physical therapy: This therapy is designed to help the patient improve balance, strength, flexibility, and other areas of physical ability. Physical therapy might be used after an injury or surgery to help the patient regain normal functionality. 2 Occupational therapy: Occupational therapy focuses on helping people improve or regain skills necessary for everyday activities. This is a broad category of therapy and includes therapy for activities of daily living like bathing. eating, and dressing; skills needed to get and keep a job; and social skills. 3 Speech therapy: Also known as speech-language pathology, speech therapy treats a wide range of speech and voice challenges, including trouble finding the right words, creating meaningful and grammatically correct sentences, and using the proper volume when speaking.
How old do you have to be to get Medicare Part B?
Most people who qualify for Medicare Part B insurance do so based on their age of 65 older. But you could also qualify if you meet at least one of the following requirements: You are disabled and have received Social Security Disability Income for two years.
What is speech therapy?
Speech therapy: Also known as speech-language pathology, speech therapy treats a wide range of speech and voice challenges, including trouble finding the right words, creating meaningful and grammatically correct sentences, and using the proper volume when speaking.
Is eligibility.com a Medicare provider?
Eligibility.com is a DBA of Clear Link Technologies, LLC and is not affiliated with any Medicare System Providers.
Does Medicare cover end stage renal disease?
You have End-Stage Renal Disease (ESRD). Learn more about who qualifies for Medicare. Medicare Advantage plans also cover physical therapy, since they are required to cover everything Medicare Part A and Part B cover. There may be additional benefits with some Medicare Advantage insurance plans, and your costs may differ from Original Medicare.
Why is Physical Therapy Valuable?
According to the American Physical Therapy Association (APTA), physical therapy can help you regain or maintain your ability to move and function after injury or illness. Physical therapy can also help you manage your pain or overcome a disability.
Does Medicare Cover Physical Therapy?
Medicare covers physical therapy as a skilled service. Whether you receive physical therapy (PT) at home, in a facility or hospital, or a therapist’s office, the following conditions must be met:
What Parts of Medicare Cover Physical Therapy?
Part A (hospital insurance) covers physical therapy as an inpatient service in a hospital or skilled nursing facility (SNF) if it’s a Medicare-covered stay, or as part of your home health care benefit.
Does Medicare Cover In-home Physical Therapy?
Medicare Part A covers in-home physical therapy as a home health benefit under the following conditions:
What Are the Medicare Caps for Physical Therapy Coverage?
Medicare no longer caps medically necessary physical therapy coverage. For outpatient therapy in 2021, if you exceed $2,150 with physical therapy and speech-language pathology services combined, your therapy provider must add a modifier to their billing to show Medicare that you continue to need and benefit from therapy.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What is physical therapy and why is it so important for seniors?
Physical therapy is an important part of recovery for many seniors after undergoing an injury or surgery. This vital healthcare specialty includes the well-rounded evaluation, assessment, and treatment of individuals who deal with physical limitations as a result of illness, disability, surgery, or injury.
Does Medicare pay for physical therapy?
You may be pleasantly surprised to learn that Original Medicare will, in fact, pay for at least a portion of physical therapy visits that are considered to be medically necessary by a patient’s doctor.
How can I get even more comprehensive Medicare coverage for my specific healthcare needs?
The simple answer to the question “does Medicare cover physical therapy?” is yes, with conditions. That said, did you know that it may be possible to enroll in a Medicare plan that offers even more comprehensive healthcare coverage than Original Medicare?
What is the Medicare therapy cap?
The Medicare therapy cap was a set limit on how much Original Medicare would pay for outpatient therapy in a year. Once that limit was reached, you had to request additional coverage through an exception in order to continue getting covered services. However, by law, the therapy cap was removed entirely by 2019.
What is Medicare Part B?
Occupational therapy. Speech-language pathology services. Medicare Part B pays 80 percent of the Medicare-approved amount for outpatient therapy services received from a provider who accepts Medicare assignment. You are responsible for 20 percent of the cost ...
What is an ABN for a physical therapist?
This is true for physical therapy, speech-language pathology and occupational therapy. This notice is called an Advance Beneficiary Notice of Noncoverage (ABN). If your provider gives you an ABN, you may agree to pay for the services that aren’t medically necessary. However, Medicare will not help cover the cost.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
Does Medicare Advantage cover rehab?
Your costs for Medicare rehab coverage with a Medicare Advantage plan (Part C) depend on the specific plan you have. Medicare Advantage plans are offered by private insurance companies and approved by Medicare. These plans must provide coverage at least as good as what’s provided by Original Medicare (Parts A & B).
Does Medicare pay for outpatient therapy?
Technically, no. There is no limit on what Medicare will pay for outpatient therapy, but after your total costs reach a certain amount, your provider must confirm that your therapy is medically necessary in order for Medicare to cover it.1.
What is a medical social service?
Medical social services. Part-time or intermittent home health aide services (personal hands-on care) Injectible osteoporosis drugs for women. Usually, a home health care agency coordinates the services your doctor orders for you. Medicare doesn't pay for: 24-hour-a-day care at home. Meals delivered to your home.
What is the eligibility for a maintenance therapist?
To be eligible, either: 1) your condition must be expected to improve in a reasonable and generally predictable period of time, or 2) you need a skilled therapist to safely and effectively make a maintenance program for your condition , or 3) you need a skilled therapist to safely and effectively do maintenance therapy for your condition. ...
Who is covered by Part A and Part B?
All people with Part A and/or Part B who meet all of these conditions are covered: You must be under the care of a doctor , and you must be getting services under a plan of care created and reviewed regularly by a doctor.
Does Medicare cover home health services?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process.
What are the factors that determine Medicare coverage?
Medicare coverage is based on 3 main factors 1 Federal and state laws. 2 National coverage decisions made by Medicare about whether something is covered. 3 Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
