You will need to accept CMS' license agreement terms before proceeding. Non-Facility Price: Applies to audiology services provided in an office setting and all speech-language pathology services, regardless of setting. Facility Price: Applies only to audiology services provided in a facility, such as a skilled nursing facility.
What is Medicare non facility limiting charge?
· The non-facility rate is the payment rate for services performed in the office. This rate is higher because the physician practice has overhead expenses for performing that service. (Place of service 11) When you submit a claim submit your usual fee. The carrier or MAC processes your claim based on the place of service you select.
What is a non facility fee?
· Description. Under the Medicare Physician Fee schedule (MPFS), some procedures have separate rates for physicians’ services when provided in facility and nonfacility settings. The rate, facility or nonfacility, which a physician service is paid under the MPFS is determined by the Place of service (POS) code that is used to identify the setting where the beneficiary received …
What is a non facility limiting charge?
The non-facility rate is the payment rate for services performed in the office. This rate is higher because the physician practice does have the overhead expense for performing that service. When you submit a claim submit your usual fee. The carrier or MAC processes your claim based on the place of service you select.
Does Medicare cover any of the purchase price?
· A fee schedule is a complete listing of fees used by Medicare to pay doctors or other providers/suppliers. This comprehensive listing of fee maximums is used to reimburse a physician and/or other providers on a fee-for-service basis. CMS develops fee schedules for physicians, ambulance services, clinical laboratory services, and durable medical equipment, …
What is CMS non Facility limiting charge?
A limiting charge is the amount above the Medicare-approved amount that non-participating providers can charge. These providers accept Medicare but do not accept Medicare's approved amount for health care services as full payment.
What is the difference between facility and non facility fees?
In a Facility setting, such as a hospital, the costs of supplies and personnel that assist with services - such as surgical procedures - are borne by the hospital whereas those same costs are borne by the provider of services in a Non Facility setting.
What does facility Price mean?
A facility fee is a charge that you may have to pay when you see a doctor at a clinic that is not owned by that doctor. Facility fees are charged in addition to any other charges for the visit. Facility fees are often charged at clinics that are owned by hospitals to cover the costs of maintaining that facility.
What is a non Facility POS?
The rate, facility or nonfacility, which a physician service is paid under the MPFS is determined by the Place of service (POS) code that is used to identify the setting where the beneficiary received the face-to-face encounter with the physician, nonphysician practitioner (NPP) or other supplier.
What does non-facility Price mean?
The non-facility rate is the payment rate for services performed in the office. This rate is higher because the physician practice has overhead expenses for performing that service. (
What is a Medicare Non-facility?
The non-facility price is when a service is performed in a setting like an office. Some services also have a facility price, which would be when a service is provided in a hospital or an Ambulatory Surgical Center.
Is place of service 10 facility or non facility?
Database (updated September 2021)Place of Service Code(s)Place of Service Name07Tribal 638 Free-standing Facility08Tribal 638 Provider-based Facility09Prison/ Correctional Facility10Telehealth Provided in Patient's Home54 more rows
What is the difference between facility and professional billing?
Date of service: Professional claims allow reporting of a date span, with multiple units on the same claim line. Facility claims require a separate claim line for each date of service. Tip: Never unbundle services on a professional claim; however, report all services on a facility claim (even non-covered services).
Is POS 02 facility or non facility?
The list of settings where a physician's services are paid at the facility rate include: • Telehealth (POS 02); Outpatient Hospital-Off campus (POS code 19); • Inpatient Hospital (POS code 21); • Outpatient Hospital-On campus (POS code 22); • Emergency Room-Hospital (POS code 23);
Is POS 19 a facility or non facility?
According to CMS, reporting the outpatient hospital POS code 19 or 22 is a minimum requirement to trigger the facility payment amount under the PFS when services are provided to a registered outpatient. If the physician/practitioner knows the exact setting where the beneficiary is a registered hospital outpatient.
Is POS 13 facility or non facility?
POS 13 may be used when the place of service is an assisted living facility. This facility is a congregate residential facility with self contained living units. Resident needs an support is provided on a 24/7 basis and some health care is delivered.
Why is the non-facility rate higher?
This rate is higher because the physician practice does have the overhead expense for performing that service. When you submit a claim submit your usual fee. The carrier or MAC processes your claim based on the place of service you select.
What is a managed care organization?
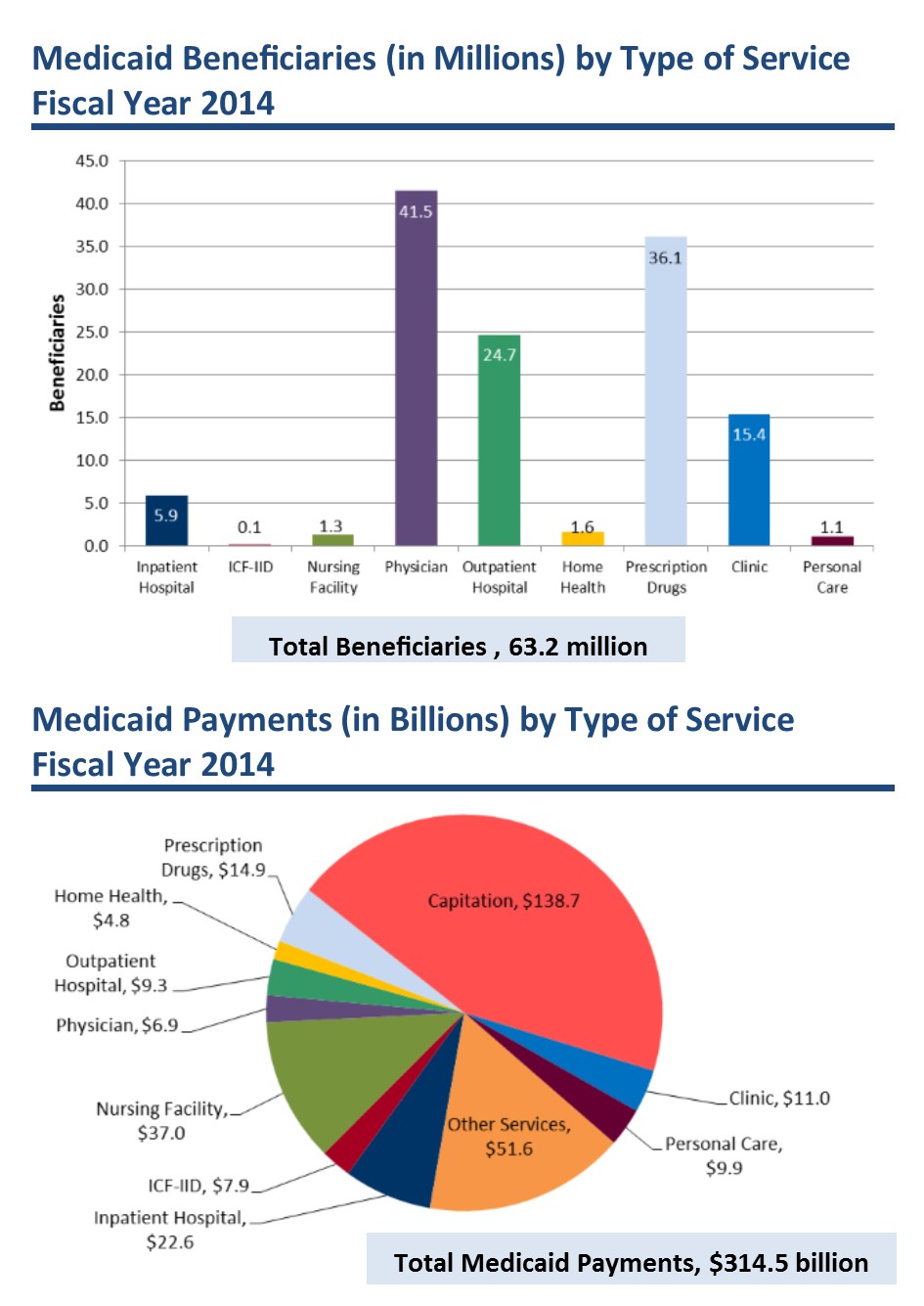
Managed Care Organizations (MCOs) include risk-adjusted plans whose funding is based on the health status of their beneficiaries. Government-funded MCOs use CMS information to search for suspected cases of fraud and abuse.
What is the number 99202-99215?
Due to the extensive changes in office or other outpatient services (99202-99215), there are many questions which still need to be answered, one of which is related to the prolonged services without face-to-face contact.
How is the most appropriate care setting for a given surgical procedure determined?
The decision regarding the most appropriate care setting for a given surgical procedure is determined by the physician based on the patient's individual clinical needs and preferences. Of course, there is a difference in reimbursement, and the billing depends on where the procedure took place, such as an office setting, inpatient ...
Why is the practice expense RVU lower?
This is because the practice does not have the expense for the overhead, staff, equipment and supplies used to perform that service.
Does Medicare have a facility fee?
The Medicare Physician Fee Schedule has values for some CPT® codes that include both a facility and a non-facility fee. The facility fee is typically lower.
What is the role of CMS in quality measures?
It is CMS’ responsibility to ensure that meaningful robust clinical quality measures (CQMs) are available for determination of quality and value of clinical care across all settings. To fully support and help realize the intent of the CMS Quality Strategy, it is critical to ensure that the measures developed are meaningful, represent opportunities for improvement in care quality, and differentiate quality in a meaningful and valid way.
Why is facility input important?
Facility input is a key process to ensure that measures developed and maintained are effective for accountability, for quality improvement, and are useful to healthcare providers . It is also critical that the value added by the measure outweighs the burdens of collecting and reporting the data.
How is MPFS determined?
The rate, facility or nonfacility, that a physician service is paid under the MPFS is determined by the Place of service (POS) code that is used to identify the setting where the beneficiary received the face-to-face encounter with the physician, nonphysician practitioner (NPP) or other supplier.
Does Medicare have separate rates for physicians?
Under the Medicare Physician Fee schedule (MPFS), some procedures have separate rates for physicians’ services when provided in facility and nonfacility settings. The CMS furnishes both rates in the MPFSDB update.
What is the Medicare Physician Fee Schedule?
The Medicare Physician Fee Schedule (MPFS) uses a resource-based relative value system (RBRVS) that assigns a relative value to current procedural terminology (CPT) codes that are developed and copyrighted by the American Medical Association (AMA) with input from representatives of health care professional associations and societies, including ASHA. The relative weighting factor (relative value unit or RVU) is derived from a resource-based relative value scale. The components of the RBRVS for each procedure are the (a) professional component (i.e., work as expressed in the amount of time, technical skill, physical effort, stress, and judgment for the procedure required of physicians and certain other practitioners); (b) technical component (i.e., the practice expense expressed in overhead costs such as assistant's time, equipment, supplies); and (c) professional liability component.
When does non-facility limiting charge apply?
Non-Facility Limiting Charge: Only applies when the provider chooses not to accept assignment.
How to get Medicare fee schedule?
You may request a fee schedule adjusted for your geographic area from the Medicare Administrative Contractor (MAC) that processes your claims. You can also access the rates for geographic areas by going to the CMS Physician Fee Schedule Look-Up website. In general, urban states and areas have payment rates that are 5% to 10% above the national average. Likewise, rural states are lower than the national average.
Can speech therapy be provided at non-facility rates?
Therapy services, such as speech-language pathology services, are allowed at non-facil ity rates in all settings (including facilities) because of a section in the Medicare statute permitting these services to receive non-facility rates regardless of the setting.
Why is Medicare higher for audiologist?
In general, if services are rendered in one's own office, the Medicare fee is higher (i.e., the non-facility rate) because the pratitioner is paying for overhead and equipment costs. Audiologists receive lower rates when services are rendered in a facility because the facility incurs overhead/equipment costs.
When can Medicare change your status?
Your status with Medicare may be changed by informing your contractor of your contracted status for the next calendar year, but only in November of the preceding year.
Do non-participating providers have to file a claim?
Both participating and non-participating providers are required to file the claim to Medicare. As a non-participating provider you are permitted to decide on an individual claim basis whether or not to accept assignment or bill the patient on an unassigned basis.
What is Medicare Administrative Contractor?
The Medicare Administrative Contractor is hereby advised that this constitutes technical direction as defined in your contract. CMS does not construe this as a change to the MAC Statement of Work. The contractor is not obligated to incur costs in excess of the amounts allotted in your contract unless and until specifically authorized by the Contracting Officer. If the contractor considers anything provided, as described above, to be outside the current scope of work, the contractor shall withhold performance on the part(s) in question and immediately notify the Contracting Officer, in writing or by e-mail, and request formal directions regarding continued performance requirements.
When were Medicare payment files issued?
Payment files were issued to contractors based upon the CY 2011 Medicare Physician Fee Schedule (MPFS) Final Rule, released on November 2, 2010, and published in the Federal Register on November 29, 2010, as modified by the Final Rule Correction Notice released on December 30, 2010, and published in the Federal Register on January 11, 2011, and relevant statutory changes applicable January 1, 2011, including the Physician Payment and Therapy Relief Act of 2010 and the Medicare and Medicaid Extenders Act of 2010. This change request amends those payment files.
What does Medicare limit charge mean?
What Does Medicare “Limiting Charges Apply” Mean? Medicare is a commonly used healthcare insurance option. Most people over the age of 65 qualify for Medicare benefits, as well as those with certain disabilities or end-stage renal disease.
What is the limiting charge for Medicare?
This limit cap is known as the limiting charge. Providers that do not fully participate only receive 95 percent of the Medicare-approved amount when Medicare reimburses them for the cost of care. In turn, the provider can charge the patient up to 15 percent more than this reimbursement amount.
What happens if a facility does not accept assignment?
If you decide to seek care from a facility that does not fully accept assignment or does not accept assignment at all, you may be forced to pay more out of pocket. In addition to an extra 15 percent or more, you may also be forced to pay for all of your care out-of-pocket initially.
Can non-participating providers accept assignment?
One possible option for non-participating providers is to choose to accept assignment for some services but to decline assignment for others. For services that they accept assignment for, they are only able to bill the Medicare-approved amount. However, for other services, they are allowed to charge up to 15 percent more than the Medicare-approved amount.
Can Medicare be assigned to other providers?
Other providers may decide not to accept Medicare assignment at all. These providers do not have to abide by any cost-limiting rules put in place by Medicare. Medicare will still reimburse 95 percent of the Medicare-approved amount, but these providers are able to charge any amount they choose for their services.