N264: Missing/incomplete/invalid ordering provider name. N575: Mismatch between the submitted ordering/referring provider name and records. A CO16 denial does not necessarily mean that information was missing. It could also mean that specific information is invalid.
When to use a Medicare denial reason code?
Thus, it must be always used along with a claim adjustment reason code for showing liability for the amounts that are not covered under Medicare for a service or claim. Medicare denial codes are standard messages used to provide or describe information to a medical patient or provider by insurances about why a claim was denied.
What is the ICD code for Medicare remittance co 65?
Medicare remittance CO 65, CO 133 & CO 170 171 172 - Medical Billing and Coding - Procedure code, ICD CODE. Procedure code was incorrect. This payment reflects the correct code.
What does denial code 97 mean on claim form?
Note: If its valid diagnosis and procedure code, then you have rights to appeal with supporting documentation. Denial code - 97 described when "The benefit for this service is included in the payment or allowance for another service/procedure that has already been adjudicated". 1) Claim denial date?
What is the CPT code for claim denied charges?
A1 Claim denied charges. A2 Contractual adjustment. Note: Inactive for version 004060. Use Code 45 with Group Code 'CO' or use another appropriate specific adjustment code. A3 Medicare Secondary Payer liability met. Note: Inactive for 004010, since 6/98.

What are the denial codes?
1 – Denial Code CO 11 – Diagnosis Inconsistent with Procedure. ... 2 – Denial Code CO 27 – Expenses Incurred After the Patient's Coverage was Terminated. ... 3 – Denial Code CO 22 – Coordination of Benefits. ... 4 – Denial Code CO 29 – The Time Limit for Filing Already Expired. ... 5 – Denial Code CO 167 – Diagnosis is Not Covered.
What are remittance advice Remark codes?
Remittance Advice Remark Codes (RARCs) are used to provide additional explanation for an adjustment already described by a Claim Adjustment Reason Code (CARC) or to convey information about remittance processing.
What is denial code CO 183?
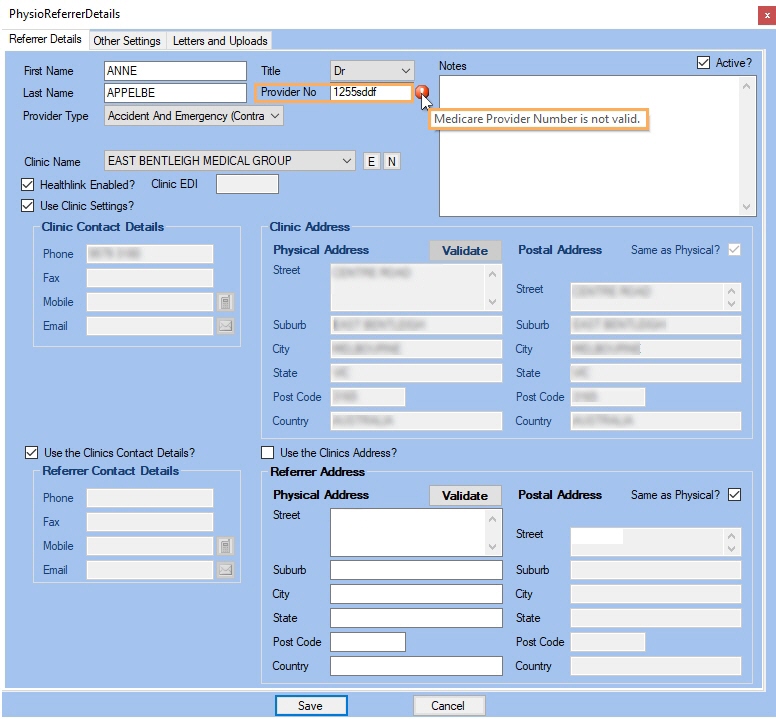
CO-183: The Referring Provider is not eligible to refer the service billed.
How do you fix CO 16?
To resolve this denial, the information will need to be added to the claim and rebilled. For commercial payers, the CO16 can have various meanings. It is primarily used to indicate that some other information is required from the provider before the claim can be processed.
What is a Medicare remittance advice?
The Remittance Advice (RA) contains information about your claim payments that Medicare Administrative Contractors (MACs) send, along with the payments, to providers, physicians, and suppliers. The RA, which may either be in the form of an Electronic Remittance Advice (ERA) or a Standard Paper.
How do you read remittance advice?
1:1228:46How to Read the Remittance Advice - YouTubeYouTubeStart of suggested clipEnd of suggested clipThe basics of a remittance advice is to include the a35 transaction is to communicate the claimMoreThe basics of a remittance advice is to include the a35 transaction is to communicate the claim submitters. The reasons why build services are paid or denied. Both the current paper remit.
What are the top 10 denials in medical billing?
These are the most common healthcare denials your staff should watch out for:#1. Missing Information. You'll trigger a denial if just one required field is accidentally left blank. ... #2. Service Not Covered By Payer. ... #3. Duplicate Claim or Service. ... #4. Service Already Adjudicated. ... #5. Limit For Filing Has Expired.
What does co mean on an EOB?
Contractual ObligationsCO (Contractual Obligations) is the amount between what you billed and the amount allowed by the payer when you are in-network with them. This is the amount that the provider is contractually obligated to adjust off.
What does denial code Co 234 mean?
234. This procedure is not paid separately. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) 1/24/2010. New Codes - RARC.
What does remittance code 16 mean?
Description. Reason Code: 16. Claim/service lacks information or has submission/billing error(s) which is needed for adjudication. Do not use this code for claims attachment(s)/other documentation.
What does co24 mean?
CO 24 – charges are covered under a capitation agreement/managed care plan: This reason code is used when the patient is enrolled in a Medicare Advantage (MA) plan or covered under a capitation agreement. This claim should be submitted to the patient's MA plan.
What does denial code OA 16 mean?
OA 16 Claim/service lacks information which is needed for adjudication. At least one Remark Code must be provided (may be comprised of either the Remittance Advice Remark Code or NCPDP Reject Reason Code.)
When did CMS standardize reason codes?
In 2015 CMS began to standardize the reason codes and statements for certain services. As a result, providers experience more continuity and claim denials are easier to understand.
What does CMS review?
CMS contractors medically review some claims (and prior authorizations) to ensure that payment is billed (or authorization requested) only for services that meet all Medicare rules.
